Coal Workers’ Lung Diseases and Silicosis
COAL WORKERS’ LUNG DISEASES
Coal miners are at risk for developing several distinct clinical illnesses in relation to their occupational exposures. Historically, some names applied to these conditions were miners’ asthma, phthisis, anthracosis, and in Scotland, miners’ black lung. It was recognized early that these afflictions were related to the occupation of mining; however, it was not until the development of specialized techniques such as chest radiography, pulmonary function testing, the discovery of the tubercle bacillus, and sophisticated histologic examination of tissue that respiratory diseases affecting miners could be separated and defined. Recent advances in the understanding of respiratory health issues in coal miners have focused on the spectrum of disease caused by inhalation of coal mine dust, termed coal mine dust lung disease (CMDLD).1
CMDLD includes the classic occupational interstitial lung diseases, such as coal worker’s pneumoconiosis (CWP), silicosis, and mixed dust pneumoconiosis, but also includes the more recently described entity labeled dust-related diffuse fibrosis (DDF).1 CMDLD is a preventable occupational disease that results from inhalation of coal mine dust into the lungs leading to parenchymal and airway damage, not only from the foreign material itself but also the tissue’s reaction to the dust.1,2 This disease process was identified as early as the 1800s, but became much more prevalent as coal production increased during the industrial revolution. Unfortunately, disability from coal mine dust exposure went mostly unrecognized by medical authorities in the United States through the first part of the 20th century. Congress finally passed comprehensive legislation with the Federal Coal Mine Health and Safety Act of 1969. This Act went above and beyond previous legislation by providing for the first mandatory standards for working conditions in US mines, a system for enforcement, and ongoing monitoring of miner health, as well as a mechanism for seeking financial compensation for coal miners who could demonstrate total disability arising from their dust exposure (aka “black lung”).3
Since the time of this landmark legislation further acts by Congress and enforcement agencies have improved miners’ working conditions, which now fall under the purview of the Mine Safety and Health Administration (MSHA). Much of our improved understanding of the nature and extent of lung disease associated with mining coal in the United States over the past half century comes from the large number of studies performed by the National Institute for Occupational Safety and Health (NIOSH). Despite increased understanding of CWP and reports of stable or improved dust levels in mines, dust-related respiratory disease remains a significant burden. Most worrisome are recent data suggesting that contemporary dust exposure is leading to rapidly progressive pneumoconiosis particularly in young miners, with a significant impact on pulmonary function and premature death.4
 COAL AND COAL MINING
COAL AND COAL MINING
Coal is not a pure mineral. It is a spectrum of carbonaceous rocks derived from the accumulation of vegetation sedimented under swampy conditions and subjected to extreme pressure over long periods of time. Coals are characterized by rank, which relates to geologic age, hardness, carbon content, and the amount of heat released (BTUs) when they are burned. Thus, peat is the lowest rank (softest) coal, being geologically the newest, and anthracite is the highest rank (hardest) and oldest type of coal.
Coal may be found in outcroppings and in seams that vary from a few feet to several thousand feet below the surface. Surface or strip mining, which currently accounts for the majority of US coal production, involves removal of the overburden and mining the coal seams with large earth-moving equipment. In some areas of the eastern United States, mountaintop removal mining has become a dominant form of mining. Mountaintop mining involves first removal of all vegetation and soil, and then drilling and blasting through hundreds of feet of strata to access the coal seam. The excess rock and soil is placed in the steep stream beds along the mountainsides, creating areas called valley fills. Occasionally, surface mining is also performed by boring into coal outcrops with an auger. Dust levels measured in the air at surface mines have generally been lower than in underground mines, with a few notable exceptions, but miners who work exclusively at surface operations may still develop advanced forms of pneumoconiosis (discussed below).5,6 Coal outcrops of sufficient size can be mined deep into the hillsides. Deep seams are accessed through vertical shafts drilled from the surface to the coal seam where the mining process then follows the seam through a series of more or less horizontal tunnels. Shaft drilling, which is frequently performed under contract for mine operators, may present an important silicosis hazard. A majority of the approximately 92,000 coal miners in the US work at underground mines,3 although deep mines produce somewhat less than half of the coal mined; in China, there are about six million underground miners.1
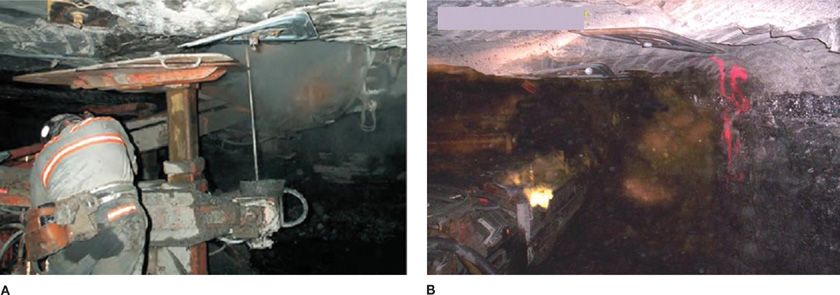
Respirable dust concentration, coal rank, types of mining work, mining category, and duration of exposure are known risk factors for the development of pneumoconiosis.7 Dust exposure varies significantly between specific tasks within the mines. In underground mining, airborne dust is generally highest during work at the coal-cutting face, where coal is removed from intact seams. Miners involved in roof support (termed roof bolters; see Fig. 88-1), miners who do not use protective respiratory equipment, workers exposed to explosive blasting fumes, and those who use stored mine water for dust suppression spray are all at increased risk for accelerated loss of lung function.8
Figure 88-1 Photographs illustrating underground coal mining. In (A), miner is engaged in drilling before placing a roof bolt. In (B), the gray area above the black coal seam indicates where the mining equipment has pulverized a layer of silica-bearing rock. (Used with permission of Anita Wolfe, National Institute for Occupational Safety and Health, Morgantown, WV.)
