INDICATIONS/CONTRAINDICATIONS
Thoracic outlet syndrome (TOS) is a group of relatively uncommon, anatomically related, conditions caused by compression of neurovascular structures that serve the upper extremity. The most frequent form is neurogenic TOS (NTOS), which occurs in 85% to 90% of patients, most typically between the ages of 15 and 40. NTOS is characterized by symptoms arising from extrinsic compression and irritation of the brachial plexus nerves within the supraclavicular scalene triangle or within the infraclavicular subcoracoid space beneath the pectoralis minor muscle tendon (Fig. 10.1). NTOS results in neck and upper extremity pain, paresthesias, and functional limitations. Clinical recognition and appropriate treatment of NTOS are crucial to prevent disability in young active individuals (Table 10.1).
NTOS is caused by a combination of two factors: Predisposing anatomical variations and previous neck or upper extremity injury. The anatomical variations that may predispose to NTOS include anomalous scalene musculature, aberrant fibrofascial bands, and/or cervical ribs. Injury superimposed on this anatomical area can subsequently result in scalene/pectoralis muscle spasm, fibrosis, and other pathologic changes, which in turn lead to compression and irritation of the adjacent brachial plexus nerves. While the types of injury precipitating NTOS can include a motor vehicle collision with whiplash-type cervical strain or a fall on the outstretched arm, NTOS can also arise as a consequence of repetitive strain associated with frequent heavy lifting, poor posture, overhead use of the arm, or prolonged work at a computer keyboard. Although the presence of a cervical rib is often considered a prerequisite to the development of NTOS, only a small proportion of patients (approximately 10%) exhibit a definable cervical rib on radiographic studies, and in the absence of some form of additional injury, development of symptoms of NTOS remains rare even in patients with cervical ribs.
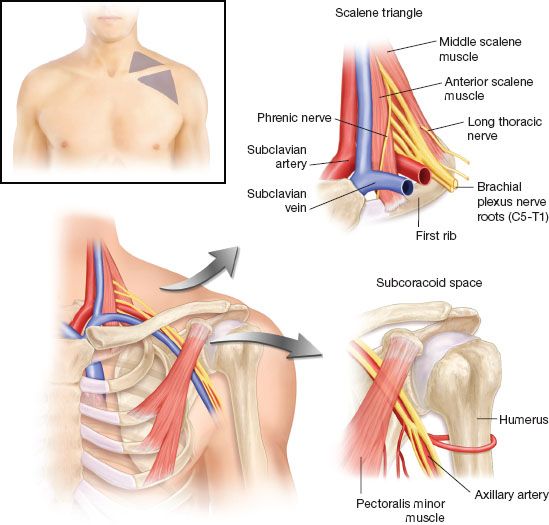
Figure 10.1 Anatomy of the thoracic outlet, with emphasis on the supraclavicular scalene triangle and the infraclavicular subcoracoid space.
Other forms of TOS include compression of the subclavian vein (venous TOS), most often presenting with the axillary–subclavian vein “effort thrombosis” (Paget–Schroetter) syndrome. This condition is readily differentiated from NTOS, as it results in marked arm swelling, cyanotic discoloration, and distention of subcutaneous veins around the shoulder and chest wall and is not usually associated with pain and paresthesia. The least frequent form of TOS arises from compression of the subclavian artery with pathologic changes (arterial TOS), usually in patients with a bony anatomical anomaly (e.g., cervical rib). Arterial TOS can result in fixed subclavian artery obstruction, resulting in cramping muscular fatigue with arm use similar to intermittent claudication. More frequently, it leads to poststenotic subclavian artery aneurysm formation and thromboembolism, hand ischemia, rest pain, and/or digital ulceration and necrosis. This clinical presentation is also readily differentiated from that of NTOS. It is important to recognize that positional compression of the subclavian artery during elevation of the arm is a frequent finding on physical examination in a substantial number of asymptomatic individuals and should not be considered evidence for arterial TOS in the absence of established arterial pathology.
