Early repolarization (ER) on a 12-lead electrocardiogram has recently been associated with ventricular tachyarrhythmias (VTAs) in patients without structural heart disease and in patients with healed myocardial infarction (MI). An association between ER and VTAs in the setting of acute ST-segment elevation MI (STEMI) has not been explored. In a single-center retrospective case–control design, 50 patients with STEMI complicated by VTAs (cases), defined as ventricular fibrillation, sustained ventricular tachycardia, or nonsustained ventricular tachycardia within 72 hours of the index hospitalization, were matched for age and gender with 50 subjects with STEMI without VTAs (controls). Electrocardiograms obtained an average of 1 year before STEMI were analyzed for ER pattern, defined as notching or slurring of the terminal QRS complex or J-point elevation >0.1 mV above baseline in ≥2 contiguous leads. A higher prevalence of ER was associated with VTAs overall in cases compared to controls (26% vs 4%, p = 0.01) and localized to anterior (16% vs 0%) and inferior (14% vs 2%, p = 0.07) leads but not lateral limb leads. Notching (10% vs 2%, p = 0.1) and J-point elevation (16% vs 0%) were more common in cases. Slurring was uncommon. ER was associated with VTAs (odds ratio [OR] 6.5, 95% confidence interval [CI] 1.5 to 28.8, p = 0.01), even after adjustment for creatine kinase-MB (OR 9.2, 95% CI 1.6 to 53.4, p = 0.01) and ejection fraction (OR 5.7, 95% CI 1.2 to 27.1, p = 0.03). In conclusion, ER is associated with VTAs in patients with STEMI even after adjustment for left ventricular ejection fraction or creatine kinas-MB levels. Larger prospective studies exploring potential associations and mechanisms of ventricular arrhythmogenesis with ER pattern are needed.
Ventricular tachyarrhythmia (VTA) is a well-recognized complication during acute ST-segment elevation myocardial infarction (STEMI) and carries a significant risk of sudden cardiac death. Although the incidence of sudden cardiac death has decreased with improvements in arrhythmia detection and medical therapy, several variables in the peri-STEMI setting have been identified as significant predictors of VTAs including infarct size and location, Killip class, and Thrombolysis In Myocardial Infarction flow grade before and after percutaneous coronary intervention. However, there are no reliable and easily obtainable clinical phenotypes preceding STEMI that may help identify patients who are susceptible to VTAs during STEMI. Early repolarization (ER) historically has been viewed as a benign finding on the 12-lead electrocardiogram (ECG). However, recent studies have implicated ER with idiopathic ventricular fibrillation in patients with structurally normal hearts. In addition, a recent study has shown a positive association between ER and VTAs in patients with chronic coronary artery disease and a history of healed MI. To date, there have been no studies that assessed the association between VTAs and ER in the setting of STEMI. Because this patient population is at significant risk for VTAs, we performed a case–control study to explore whether ER is associated with a heightened risk of VTAs in the setting of acute STEMI.
Methods
This was a single-center retrospective case–control study that identified patients from a STEMI database spanning 2002 through 2008 at our institution. The study population consisted of patients who had STEMI complicated by VTAs (cases) who were matched to patients who sustained STEMI but did not develop VTAs (controls). The study was approved by the Institutional Review Board at Northwestern Memorial Hospital.
In total 425 patients with STEMI were admitted from the emergency department to our institution from 2002 to 2008. STEMI was defined by new STE at the J-point in 2 contiguous leads with cut-off points >0.2 mV in men or >0.15 mV in women in leads V 2 to V 3 or >0.1 mm in other leads and an increase of troponin >99th percentile of the upper reference limit. Creatine kinase-MB levels (nanograms per liter) also were collected and peak creatine kinase-MB levels were recorded to correlate to infarct size. Patients selected for this study received coronary angiography and an appropriate percutaneous coronary intervention during the index hospitalization. Infarct locations were classified as anterior, inferior, or other based on angiographic findings, and patients may have had infarction in >1 myocardial region. Left ventricular ejection fraction assessment was performed by echocardiography during the index hospitalization. Patients excluded from this study were those without a baseline ECG before STEMI; those who sustained STEMI during an inpatient hospitalization; those with suspected Brugada syndrome, defined as right bundle branch block and STE (>0.2 mV) in precordial leads V 1 to V 3 ; those with QRS complexes ≥120 ms; and those with a documented history of congestive heart failure, MI, or angina. In addition, we excluded patients with cardiogenic shock on presentation requiring hemodynamic support such as inotropes or intra-aortic balloon pump placement. Clinical characteristics were obtained through chart review.