Many miners also have exposure to respirable crystalline silica, placing them at risk for silicosis and or concurrent CWP/silicosis.9 In particular, silicosis has been recognized among miners performing roof bolting, and drilling operations, as well as motormen who operate underground coal trains and use sand for traction on the rails.10,11 Workers in some aboveground coal mining operations also may have important exposure to dusts.5,12 These include workers at tipples and preparation plants, where crushing, sizing, washing, and blending of coal is done, and coal is stored or loaded onto ships, railroad cars, or river barges. At surface coal mines, drilling rigs are used to bore holes in which explosives are placed. Equipment operators may be exposed to silica and silicate dusts from the rock strata, representing a risk for silicosis or mixed dust pneumoconiosis, rather than CWP (Fig. 88-1).
 EPIDEMIOLOGY OF LUNG DISEASES IN US COAL MINERS
EPIDEMIOLOGY OF LUNG DISEASES IN US COAL MINERS
The first major survey of the health of American coal workers was conducted by the US Public Health Service from 1969 to 1971, evaluating symptoms, lung function, and chest radiographic findings. This study included over 9000 miners at 31 underground mines (2 were anthracite mines; 29 were bituminous mines). Participation in the survey was over 90%. The mines were chosen to represent different geographic areas, coal seams, and mining methods. After this initial study, three subsequent surveys have been conducted to evaluate miners at these and other US mines.
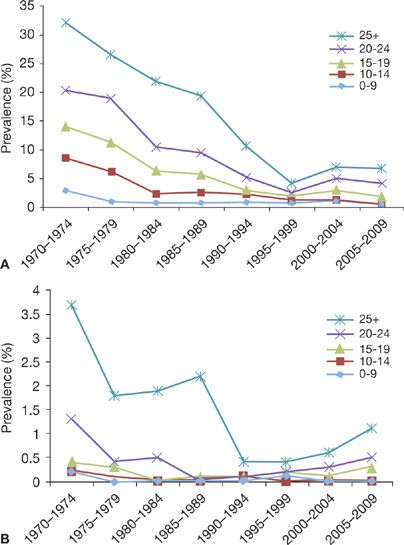
Results of radiographic surveillance from the 1970s through the mid-1990s showed a marked decline in the prevalence of CMDLD.13,14 The decreased prevalence was a source of great optimism that government regulations and oversight was resulting in improvement in miners’ respiratory health. Unfortunately the decline has not continued. Since about 1995, the observed prevalence of CMDLD among miners who participate in health surveillance has been increasing (see Fig. 88-2B.15 In response to this troubling finding, availability of health surveillance for miners was increased. When data from underground miner health surveillance are compared to reported dust measurements, CWP prevalence is less than expected in some regions but substantially greater than expected in others, with some miners experiencing rapid progression of disease.16
Figure 88-2 Proportion of miners examined in the NIOSH Coal Workers’ X-ray Surveillance Program from 1970–2009 with Coal Workers’ Pneumoconiosis category 1 or greater (A) or progressive massive fibrosis (B), by tenure in underground coal mining. (Adapted with permission from Attfield MD. Centers for Disease Control and Prevention: Current Intelligence Bulletin 64: Coal Mine Dust Exposures and Associated Health Outcomes—A Review of Information Published Since 1995. DHHS(NIOSH) Publication No. 2011–172; 2011. Available from: http://www.cdc.gov/niosh/docs/2011–172.)
