Fig. 21.2 Left ventricular hypertrophy (LVH). Substantial increase in the voltage of the leads looking at the left ventricle – the R wave in V5 = 33 mm (exceeding that for the diagnosis of LVH in many scoring systems – see Chapter 24). In addition, there are gross ST–T changes, with ST depression/T wave inversion in most of the chest leads (V3–6). There is also T wave inversion in the inferior leads (II, III, aVF). This ECG shows severe LVH with generalized repolarization changes, too extensive to be just due to acquired LVH. The diagnosis is therefore hypertrophic cardiomyopathy (HCM), or in addition to acquired hypertrophy (from hypertension or aortic stenosis) there is another process such as ischaemia from critical coronary disease. In fact, the patient had HCM.
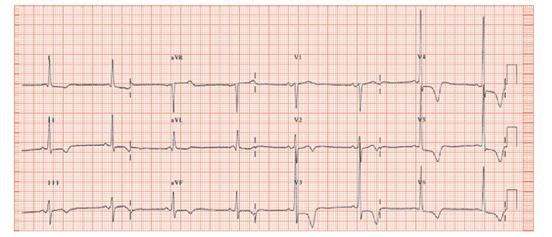
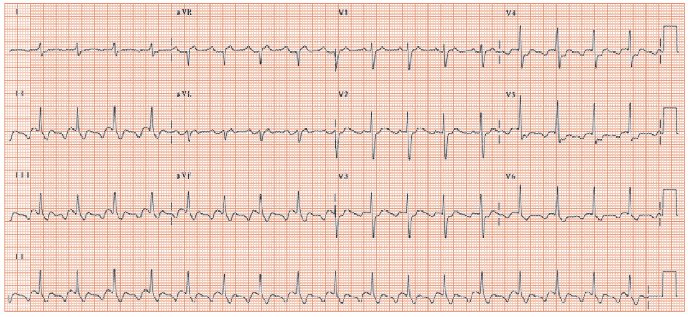
Fig. 21.3 Atrial tachycardia. The rhythm is not immediately apparent. From lead V1 it is easy to miss the second P wave buried in the T wave. However, inspection of lead II shows two abnormally shaped P waves for every QRS complex. The differential diagnosis includes atrial flutter. However, as an iso-electric line is clearly seen between the P waves in lead II, not found in classic atrial flutter, it is more likely that this is an automatic atrial arrhythmia, such as atrial tachycardia.
The cause of long-standing breathlessness can be identified from the history, physical examination, and simple tests including the ECG, spirometry, chest X-ray and brain natriuretic peptide (BNP). Occasionally more sophisticated tests are necessary, including cardiac magnetic resonance (MR), cardiac catheterization and specialized lung tests.
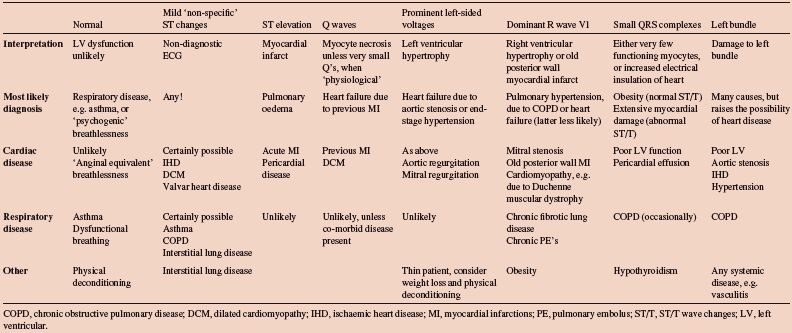
Heart failure is diagnosed from: (i) identifying a predisposing cause (e.g. rheumatic fever, hypertension, valvar heart disease, previous myocardial infarction [MI] [Fig. 21.1]); (ii) resulting in effort breathlessness without wheeze, orthopnoea, ankle oedema; (iii) physical examination – large heart, third heart sound, bibasal inspiratory lung crepitations, raised venous pressure, ankle oedema; and (iv) investigations – cardiac ultrasound, ECG and BNP. Most patients have ECG abnormalities, depending on aetiology (Table 21.1): (i) ischaemic heart disease, heart failure relates to a previous MI and the ECG shows pathological Q waves or regional loss of R wave height; (ii) aortic stenosis, the ECG shows left ventricular hypertrophy (LVH); (iii) cardiomyopathy, often idiopathic dilated cardiomyopathy (DCM), the ECG often shows atrial fibrillation (AF), small QRS complexes and diffuse ST changes, and, rarely, hypertrophic cardiomyopathy (HCM) (Fig. 21.2). The severity/extent of the ECG changes in heart failure often relate to the severity of cardiac damage, though there are many exceptions. Heart failure with a normal ECG is possible, but unlikely. If the ECG is normal, then causes other than heart failure should be considered first.
Chronic obstructive airways disease (COPD) causes slowly progressive effort breathlessness with wheeze, no orthopnoea, with exacerbations, and, when the right heart fails (‘cor pulmonale’), peripheral oedema. The ECG may show the consequences of the destruction of the pulmonary arterial circulation, and the difficulty the right ventricle has in pushing blood into the lungs – right ventricular hypertrophy, with deviation of the QRS axis to the right and/or a dominant R wave in lead V1. Surprisingly the ECG often shows neither of these changes, despite dramatic increases in pulmonary artery pressure. The commonest findings in COPD are: (i) low voltage QRS complexes, due to the increased lung volume decreasing the transmission of electricity to the chest wall; and (ii) non-specific ST flattening, often throughout the ECG leads.
Obesity is usually obvious. The ECG shows small PQRST complexes, but no T wave abnormalities. Anterior wall myocardial infarction also often shows small QRS waves, though often with flat or inverted T waves. Thus changes in the T wave are useful to tell ‘straightforward’ obesity apart from myocardial damage.
Physical deconditioning has no pathognomonic ECG changes, but the history is suggestive. Resting heart rate and QT interval increase with unfitness though, in those without cardiac disease, are still often within the normal range. An exercise test shows a low work capacity, due to breathlessness, with a very brisk increase in heart rate, but no ECG changes.
Anaemia suspected from the physical examination, and confirmed by a blood count. The ECG is unremarkable.
Arrhythmias usually do not cause breathlessness, unless there is preexisting left ventricular dysfunction, or the arrhythmias have resulted in left ventricular impairment, or the arrhythmias are very fast or very (≤ 30 b/min) slow. The ECG is diagnostic (Fig. 21.3).
Table 21.1 ECG findings in different causes of breathlessness.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