TABLE 10.1 Differential Diagnosis of NTOS
Surgical treatment for NTOS can be accomplished effectively by several different approaches, including transaxillary first rib resection and anterior (supraclavicular) decompression, with each approach having its advantages and disadvantages. Supraclavicular decompression for NTOS most frequently involves complete anterior and middle scalenectomy, first rib resection, and brachial plexus neurolysis. This operation provides superb surgical exposure, a high degree of safety in experienced hands, and the most definitive means to address the relevant neurovascular structures, as well as flexibility in managing the entire spectrum of circumstances that may be encountered.
Supraclavicular decompression is a recommended treatment option for NTOS when the clinical diagnosis is considered to be sound and the patient has had substantial disability, with symptoms that interfere with daily activities and/or work. A third criterion for surgical treatment is that the patient has had an insufficient response to a course of physical therapy that has been appropriately targeted toward NTOS. Use of the supraclavicular approach to thoracic outlet decompression is also recommended when there has been no response to appropriate conservative measures in patients with persistent or recurrent symptoms of NTOS following a previous operation.1
For individuals with symptoms of disabling NTOS that are referable on physical examination to the subcoracoid space, the inclusion of pectoralis minor tenotomy is an important consideration as part of supraclavicular thoracic outlet decompression. In patients with NTOS in whom nerve compression symptoms appear confined to the subcoracoid space, pectoralis minor tenotomy may be performed as an isolated procedure.
 PREOPERATIVE PLANNING
PREOPERATIVE PLANNING
In the preoperative holding area, the supraclavicular surgical site is confirmed and marked. The subcoracoid space is included if concomitant pectoralis minor tenotomy is planned. Prophylactic antibiotics are administered within an hour of the planned procedure.
 SURGERY
SURGERY
Positioning
After general endotracheal anesthesia is induced, the patient is positioned supine with the head of the operating table elevated approximately 30 degrees. The neck is extended and turned to the opposite side, and a small inflatable pillow is placed behind the shoulders. The neck, chest, and affected upper extremity are prepped into the sterile field, and the arm is wrapped in stockinette to permit free range of movement during the operation (Fig. 10.2). Lower extremity sequential compression devices are placed for prophylaxis against thromboembolism.
Incision
A transverse neck incision is made parallel to and just above the clavicle. This begins at the lateral edge of the sternocleidomastoid muscle and extends to the anterior edge of the trapezius muscle. The incision is carried through the subcutaneous layer and the platysma muscle is divided, then subplatysmal flaps are developed to expose the scalene fat pad. The sternocleidomastoid muscle is retracted medially, but it is not divided (Fig. 10.3).

Figure 10.2 Patient position and planned incisions for left-sided supraclavicular thoracic outlet decompression with pectoralis minor tenotomy.
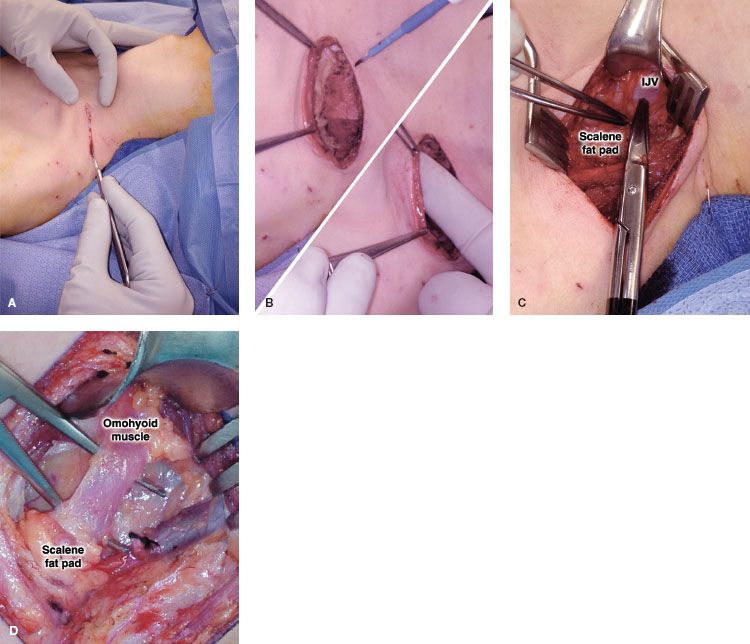
Figure 10.3 The skin incision is made just above and parallel to the clavicle, extending from the lateral border of the sternocleidomastoid muscle to the anterior border of the trapezius muscle (A). Subplatysmal flaps are created to expose the underlying scalene fat pad (B). The scalene fat pad is mobilized, beginning with its medial attachments to the internal jugular vein (IJV) (C), and the omohyoid muscle is divided (D).