 RADIOGRAPHIC FINDINGS
RADIOGRAPHIC FINDINGS
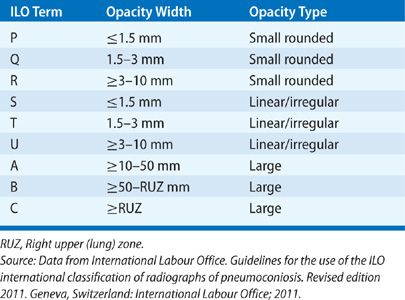
Radiographic epidemiologic studies and surveillance findings for underground coal miners have been reported over the last four decades. As part of these activities, each miner’s chest radiograph is independently interpreted by at least two qualified physicians, using the International Labour Office (ILO) pneumoconiosis classification system (see Table 88-1 for the definition of ILO terminology).17 Radiographic data from the initial health surveys showed an overall prevalence of simple and complicated CWP of nearly 30%. There was variation in prevalence by region of the country and the type (rank) of coal mined.18 Enforcement of dust control measures in the United States, fully enacted in 1973, resulted in a declining pneumoconiosis attack rate. This decreased prevalence was confirmed through the federally mandated chest radiographic surveillance program for underground US miners.13,14 Between 1973 and 1978, CWP was found in about one-third of the miners who participated in the program and had worked 25 years or more underground.14 By 1995 to 1999, only 1 in 25 (4.2%) of these miners showed radiographic evidence of CWP (Table 2011 to 2012 in reference 14).
TABLE 88-1 Definitions of Terminology Used by the International Labour Office Classification to Describe Pneumoconiotic Opacities
Regrettably, continued surveillance by NIOSH has revealed a significant increase in the prevalence of radiographic pneumoconiosis (to 7%) in 2005 to 2009 for miners with more than 25 years tenure, since hitting its nadir in the late 1990s.14 The rate of progressive massive fibrosis (PMF) has also tripled to 1.1% after reaching its low point over a decade ago.18 Also of interest is the elevated disease prevalence among workers at smaller mines.19
Perhaps the most concerning findings of ongoing surveillance studies have been the frequency of rapidly progressive radiographic disease in certain mining populations. During their 2005 analysis, Antao et al. found that in miners with pneumoconiosis, about 35% had rapidly progressive disease. This rapid progression was defined as an increase of greater than one ILO subcategory over 5 years.16 More worrisome is the fact that 15% developed PMF, the most advanced and debilitating form of the disease. Current studies are now underway to assess the reason(s) for this rapidly progressive form of CMDLD.
Radiographic analysis has been complemented by ventilatory lung function testing as an integral component of respiratory health studies of the mining population. Early reports strived to identify a relationship between radiographic disease and spirometry results. Multiple studies in the United States and abroad have subsequently evaluated the relationship between radiographically evident CMDLD and lung function.20–22 Although several earlier studies did not associate lung function impairment with uncomplicated CWP, recent analysis has identified significant ventilatory deficits among coal miners with small radiographic opacities, in addition to the important decrements in lung function that have been observed in miners with the large radiographic shadows (>10 mm) of PMF.4,22,23
Studies in the United States and Great Britain evaluated lung function with respect to the miners’ cumulative dust exposure, and have helped to clarify the adverse effect of dust on coal miners’ lung function.24–26 Miners show a progressively greater risk of lung function loss with increasing cumulative dust exposure, independent of the chest radiographic findings of CWP. The forced expiratory volume in 1 second (FEV1) loss is most severe in those who work for many years at the dustiest jobs. Among smoking miners, the effects of tobacco smoke appear to be additive and of similar magnitude to the dust effect. Studies of FEV1 decline have demonstrated essential equivalence between 1 year of work in a job at the coal face and 1 year of cigarette smoking: no disproportionate dust effect has been noted in relation to tobacco use. Also, there is evidence that miners experience a more rapid loss in spirometric function parameters during their first few years of mining, with slower dust-related declines after that time.27
In summary, the epidemiologic evidence has shown that coal miners experience ventilatory lung function loss with increasing exposure to dust, either in the presence or absence of radiographic CWP. Among smoking miners, the effects of tobacco and dust appear to be additive. Although, on average, the functional losses associated with either dust or smoking are small, it is estimated that after 35 years of work at the current permissible limit, dust exposures will cause a clinically important FEV1 loss in 8 out of 100 nonsmoking coal miners. Higher exposures result in greater losses. When chronic bronchitis is present, there is an additional FEV1 reduction averaging 200 to 250 mL.7,27 With simple CWP, and especially when PMF is present, an additional ventilatory deficit is likely.
Investigations into miner mortality have been completed in both the United States and Britain. Findings from both countries have been generally consistent, and reveal that the miners experience increased mortality attributable to pneumoconiosis, emphysema, chronic bronchitis, and ischemic heart disease.28–33 Radiographic findings of advanced CWP (PMF) consistently affect mortality, especially in categories B and C (see Table 88-1 for definition of ILO terminology) whereas among miners with simple CWP, decreases in survival were smaller. Accelerated FEV1 decline is also associated with increased mortality from both cardiovascular and respiratory causes.30 Miners’ risks of dying from the obstructive airway diseases of emphysema and chronic bronchitis exhibit a different geographic pattern than the mortality from CWP, suggesting that these dust effects have different mechanisms.31 Attfield and Kuempel32 analyzed the mortality experience over 22 to 24 years among 8899 working coal miners. Their results revealed increased mortality from nonviolent causes, nonmalignant respiratory disease, and accidents, and confirmed previous results indicating that exposure to coal mine dust leads to increased mortality in the absence of tobacco smoke exposure.
