Chronic Gangrenous Foot, Nonvascularizable (Primary Amputation)
MARK NEHLER
Presentation
A 70-year-old man with diabetes, oxygen-dependent chronic obstructive pulmonary disease, hypertension, a 40-pack-year history of smoking, and end-stage renal disease presents with left heel gangrene. The patient has been minimally ambulatory after a recent hospitalization for a fall and fractured hip repair. On examination, the patient has femoral pulses and no pulses distally. There is a dry eschar on the left heel that encompasses most of the heel but no surrounding erythema and no odor (Fig. 1). He has a mild contracture at the left knee.

FIGURE 1 Heel eschar in patient with critical limb ischemia and end-stage renal disease.
Differential Diagnosis
Heel lesions always involve some level of pressure and potentially neuropathy as components. Although they can occur in the setting of a fully ambulatory patient due to poorly fitting footwear, the current presentation is much more common. Patients with heel lesions often are at least briefly nonambulatory, frequently due to some acute event (in this case a hip fracture). In addition to the pressure issues, patients with heel lesions frequently have some level of peripheral vascular disease. Therefore, evaluation of the arterial circulation is important. Finally, there is no completely agreed-upon definition of an unsalvageable foot lesion. Heel lesions are notoriously difficult to manage due to poor local blood supply of the fat pad. Determination of the involvement of the calcaneus is critical as most would consider that to be an indication of nonsalvageable.
Workup
Plain films demonstrate no soft tissue gas and no evidence of calcaneal osteomyelitis. Segmental pressures demonstrate suprasystolic pressures at multiple levels including the ankles. Toe pressures are 20 mm Hg bilaterally. Duplex shows both common femoral arteries are calcified but patent with biphasic waveforms and normal velocities. Both superficial femoral arteries show severe calcification and multiple stenoses with bilateral popliteal occlusions. After discussion with the patient and family, it is clear that his overall function has declined in the last 6 months. This has been markedly so since his fall and hip fracture where he has been minimally ambulatory since. He was living independently prior to the fall but now has required live-in assistance.
Discussion
The decision for a primary amputation is not an easy one for the surgeon or the patient. Most amputations done by vascular surgeons follow failed attempts at revascularization/limb salvage. However, a number of factors play into the decision for a primary amputation. The functional status of the patient is extremely important. Multiple series examining function in critical limb ischemia patients undergoing revascularization demonstrate that patients who are nonambulatory at baseline do not gain significant functional benefits and the patients who are ambulatory at baseline often take a functional hit in the first few weeks postoperatively that the majority will recover from over time (Fig. 2). Another issue that is critical is the extent and nature of the foot lesion. Extensive necrosis theoretically can be managed with a variety of partial forefoot amputations and even free flap tissue coverage. In good-risk functional patients, this can be a useful strategy. However, the time for wound healing in these cases is usually measured in months not weeks, a substantial amount of downtime that often reduces function substantially due to deconditioning. A lack of revascularization option usually is an issue associated with secondary amputation after prior revascularization failure as the vast majority of patients with critical limb ischemia will have some revascularization option to attempt as a first-line therapy.
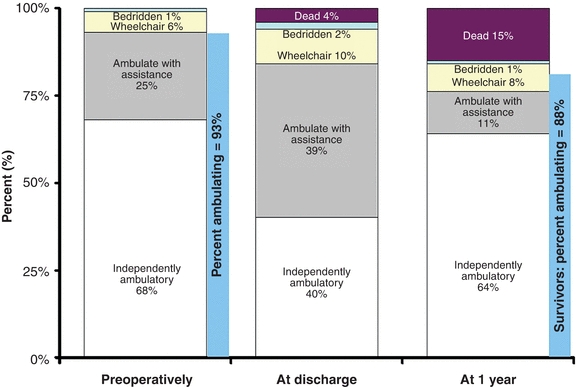
FIGURE 2 Ambulation status preoperatively, at discharge, and at 1 year in patients undergoing bypass revascularization for critical limb ischemia. (From Goodney PP, et al. Predicting ambulation status one year after lower extremity bypass. J Vasc Surg. 2009;49:1431–1439, used with permission.)