Mobilization of the Scalene Fat Pad
One of the keys to simplifying the supraclavicular exposure is proper mobilization and lateral reflection of the scalene fat pad.
 The scalene fat pad is initially detached with the electrocautery along the lateral edge of the internal jugular vein and along the superior edge of the clavicle, while ligating small blood vessels and lymphatics. The omohyoid muscle is routinely divided. The thoracic duct is usually identified near the junction of the internal jugular and subclavian veins (this is more prominent on the left side, but a prominent accessory thoracic duct may also be found on the right side), and it may be ligated and divided (Fig. 10.3).
The scalene fat pad is initially detached with the electrocautery along the lateral edge of the internal jugular vein and along the superior edge of the clavicle, while ligating small blood vessels and lymphatics. The omohyoid muscle is routinely divided. The thoracic duct is usually identified near the junction of the internal jugular and subclavian veins (this is more prominent on the left side, but a prominent accessory thoracic duct may also be found on the right side), and it may be ligated and divided (Fig. 10.3).
 Using gentle fingertip dissection, the scalene fat pad is progressively elevated by moving in a medial to lateral direction, over the surface of the anterior scalene muscle. The phrenic nerve is identified as it descends along the muscle surface, passing in a lateral to medial direction, with a “dartle” (diaphragmatic startle) response elicited by gentle manipulation.
Using gentle fingertip dissection, the scalene fat pad is progressively elevated by moving in a medial to lateral direction, over the surface of the anterior scalene muscle. The phrenic nerve is identified as it descends along the muscle surface, passing in a lateral to medial direction, with a “dartle” (diaphragmatic startle) response elicited by gentle manipulation.
 With further lateral mobilization of the scalene fat pad, the brachial plexus nerve roots (posterior and lateral to the anterior scalene muscle), and the middle scalene muscle (behind the brachial plexus) are gradually brought into view. The lateral aspect of the first rib may also be palpated and visualized at this stage. The long thoracic nerve is observed where it emerges from the body of the middle scalene muscle and passes beyond the lateral part of the first rib. The mobilized scalene fat pad is then held in position with several silk retraction sutures. The exposure is further maintained with a Henley self-retaining retractor, using the third arm to hold the edge of the sternocleidomastoid muscle. This exposure represents the first and most important of six “critical views” that should be obtained during supraclavicular decompression (Table 10.2) (Fig. 10.4).
With further lateral mobilization of the scalene fat pad, the brachial plexus nerve roots (posterior and lateral to the anterior scalene muscle), and the middle scalene muscle (behind the brachial plexus) are gradually brought into view. The lateral aspect of the first rib may also be palpated and visualized at this stage. The long thoracic nerve is observed where it emerges from the body of the middle scalene muscle and passes beyond the lateral part of the first rib. The mobilized scalene fat pad is then held in position with several silk retraction sutures. The exposure is further maintained with a Henley self-retaining retractor, using the third arm to hold the edge of the sternocleidomastoid muscle. This exposure represents the first and most important of six “critical views” that should be obtained during supraclavicular decompression (Table 10.2) (Fig. 10.4).
Anterior Scalenectomy
Attention is next turned to detachment of the anterior scalene muscle from its insertion on the top of the first rib and subsequent resection of the muscle up to the apex of the scalene triangle.
 The lower lateral edge of the anterior scalene muscle is dissected where it attaches to the first rib. The subclavian artery and brachial plexus are carefully mobilized away from the muscle, until a fingertip can be easily passed behind the muscle just above the first rib to displace the neurovascular structures posterolaterally. Blunt fingertip dissection is then continued in front of and behind the muscle to its medial edge, taking care to avoid the phrenic nerve by gentle medial retraction. Once the insertion of the anterior scalene muscle onto the top of the first rib has been completely isolated under direct vision, it is sharply divided from the top of the bone with scissors (Fig. 10.5).