The case group consisted of 50 patients with documented VTA episodes during the first 72 hours of the index hospitalization for STEMI. We included a priori all VTAs that occurred in the first 72 hours of the index hospitalization because this was the common time frame of intensive care and telemetry monitoring and because patients sustaining acute MI are vulnerable to VTAs during this period. VTAs were defined by documented arrhythmia through chart review with an accompanying rhythm strip or ECG of the VTA episode. Two trained professionals reviewed each rhythm strip to confirm and categorize the VTA as ventricular fibrillation, sustained ventricular tachycardia (VT), or nonsustained VT. Sustained VT was differentiated from nonsustained VT if the VTA lasted ≥30 seconds or required external defibrillation. To explore associations between pre-existing ER pattern (substrate), a trigger (STEMI), and events (VTAs), we included patients with nonsustained VT in the analysis. In exploratory analyses we subclassified nonsustained VT as significant if the episode of nonsustained VT (>100 beats/min) was >15 beats and monomorphic. Therefore, significant VTAs included ventricular fibrillation, sustained VT, and nonsustained VT >15 beats. The control group consisted of 50 patients with STEMI who were matched to cases by age and gender. Controls were randomly selected and qualified for inclusion if there was no documentation of VTAs through chart review. All patients with STEMI routinely spent 2 to 3 days in the coronary care unit where continuous telemetry monitoring was available.
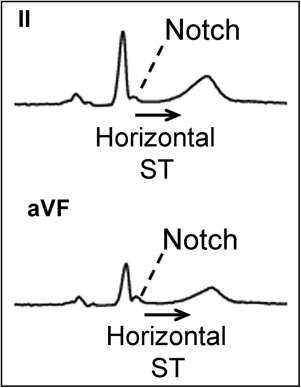
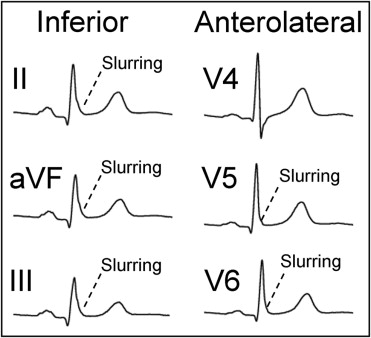
The most recent ECG before STEMI was identified for ER characteristics. Twelve-lead ECGs were digitally downloaded from the GE Marquette MUSE system (GE Medical Systems, Milwaukee, Wisconsin) and were analyzed offline using custom-designed software developed using MATLAB (MathWorks, Natick, Massachusetts) for semiautomated measurement of ER. Three trained investigators independently performed manual over-reading of the automated analysis to verify correct ER markings. In addition, ST-segment morphology was characterized. In the event of a misplaced marking by automated analysis, all reviewing investigators were required to agree on the location of the ER marking. ECGs were coded to blind investigators from clinical characteristics and patient grouping. ER was defined as notching, slurring, or J-point elevation ≥0.1 mV above baseline in ≥2 contiguous inferior, lateral, or anterior leads. Terminal QRS was characterized as exhibiting notching or slurring if it met amplitude criteria. Notching was classified as a positive deflection at the terminal portion of a positive QRS complex ( Figure 1 ). Slurring was defined as a smooth transition from the QRS complex to the ST segment with upright concavity ( Figure 2 ). Amplitude of notching was measured at the peak of the positive deflection relative to QRS onset, and amplitude of slurring was measured at the inflection point of the QRS complex relative to QRS onset. J-point amplitude was measured at the QRS–ST junction (J-point) and relative to QRS onset to minimize the baseline wandering effect. Amplitude was calculated as a pooled mean among all types of ER. ECGs that met criteria for ER were subsequently analyzed for ST-segment morphology, defined as horizontal/descending or concave/ascending, using previously published criteria.
Continuous variables are reported as mean ± SD and categorical variables are presented as number and percentage in each group. Comparison of continuous variables between cases and controls was performed with Student’s t test because all continuous variables were normally distributed. Comparison of categorical variables was performed with McNemar test. Prevalence of ER patterns comparing cases to controls was assessed by conditional logistic regression analysis; odds ratios (ORs) for the association between ER presence and VTAs were adjusted for creatine kinase-MB level and left ventricular ejection fraction in separate univariate analyses. Multivariate analysis was not possible because of the small sample and low prevalence of ER. Analyses were considered significant at a p value <0.05 (2-tailed). All statistical analyses were performed with SAS (SAS Institute, Cary, North Carolina).
Results
Table 1 lists baseline characteristics of the study population. Case subjects with VTAs included 30 men and 20 women with a mean age of 65.6 ± 12.8 years. The control group consisted of 50 patients matched for age (65.3 ± 13.5 years) and gender. There was a trend toward a lower prevalence of hypertension in cases compared to controls (68% vs 86%, p = 0.05). Left ventricular ejection fraction was significantly lower in cases compared to controls (40.7 ± 12.2% vs 48.3 ± 10.9%, p = 0.001), and peak creatine kinase-MB levels were significantly higher in cases compared to controls (211 ± 226 vs 109 ± 113 ng/ml, p = 0.002). Controls also had longer PR intervals and QRS durations. Otherwise, no significant differences in baseline characteristics were noted.