Troubling recent data regarding miners with both rapidly declining lung function and rapid progression of radiographic disease seem to have also had mortality implications. A NIOSH report from 2009 revealed a substantial increase after 2006 in years of potential life lost (YPLL) before age 65 years associated with CWP.2 A recent study looked at data over the past decade (at current exposure levels). Investigators found rapidly progressive pneumoconiosis and massive fibrosis in relatively young West Virginia coal miners that led not only to important lung dysfunction but also premature death.4 More documentation for the high risk of contemporary coal mine exposures comes from investigations into mining accidents. Lung tissue analysis was performed on 24 victims of a recent mine explosion. Seventy-one percent (17/24) had autopsy evidence of CMDLD and 16 of the 17 miners with CWP had started working after the modern dust limits were put into effect.34 The implications of these new studies are incompletely understood, but it is obvious that contemporary miners are still developing severe and fatal CMDLD.
 PATHOLOGY OF COAL MINERS’ LUNG DISEASES
PATHOLOGY OF COAL MINERS’ LUNG DISEASES
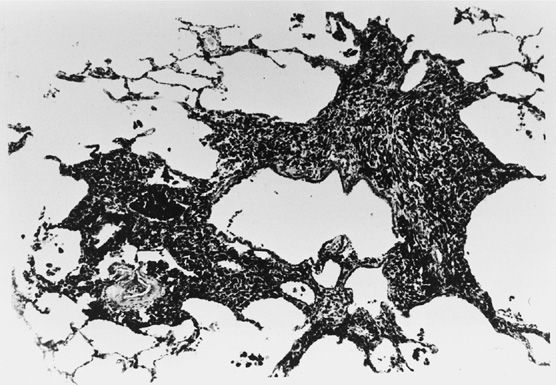
Heppleston35 identified the coal macule as a fundamental histopathologic finding in CMDLD in 1953 (Fig. 88-3). In his discussion he described the macule as consisting of a focal collection of coal dust in pigment-laden macrophages around the respiratory bronchioles and tapering off toward the alveolar duct. A fine network of reticulin is present in the early stages and may include a small amount of collagen depending upon the character of the dust.36 Centriacinar emphysema, the dilation and injury of lung gas exchange units, is observed with increased prevalence in the lungs of coal miners. Focal emphysema is the form of centriacinar emphysema that is seen as an integral part of the lesion of simple CWP. It is characterized by enlargement of the airspaces immediately adjacent to the dust macule. The pathologic severity of the emphysema is proportional to the miner’s cumulative dust exposure and increases with increasing lung dust retention.37–39 Muscular thickening of pulmonary arteries, in conjunction with hypertrophy of the right ventricle, can be observed with both simple and complicated CWP, and is increasingly prominent when CWP is associated with other lung disorders.40 The development of pulmonary hypertension secondary to these changes may have a profound adverse effect on miner mortality.41 Pathologic changes in the airways consistent with chronic bronchitis, including enlargement of mucus glands, have also been documented in miners’ lungs.42
Figure 88-3 A coal macule, microscopic section. (Used with permission of Dr. Val Vallyathan, National Institute for Occupational Safety and Health, Morgantown, WV.)
Central to the biology of CMDLD (discussed below) is the alveolar macrophage.43–45 Dust particles that travel to the distal airways (beyond the mucociliary escalator) are engulfed by alveolar macrophages and removed from the airways and lung parenchyma via lymphatics. With extended excessive dust exposure, this system is overwhelmed and coal mine dusts as well as dust-laden macrophages begin to accumulate in the airway walls and interstitium. Recent evidence suggests that important lung functional losses observed during coal mining work may at least in part be related to this dust reaction in the small airways.46 With ongoing dust deposition and inadequate clearance mechanisms, these lung lesions increase in size and number. These larger fibrotic lesions are called coal nodules and are palpable in lung specimens, whereas coal macules are not. Palpable coal nodules are classified as micronodular up to 7 mm in diameter and macronodular from 7 mm and larger.47
A less common form of CMDLD and silicosis labeled DDF has been increasingly recognized. This finding had previously been interpreted as representing the development of usual interstitial pneumonitis (UIP) in miners. Recognition of a pulmonary fibrosis pattern related to CMDLD has been supported by case reports and several studies.48–50 In their position paper the Industrial Injuries Advisory Council (IIAC) found “there is good evidence for a form of interstitial fibrosis which is really part of the disease process of CWP and is not typical of cases of interstitial fibrosis in noncoal workers.” DDF has been described in pathologic terms as a bridging fibrosis connecting various stages of CMDLD lesions and/or lesions of silicosis, and has been found in approximately 12% of coal miners at autopsy.50 An occupational history is of utmost importance to the proper clinical recognition of DDF as opposed to UIP.1 This distinction is of importance both from a prognostic and management standpoint.
