Common Echo Requests
A number of echo requests crop up commonly, such as ‘Breathlessness ?cause’ and ‘Stroke ?cardiac source of emboli’. This chapter considers some of the requests you will see most often and discusses the key points that you need to consider in each case.
BREATHLESSNESS
Breathlessness is a common symptom that has a multitude of possible causes. In many cases the clinician will want the sonographer to look for evidence of heart failure (systolic or diastolic), but it is important to be alert to a broad range of possible diagnoses as you perform the echo study. Even if you do find evidence of left ventricular (LV) dysfunction, remember that an individual patient can have more than one contributing factor for their symptoms. Common causes of breathlessness are listed below:
Heart failure:
Measure left and right ventricular dimensions.
Assess left and right ventricular systolic function.
Check for LV diastolic dysfunction.
Describe any regional wall motion abnormalities.
Check for associated valvular disease.
Valvular disease:
Assess valvular structure and function.
Assess chamber dimensions and function.
Assess pulmonary artery pressure (if possible).
Ischaemic heart disease:
Are there any regional wall motion abnormalities?
Consider stress echo.
Lung disease:
Assess right ventricular (RV) dimensions and function.
Assess pulmonary artery pressure (if possible).
Is there any evidence of pulmonary embolism?
Remain alert to non-cardiac causes of breathlessness that might nonetheless be detected on echo, such as a pleural effusion (Fig. 25.3, p. 251).
ARRHYTHMIAS
Echo is frequently requested in patients with arrhythmias to check for associated structural heart disease. Although the heart will often prove to be structurally
normal, it is nonetheless important to perform a full echo study as there are several possible abnormalities that may be found. It is helpful to have as much detail as possible about the nature of the arrhythmia to help guide the echo study. An echo is part of the assessment of patients with sustained (or non-sustained) supraventricular or ventricular tachyarrhythmias. It is not usually helpful in those with isolated supraventricular or ventricular ectopic beats, in the absence of any other features.
normal, it is nonetheless important to perform a full echo study as there are several possible abnormalities that may be found. It is helpful to have as much detail as possible about the nature of the arrhythmia to help guide the echo study. An echo is part of the assessment of patients with sustained (or non-sustained) supraventricular or ventricular tachyarrhythmias. It is not usually helpful in those with isolated supraventricular or ventricular ectopic beats, in the absence of any other features.
Atrial fibrillation
Atrial fibrillation (AF) is the commonest sustained arrhythmia, affecting 0.5 per cent of the adult population (and 10 per cent of those aged over 75 years). Many conditions can cause AF (Table 29.1), and an echo may reveal evidence of these, in particular:
valvular heart disease
cardiomyopathy
right heart abnormalities in pulmonary disease or pulmonary embolism
pericardial disease.
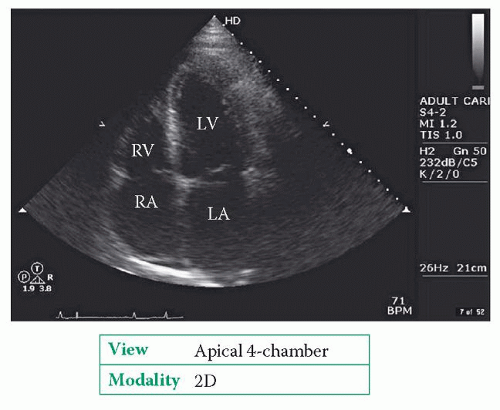
Longstanding AF leads to dilatation of the left and right atria (Fig. 29.1), but be sure to check for other causes of atrial enlargement, such as mitral/tricuspid valve disease or restrictive cardiomyopathy. Atrial enlargement indicates a lower success rate for cardioversion (see below).
Table 29.1 Causes of atrial fibrillation | |||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
AF is a risk factor for embolic stroke and patients at high risk should be considered for anticoagulation with warfarin. Echo indicators of high stroke risk include the presence of valve disease or impaired LV function (clinical indicators include heart failure, previous stroke/transient ischaemic attack (TIA) or peripheral embolic events, or, in those aged 75 years or over, the presence of hypertension, diabetes or vascular disease).
Cardioversion of persistent AF back to sinus rhythm should be considered in patients where the procedure is likely to succeed (and sinus rhythm maintained in the longer term). The presence of structural heart disease on echo (such as a left atrium (LA) >5.5 cm or mitral stenosis) suggests a lower likelihood of successful cardioversion.
If cardioversion is going to be undertaken for a patient who has been in AF for longer than 48 h, it is important to minimize the risk of embolism either by arranging therapeutic anticoagulation for at least 3 weeks prior to the cardioversion, or by performing a transoesophageal echo (TOE) to rule out intracardiac thrombus – this is called TOE-guided cardioversion. If there is no thrombus present, the cardioversion is normally carried out with heparin cover, and the patient treated with warfarin for 4 weeks afterwards.
Ventricular arrhythmias
Ventricular tachycardia and/or fibrillation commonly result from underlying structural heart disease. Echo is therefore part of the assessment of patients who have had, or are regarded as being at high risk of, ventricular arrhythmias, looking in particular for evidence of:
myocardial infarction/ischaemia
valvular heart disease (in particular, mitral valve prolapse)
cardiomyopathy (e.g. hypertrophic cardiomyopathy, dilated cardiomyopathy, arrhythmogenic RV cardiomyopathy).
A full assessment of both LV and RV dimensions, morphology and function is required. If myocardial ischaemia is suspected, a stress echo study may be required (Chapter 8).
EJECTION SYSTOLIC MURMUR
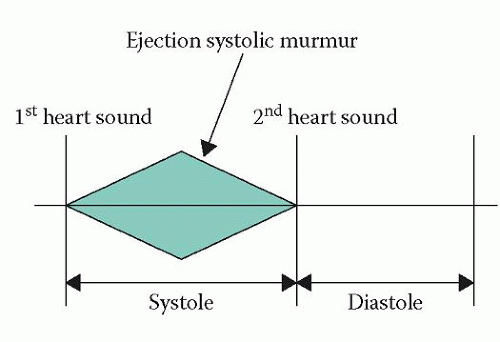
An ejection systolic murmur begins after the first heart sound, rises in intensity to reach a peak during systole, and then falls in intensity to end before the second heart sound (Fig. 29.2). The murmur is also described as ‘diamond-shaped’ or ‘crescendodecrescendo’.
Causes of an ejection systolic murmur include:
aortic stenosis
bicuspid aortic valve
pulmonary stenosis
hypertrophic obstructive cardiomyopathy.
Remember that aortic and pulmonary stenosis can occur not just at the valve but also with obstruction to outflow at a subvalvular or supravalvular level.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree