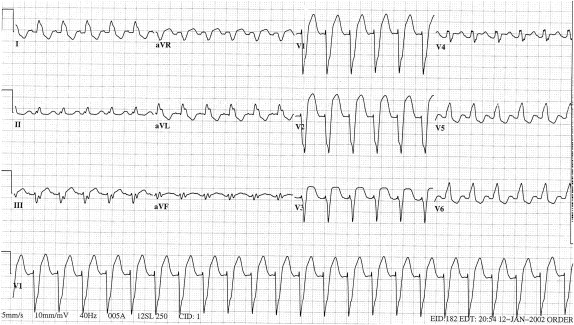
A 50-year-old man presented to the emergency department with chest pain and his initial electrocardiogram showed sinus tachycardia at a rate of 139 beats/min and left bundle branch block ( Figure 1 ). Because of persistent chest pain and ST-segment elevation of 0.7 mV in lead V 2 , he underwent coronary arteriography, which demonstrated subtotal occlusion of the left anterior descending coronary artery and high-grade narrowing of its diagonal branch and of the left circumflex and right coronary arteries. A left ventriculogram revealed an ejection fraction of 15%. Urgent multivessel coronary artery bypass grafting was then performed.
The electrocardiographic diagnosis of myocardial infarction in patients with right bundle branch block, which deforms the terminal portion of the QRS complex, usually is only minimally more difficult than in patients without a conduction defect. In contrast, left bundle branch block, which deforms the initial portion of the QRS, makes the diagnosis of myocardial infarction considerably more difficult. Seventy years ago, the preeminent electrocardiographer Wilson et al wrote, “In the presence of left bundle branch block it is seldom possible to make a diagnosis of myocardial infarction on the basis of electrocardiographic findings alone.”
Patients with acute myocardial infarction and left bundle branch block have a higher mortality rate than infarct patients with normal conduction, regardless of whether the left bundle branch block preceded the infarct or resulted from it. Prompt diagnosis of the infarct and reperfusion improve prognosis and are essential. Although the diagnosis of old myocardial infarction in the presence of left bundle branch block is nearly as difficult now as in Wilson’s day, we have made progress with acute myocardial infarction. Analysis of patients in the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries-1 trial who had left bundle branch block and acute chest pain has yielded 3 electrocardiographic criteria with independent value in the diagnosis of infarction. In order of decreasing predictive accuracy, these were ST-segment elevation ≥0.1 mV and concordant with the QRS complex; ST-segment depression ≥0.1 mV in lead V 1 , V 2 , or V 3 ; and ST-segment elevation ≥0.5 mV and discordant with the QRS complex ( Figure 1 ). Comparison of the electrocardiogram with previous tracings and serial electrocardiographic changes have also been found to be useful in diagnosing acute myocardial infarction in patients with left bundle branch block.
A variety of imaging techniques and cardiac markers may improve diagnostic accuracy but may also cost valuable time. The history has always been vital as it was in Wilson’s time. In our patient, the history was essential in making a prompt diagnosis and facilitating early revascularization.
Disclosures
The authors have no conflicts of interest to disclose.
See page 487 for disclosure information.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