| Variable | Cases (n = 50) | Controls (n = 50) | p Value |
|---|---|---|---|
| Age (years) | 65.6 ± 12.8 | 65.3 ± 13.5 | 0.8 |
| Men | 30 (60%) | 30 (60%) | 1 |
| White | 36 (72%) | 38 (76%) | 0.8 |
| Smoker | 31 (62%) | 28 (56%) | 0.7 |
| Diabetes mellitus | 14 (28%) | 16 (32%) | 0.8 |
| Hypertension | 34 (68%) | 43 (86%) | 0.05 |
| Medications at presentation | |||
| β Blocker | 19 (38%) | 22 (44%) | 0.7 |
| Statin | 21 (42%) | 25 (50%) | 0.5 |
| Presenting characteristics | |||
| Infarct location ⁎ | |||
| Anterior | 26 (52%) | 23 (46%) | 0.7 |
| Inferior | 22 (44%) | 23 (46%) | 1 |
| Other | 10 (20%) | 12 (24%) | 0.8 |
| Systolic blood pressure (mm Hg) | 127 ± 28 | 124 ± 26 | 0.72 |
| Heart rate (beats/min) | 82 ± 24 | 77 ± 18 | 0.38 |
| Troponin (μg/L) | 26.8 ± 30.3 | 32.8 ± 59.6 | 0.33 |
| Creatine kinase-MB (ng/ml) | 211.4 ± 226 | 108.8 ± 113 | 0.003 |
| Left ventricular ejection fraction (%) | 40.7 ± 12.2 | 48.3 ± 10.9 | 0.001 |
| Creatinine (mg/dl) | 1.3 ± 0.9 | 2 ± 3.4 | 0.15 |
| Baseline electrocardiographic characteristics | |||
| Heart rate (beats/min) | 75.8 ± 18.8 | 71.3 ± 14.5 | 0.24 |
| PR interval (ms) | 156.8 ± 21.4 | 171.0 ± 33.6 | 0.008 |
| QRS duration (ms) | 85.3 ± 10.0 | 90 ± 11.1 | 0.01 |
| Corrected QT interval (ms) | 418.9 ± 25.6 | 424.2 ± 27.8 | 0.32 |
| Arrhythmia type | |||
| Nonsustained ventricular tachycardia | 39 (78%) | — | |
| >15 beats | 2 (4%) | — | |
| 11–14 beats | 5 (10%) | — | |
| 5–10 beats | 26 (52%) | — | |
| <5 beats | 6 (12%) | — | |
| Sustained ventricular tachycardia | 3 (6%) | — | |
| Ventricular fibrillation | 8 (16%) | — |
Of the 50 cases, most (n = 39) had nonsustained VT (78%), 3 had sustained VT (6%), and 8 had ventricular fibrillation (16%). Most patients with nonsustained VT exhibited 5 to 10 beats of VTA (67%; Table 1 ). We included all VTAs that were documented during the index hospitalization for STEMI. However, if patients had multiple VTAs, only the most significant VTA was counted in the analysis.
Median intervals from baseline ECG to STEMI for cases and controls were 15 months (interquartile range 2 to 35.75) and 11.5 months (interquartile range 1.25 to 31.75), respectively. Overall prevalence of ER patterns (notching, slurring, or J-point elevation) was higher in cases compared to control subjects (26% vs 4%, OR 6.5, 95% confidence interval [CI] 1.5 to 28.8, p = 0.01), even after adjustment for peak creatine kinase-MB level (OR 9.2, 95% CI 1.6 to 53.4, p = 0.01) or left ventricular ejection fraction (OR 5.7, 95% CI 1.2 to 27.1, p = 0.03). When analyzing regional leads, ER was observed more frequently in inferior (14% vs 2%, p = 0.07) and anterior (16% vs 0%) leads in cases compared to control subjects after unadjusted analysis. There was no evidence of ER pattern in lateral limb leads (I and aVL) in cases or controls. Similarly, ER pattern in anterolateral precordial leads (V 4 to V 6 ) was uncommon in cases and controls (2% vs 2%). Because of the low prevalence of ER noted by regional electrocardiographic leads, multivariable analysis to adjust for creatine kinase-MB or left ventricular ejection fraction was not possible. In patients with ER, ST segments were analyzed for morphology. In cases with ER, 46% (n = 6) had horizontal/downsloping ST segments. The 2 control patients with ER had evidence of horizontal/downsloping ST segments.
When comparing morphologic characteristics of ER, there was no statistically significant association in prevalence of notching in cases compared to controls (10% vs 2%, p = 0.14). Slurring was uncommon in cases and controls (6% vs 2%, p = 0.34). J-point elevation was noted in 16% of cases (n = 8) and 0% of controls (n = 0); thus, conditional logistic regression analysis could not be performed. In patients with any ER pattern, there was no statistical difference in mean amplitude in cases and controls (0.11 ± 0.04 vs 0.12 ± 0.03 mV, p = 0.6 by paired t test).
In cases we found an overall statistically significant association between presence of ER and VTAs (26% vs 4%, OR 6.5, 95% CI 1.5 to 28.8). The prevalence of any ER pattern (notching, slurring, J-point elevation) based on arrhythmia type was 37.5% in patients with ventricular fibrillation, 26% in patients with nonsustained VT, and 0% in patients with sustained VT. In exploratory analyses, we did not find a statistically significant association of ER in the 13 cases who had significant (ventricular fibrillation, sustained VT, or nonsustained VT >15 beats) VTAs compared to matched controls (23% vs 8%, p = 0.30).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