At autopsy, complicated CWP (PMF) is confirmed when one or more nodules in a lung specimen are noted to attain a size of 2 cm or greater in diameter.47 The 2 cm is an arbitrary choice of a minimal diameter that permits better correlation with clinical and radiographic measurements. (In fact, when radiographic pneumoconiotic shadows are >1 cm, PMF is said to be present.) Lesions are solid, heavily pigmented, and rubbery to hard. They tend to occur symmetrically, but may be asymmetrical, and may cavitate.51,52 Airways and vessels adjacent to the lesions may be distorted, and within the lesions, they are destroyed. PMF generally occurs in association with background pathologic changes of simple CWP.53
 BIOLOGY OF COAL WORKERS’ PNEUMOCONIOSIS
BIOLOGY OF COAL WORKERS’ PNEUMOCONIOSIS
Numerous studies have evaluated the relationship of coal mine dust exposure and activation of immunologic and inflammatory mechanisms. Soutar et al.54 reported a study of serum antinuclear antibodies (ANA) and rheumatoid factor (RF) among 109 miners with radiographic evidence of pneumoconiosis attending the London Pneumoconiosis Panel. They reported positive ANA in 17% and RF in 10% of the miners whereas about 2% to 3% positive ANA was expected in a healthy male population. The prevalence of ANA was 9% in simple CWP and 27% in those with category C (PMF). A similar trend was seen with RF, ranging from 6% in simple CWP to 18% in category C. Combining both ANA and RF resulted in prevalences of positive results in 13% of the miners with simple CWP and 45% of those with category C CWP.
Studies of serum immunoglobulins were conducted by Hahon et al.55 among 155 US coal miners with chest radiographs demonstrating simple CWP, Caplan syndrome (an atypical clinical presentation of pneumoconiosis associated with features of rheumatoid arthritis), or PMF. Among miners with PMF, those mining anthracite coal had significantly higher serum concentrations of C3, α1-antitrypsin, IgA, and IgG compared to miners from bituminous regions. Compared to normal controls, the miners had elevated C3, α1-antitrypsin, and IgG values. There were few differences in these serum proteins among the miners with simple CWP. The authors did not find any association between the elevated immunoglobulins and FEV1.
Over the past decade much research has been undertaken to understand the mechanism(s) of coal mine dust–induced inflammation. Compared to controls, miners with CMDLD have been shown to have elevations in both serum and bronchoalveolar lavage (BAL) of several cytokines, which play an important role in lung inflammation and fibrosis, including IL-1β, IL-6, and TNF-α.56,57 Inflammation resulting from oxidative stress has also been suggested in both human and animal data.58,59 One potential contributor to miners’ increased oxidative stress is the level of bioavailable iron. Iron has the known potential to catalyze oxidant formation through its interaction with oxygen or hydrogen peroxide. The potential of bioavailable iron to induce oxidative stress has been associated ecologically with regional variations of CMDLD prevalence.60
Although immunomodulation and inflammation play an important role in the development of CMDLD, the underlying host susceptibilities that lead one miner to develop severe disease in a given environment while another miner may have a relatively minimal disease burden remain elusive. Genetic studies have been unable to identify specific markers of susceptibility to CMDLD, although one study suggested certain polymorphisms of IL-18 may be protective.61–63 Continued studies on the mechanisms of CMDLD and understanding of disease susceptibility are important, given recent trends in CMDLD epidemiology.
 CLINICAL FEATURES OF COAL WORKERS’ LUNG DISEASES
CLINICAL FEATURES OF COAL WORKERS’ LUNG DISEASES
Reflecting the diverse lung pathology associated with coal mine dust exposure, it is not surprising that the clinical presentation of the disease may be quite variable. Miners with simple CWP, perhaps detected through a screening radiograph, may deny significant respiratory symptoms. With increased dust exposures, chronic cough and sputum production are more common, regardless of the presence or absence of simple pneumoconiosis.64 These symptoms are likely related to bronchitic changes in the large airways, including thickening of the airway wall with mucus gland enlargement and hypersecretion that result from continued inhalation of dust particles presenting a chronic burden to the mucociliary escalator.42,65 A study by Henneberger and Attfield66 reported symptoms of chronic bronchitis in 35% of seasoned US miners.