Patients with end-stage renal disease are especially problematic for limb salvage. The success rate for same is less than patients without end-stage renal disease. More importantly, the survival in patients with end-stage renal disease and critical limb ischemia is extremely limited. So decisions regarding heroic attempts for limb salvage in this population should be made with caution. The alternative of primary amputation also has high perioperative morbidity and mortality and reduced survival over time but is often more of a palliative procedure (Fig. 3).
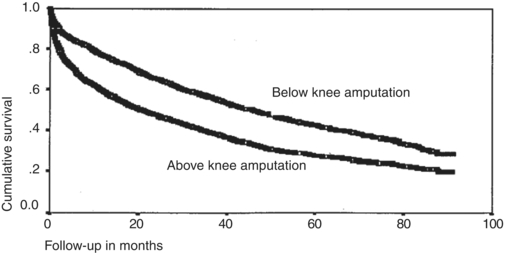
FIGURE 3 Major amputee Kaplan-Meier survival. (From Feinglass J, et al. Postoperative and late survival outcomes after major amputation. Findings of the Department of Veterans Affairs National Surgery Quality Improvement Program. Surgery. 2001:130: 21–29, used with permission.)
Diagnosis and Treatment
After discussion with the patient and family, it was decided to proceed with a primary amputation. This was primarily due to the patient’s wish to have one procedure and not require repeat hospitalizations/procedures and also due to his declining functional status since his recent hip fracture. The next decision was above, through, or below the knee. The goal of saving the knee joint is to preserve ambulation with a prosthesis. However, a below-knee amputation often requires two procedures (if there is any question of pedal sepsis, a guillotine should be done first) and has a much greater wound failure rate than above-knee amputation. The trade-off is any potential ambulation in an elderly patient with critical limb ischemia is eliminated with loss of the knee joint. Through-knee amputations have gained popularity in select patients as the ambulation capability is much better than above-knee amputations with newer computerized prosthetics at the expense of somewhat greater wound complications.
The current patient has been minimally ambulatory with two legs due to recent hip fracture, and the focus really became palliation with reducing procedures and time in hospital. He had been considering withdrawal of dialysis due to his reduction in quality of life, a top cause of death in elderly patients on dialysis that is often prompted by acute events. He also has a knee contracture that would complicate his ability to salvage his knee joint. Due to the wishes of the patient and family and his modest functional outlook, the decision was made to perform an above-knee amputation. The circulation needed for healing at the below-knee level has been best predicted by either a TC02 35 mm Hg or greater or a normal profunda femoris artery on imaging. This patient has a patent profunda femoris artery on duplex examination and should be able to heal at the above-knee level well. One final part of the workup for an above-knee amputation for this patient was plain films to determine the length of the femoral portion of the recent hip reconstruction. The goal would be to transect the femur well below the existing hardware. Transecting the hardware would require special tools and risk hardware infection.
Postoperative Issues and Rehabilitation Potential
The morbidity and mortality of major limb amputation is not trivial. Multiple large databases state an operative mortality of 7% for below-knee amputations and roughly double that for above-knee amputations (Table 1). This mortality is primarily related to the comorbidities of the population undergoing amputation rather than the technical challenges of the procedure. Major postoperative morbidities are cardiac, thromboembolism, and also infection.
TABLE 1. Thirty-day Postoperative Mortality in Various Risk Quartilesa for Above- and Below-Knee Amputation in the Veterans Affairs National Surgery Quality Improvement Program
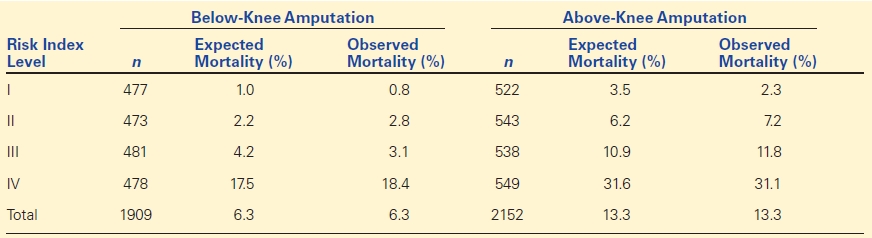
aApproximate quartiles of mean expected versus observed mortality.
From Feinglass J, et al. Postoperative and late survival outcomes after major amputation. Findings of the Department of Veterans Affairs National Surgery Quality Improvement Program. Surgery. 2001:130:21–29, used with permission.