The lower lateral edge of the anterior scalene muscle is dissected where it attaches to the first rib. The subclavian artery and brachial plexus are carefully mobilized away from the muscle, until a fingertip can be easily passed behind the muscle just above the first rib to displace the neurovascular structures posterolaterally. Blunt fingertip dissection is then continued in front of and behind the muscle to its medial edge, taking care to avoid the phrenic nerve by gentle medial retraction. Once the insertion of the anterior scalene muscle onto the top of the first rib has been completely isolated under direct vision, it is sharply divided from the top of the bone with scissors (Fig. 10.5).
TABLE 10.2 Critical Views Obtained During Supraclavicular Thoracic Outlet Decompression
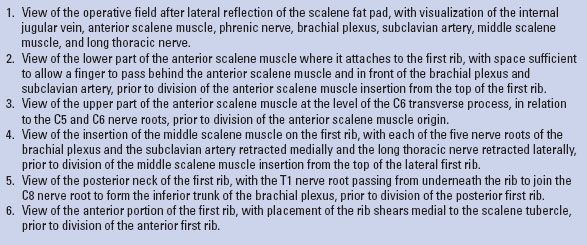
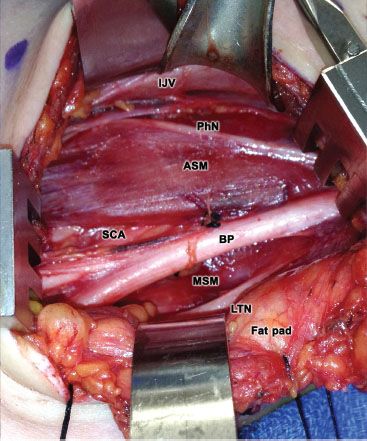
Figure 10.4 Following lateral reflection of the scalene fat pad, direct visualization is obtained of the internal jugular vein (IJV), anterior scalene muscle (ASM), phrenic nerve (PhN), brachial plexus (BP), subclavian artery (SCA), middle scalene muscle (MSM), and long thoracic nerve (LTN).
 The end of the divided anterior scalene muscle is elevated and its attachments to the underlying extrapleural fascia are sharply divided, avoiding electrocautery to prevent inadvertent nerve injury. Any muscle fibers extending from the posterior aspect of the muscle to the subclavian artery are divided to fully release the artery, and any scalene minimus muscle fibers (which pass between the roots of the brachial plexus) are divided. The anterior scalene muscle is then passed underneath and medial to the phrenic nerve, to better visualize and protect the upper brachial plexus nerve roots. The origin of the anterior scalene muscle on the C6 transverse process is palpated in the upper aspect of the operative field (the apex of the “scalene triangle”) and the muscle is divided with scissors under direct vision. The entire anterior scalene muscle is removed with a typical specimen weighing 5 to 10 g. Minor bleeding from the edge of the divided muscle origin should be controlled with a small polypropylene suture rather than electrocautery, given the proximity of the nerve roots (Fig. 10.5).
The end of the divided anterior scalene muscle is elevated and its attachments to the underlying extrapleural fascia are sharply divided, avoiding electrocautery to prevent inadvertent nerve injury. Any muscle fibers extending from the posterior aspect of the muscle to the subclavian artery are divided to fully release the artery, and any scalene minimus muscle fibers (which pass between the roots of the brachial plexus) are divided. The anterior scalene muscle is then passed underneath and medial to the phrenic nerve, to better visualize and protect the upper brachial plexus nerve roots. The origin of the anterior scalene muscle on the C6 transverse process is palpated in the upper aspect of the operative field (the apex of the “scalene triangle”) and the muscle is divided with scissors under direct vision. The entire anterior scalene muscle is removed with a typical specimen weighing 5 to 10 g. Minor bleeding from the edge of the divided muscle origin should be controlled with a small polypropylene suture rather than electrocautery, given the proximity of the nerve roots (Fig. 10.5).
Middle Scalenectomy
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