Emphysema has been shown to be more common in miners than nonminers, even after controlling for smoking status, and increases with increasing cumulative dust exposure.37 As would be expected, with more severe airflow obstruction or advanced pneumoconiosis, dyspnea, cough, and sputum production are frequent. The physiologic importance of the small airway lesions from dust exposure has been debated. A pathologic label of mineral dust-related airway disease has been used to describe a lesion of pigmentation and fibrosis specific to walls of the respiratory bronchioles among workers exposed to mineral dusts.67
Less commonly, edema of the lower extremities, and findings consistent with cor pulmonale/pulmonary hypertension may occur.40,41,68 An exceedingly rare but unique clinical manifestation of CMDLD is melanoptysis (expectoration of black sputum). Melanoptysis may be a very worrisome symptom for patients, but is the harmless result of excavation and liquefaction of a PMF lesion.69
Clubbing and crackles have not generally been considered features of coal miners’ lung diseases, and if noted, should prompt further studies. However, a series of 38 cases of a chronic interstitial pneumonia among coal miners has recently been reported. The clinical findings in these atypical cases included crackles, finger clubbing, restrictive impairment, diffusion block, and neutrophilic BAL.70 Studies have not associated CWP with an increased risk for development of coexisting mycobacterial infection, in contrast to silicosis, where the risk is well documented. However, in a minority of coal miners, the lungs show classic silicotic nodules.71 Certainly, coal miners with progressive infiltrates or cavitary lesions in PMF should undergo thorough sputum examination for typical and atypical mycobacteria.72
 RADIOLOGY OF COAL WORKERS’ PNEUMOCONIOSIS
RADIOLOGY OF COAL WORKERS’ PNEUMOCONIOSIS
The diagnosis of CWP can be made with confidence based on the classic radiographic findings and the presence of an adequate history (at least 10 years) of coal mine dust exposure without the need for histological confirmation.1 The radiographic opacities of CMDLD have been well described and are classified according to the ILO system.17 This system includes a set of standard radiographs, which can facilitate an accurate and consistent approach to recognizing and categorizing the radiographic changes associated with dust exposure. Traditionally analog chest films were used in the classification scheme. This practice changed in 2011 to include classification of digitally acquired images on a high-resolution medical viewing system.73 Digital systems can provide equivalent results in the recognition and classification of the pneumoconioses, when applied according to professional recommendations.73,74 The radiograph in simple pneumoconiosis shows small pneumoconiotic opacities, ranging in size from pinhead up to 9 mm in diameter. In a study of working US coal miners with radiographic small opacities, 62% showed mainly rounded small opacities while 38% had predominantly irregular opacities.75 Irregular opacities were more common in lower lung zones. PMF is characterized by one or more opacities in the lung fields greater than 1 cm. Complicated pneumoconiosis is more commonly seen in the upper lung zones, but is confined to the middle and/or lower zones in about one-fourth of cases.76,77 Although there are some limitations to the use of standard posteroanterior CXR in the diagnosis of simple CWP and of PMF, standard radiographic evaluation of CMDLD remains important for diagnosis, surveillance, compensation, and disease prevention.78
Computed tomography (CT) scanning in coal miners may reveal parenchymal nodules and emphysema when standard radiographs are normal.79,80 In atypical cases, CT scans may show ground-glass opacities and honeycombing, at times without nodular findings typical of CWP.70 Radiographic evidence of bronchiectasis has also been reported in coal miners, particularly among those with CWP.81 CT scanning is currently not recommended in the surveillance of exposed miners, but is likely of use in symptomatic miners with normal plain chest radiography or in miners where alternate diagnoses are being considered.82 A proposed pneumoconiosis classification scheme for CT has shown good reliability, but has yet to be widely adopted.83
Several schemes have been used for classifying the radiographic shadows of pneumoconiosis in epidemiologic studies; currently the ILO 2011 Classification of Radiographs of the Pneumoconioses is the most widely accepted (Table 88-1).17 When using the ILO system, simple pneumoconiosis is divided into major categories 0, 1, 2, and 3 according to the profusion of small opacities (number per unit area) in the lung fields. Each major category, including 0, is subdivided into 3 subcategories, providing a full range of 12 categories of simple CWP. A reading of category 1/0 indicates the definite presence of opacities consistent with pneumoconiosis. Complicated pneumoconiosis (PMF) is divided into categories A, B, and C, based on the size of the large opacities. The classification also permits documentations of other findings that may be associated with the shadows of simple or complicated pneumoconiosis, such as tuberculosis, cor pulmonale, collapse, consolidation, and emphysema. A system of training and examinations (http://www.cdc.gov/niosh/topics/chestradiography/breader-info.html) is available for physicians who wish to document competence in application of the ILO Classification.
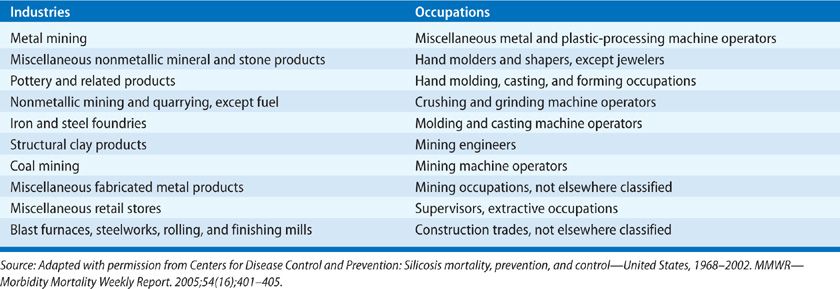
TABLE 88-2 Top 10 Industries and Occupations with Significantly Elevated Proportionate Mortality Ratios for Silicosis, 26 States, 1985–1999. CDC/NIOSH National Occupational Respiratory Mortality System
The clinician may be presented with the diagnostic dilemma of distinguishing primary or metastatic lung neoplasia from an unusual presentation of PMF or Caplan syndrome. When typical large opacities of PMF occur symmetrically and bilaterally on a background of simple CWP, one can be confident that the lesions are unlikely to represent neoplastic disease. Prior radiographs from medical screening programs are often obtainable, and can help confirm stability or progression over a long time interval. Positron emission tomography with fluorodeoxyglucose (FDG-PET) scanning may be useful in differentiating PMF lesions from malignancy when the mass lesion has a low level of glucose metabolism, although some massive pneumoconiotic lesions may demonstrate an uptake of fluorodeoxyglucose similar to neoplasms.84 On magnetic resonance imaging (MRI) with contrast enhancement, the pattern of change over time in signal intensity has been reported to be a differential criterion in this setting.84,85 When the imaging workup is equivocal, the differentiation of PMF from neoplasm may be impossible without a biopsy. In this case, patients with CMDLD who are deemed potential candidates for therapy should undergo biopsy of the suspicious lesion. Hemorrhagic complications may occur during biopsy of PMF lesions due to their vascular nature.
 LUNG FUNCTION AND RESPIRATORY IMPAIRMENT IN COAL MINERS
LUNG FUNCTION AND RESPIRATORY IMPAIRMENT IN COAL MINERS
As discussed earlier, CMDLD encompasses a spectrum of diseases caused by inhalation of coal mine dust that results in several pathologic processes (simple and complicated CWP, silicosis, DDF, chronic bronchitis, mineral dust airway disease, emphysema, and dust-related airflow limitation), each of which may contribute to adverse physiologic consequences. In an individual miner, the pattern and severity of impairment found will be related to such recognized factors as the intensity and duration of respirable dust exposure, geologic factors (e.g., coal rank, silica content), residence time of dust in the lung, and exposure to other respiratory hazards (e.g., tobacco smoke).7,8,20–27,31 In miners with airway hyperresponsiveness, greater functional deficits and an increased risk of symptoms may be expected.86,87 Several other mining exposures may also contribute to lung function loss in coal miners, including gases from underground explosive blasting and aerosols of potentially contaminated water used for dust control.8 Additional factors implicated in underground coal miners’ accelerated lung function declines include weight gain, childhood pneumonia, and childhood environmental smoke exposures.8
Ventilatory Function
As CMDLD can manifest pathologically as disease of the lung parenchyma, small airways, and/or large airways, the corresponding physiologic defects appreciated on lung function testing may include obstructive, restrictive, or mixed defects.46,88 The predominant functional abnormality in a given exposed miner will depend on the relative contribution of emphysema, airway disease, and fibrosis in the individual. Epidemiologic studies, as discussed earlier, have extensively documented the occurrence of exposure-related deficits in FEV1 and forced vital capacity (FVC) in coal miners.7,24–27,89,90 Although the magnitude of dust-related decline has varied between studies, an important subgroup of miners with accelerated decrements in lung function (FEV1 decrease of >60 mL/y) has been identified. These miners were found to have more chest illnesses, respiratory symptoms, and a greater risk of death from cardiovascular or nonmalignant respiratory disease than were their cohorts with more stable lung function.30 Airflow obstruction developing during coal mining has been associated with physiologic evidence of increased resistance to airflow in small (<2 mm internal diameter) airways, including abnormal airflow at low lung volumes and reduced density dependence of maximum expiratory flows.46 Not surprisingly, deficits in lung function have also been documented in US surface coal miners.15
Gas Exchange
Diffusing capacity has been studied in relation to radiographic changes of coal worker’s pneumoconiosis.90–92 The small rounded opacities seen in miners with simple CWP have not generally been associated with measurable reductions in diffusion capacity, and large opacities of complicated CWP are not predictably associated with decreased diffusion. In contrast, miners with irregular opacities may have significant impairment in diffusion capacity, and abnormalities of gas exchange have been associated with increasing coal mine dust exposure independent of radiographic changes. Investigators have demonstrated a significant correlation between subjective measures of breathlessness and measurements of diffusion capacity, which may not be consistently observed with other pulmonary function parameters including FEV1.91 Gas exchange on exercise has also been investigated in coal miners.40,41,93–95 Many reports have been based on patients referred for disability evaluations, and thus suffer from ill-defined selection biases. Exposure–response relationships are also unclear with respect to findings in these series. Exertional hypoxia, pulmonary arterial hypertension, and excess ventilation have frequently been observed in miners, particularly those with complicated CWP or airflow obstruction.1 However, the proportion of miners who show exertional gas exchange abnormalities in the absence of either PMF or clinically important airflow obstruction is still a topic of investigation.
 SPECIAL STUDIES
SPECIAL STUDIES
BAL has been used in studying pathogenetic mechanisms in the pulmonary pathology in CWP. Rom et al.96 reported BAL results for 15 symptomatic, nonsmoking coal miners with simple CWP. They found no significant difference between miners and controls in the number of cells recovered, the percentage distribution, and in the release of superoxide anion or hydrogen peroxide. This contrasted with the findings in subjects with asbestosis and silicosis, whose values for spontaneous release of superoxide and hydrogen peroxide were significantly higher than controls. With regard to fibronectin and alveolar macrophage–derived growth factor, the miners with CWP had values that were elevated above controls and not different from the values obtained in subjects with asbestosis and silicosis.
Wallaert et al.44 demonstrated significantly increased total number of lung cells recovered from 25 miners with simple and complicated CWP, as well as increased percentages of alveolar macrophages, lymphocytes, and neutrophils. Alveolar cells from miners with simple and complicated CWP spontaneously released significantly more superoxide, demonstrated by chemiluminescence, than controls.
 MANAGEMENT OF COAL WORKERS’ LUNG DISEASES
MANAGEMENT OF COAL WORKERS’ LUNG DISEASES
There is no specific therapy for CMDLD. Whole lung lavage has been evaluated, but studies to date have not adequately defined the risks, benefits, and role in CMDLD management.97 Thus, the crux of management is directed toward prevention, early recognition, and treatment of complications. The major clinical challenges are the recognition and management of airflow obstruction, respiratory infection, hypoxemia, respiratory failure, cor pulmonale, arrhythmias, and pneumothorax.
After implementation of the current mandated permissible exposure limit (PEL) of 2 milligrams per cubic meter (mg/m3) of respirable coal mine dust and improvements in mine dust control methods, the prevalence of CMDLD appeared to have been decreasing.14 The recent epidemiologic findings of significantly increasing prevalence and rapid progression to severe disease in CMDLD should motivate workers to assure continuous control of dust, participate in medical surveillance programs, and exercise their rights to frequent dust measurements and job transfer when necessary. Previous surveillance programs have monitored worker lung health with chest radiographs every 5 years. The current health risks for coal workers necessitate not only chest imaging but also spirometry (every 1–3 years), to provide an opportunity to protect lung health through early detection of rapid functional declines.98 Identification of rapidly declining lung function or worsening radiographic disease should prompt strict dust controls and transfer to low dust jobs when available. These workers should also be carefully advised about the risks of further dust exposures. Mine management and workers must assure that ventilation systems, water sprays, and other dust capture devices that are mandated by federal law are operating throughout the workshift and their effectiveness is continuously monitored.
Workers presenting with respiratory symptoms should have careful evaluation. Initial history and examination should be supplemented by a chest radiograph, spirometry with bronchodilators, diffusing capacity, electrocardiogram, and resting arterial blood-gas measurement as indicated.99 A comprehensive initial evaluation of the pulmonary system allows accurate assessment of the worker’s respiratory health status, and serves as a starting point for documenting the response to therapy or progression of disease. For miners who smoke, cessation is important regardless of symptoms, radiographic abnormalities, or functional status. Physician encouragement to stop smoking should be supplemented by support from smoking cessation groups, use of nicotine replacement, pharmacologic aids, and behavior modification techniques.99
Symptomatic reversible airflow obstruction may benefit from treatment with inhaled and oral bronchodilators. Patients with severe obstruction and inadequate improvement from the usual measures should be considered for a monitored trial of corticosteroids. If improvement is objectively documented, continuation of inhaled and, rarely, oral steroids may be of benefit. Hypoxemia can be a serious complication in advanced pneumoconiosis. It may be present at rest, with exercise, or during sleep. Chronic hypoxemia can lead to additional complications including polycythemia, pulmonary hypertension, cor pulmonale, and cerebral dysfunction. Therapy with low-flow oxygen is indicated when arterial oxygen tension is 55 torr or less. Oxygen therapy in this setting may improve exercise tolerance, reduce dyspnea, and prevent arrhythmias, polycythemia, and heart failure.100 Patients with functional abnormalities and/or radiographic CWP should receive appropriate immunization with influenza and pneumococcal vaccines.101 Bacterial and viral episodes of bronchitis or pneumonia should be promptly recognized and appropriately treated.
Patients with complicated pneumoconiosis, especially those who have been exposed to silica as well as coal mine dust, deserve special attention with regard to mycobacterial infection.72 These patients are considered at higher risk of TB than the general US population; thus a purified protein derivative test with >10 mm of induration is considered positive.102 Patients with a history of weight loss, fever, sweats, or malaise should be promptly investigated with chest radiographs and sputum examination for acid-fast bacilli stains and cultures. Occasionally, the sputum may be negative and mycobacterial infection can only be documented by fiberoptic bronchoscopy with brushings and washings. Active tuberculosis in patients with CWP can, in general, be successfully treated with the usual drug regimens provided rifampin is one of the drugs used. However, some authorities would recommend that in coal miners with a significant history of concurrent silica exposure (such as motormen, roof bolters, drillers, and shaft development workers), the treatment regimens for tuberculosis should be more prolonged, and long-term follow-up is indicated in view of several reports of recurrent pulmonary tuberculosis in patients with PMF after completion of apparently adequate therapy.103
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree