Guidelines recommend a ticagrelor loading dose (LD) before PCI or a prasugrel LD at the time of percutaneous coronary intervention (PCI) in intermediate and high-risk non–ST-elevation acute coronary syndrome (NSTE-ACS). However, achieving an optimal PR inhibition at the time of PCI is critical to prevent adverse events and depends on the timing of LD intake in relation to PCI. We aimed to compare the rate of myonecrosis related to PCI in patients with NSTE-ACS receiving ticagrelor pretreatment versus prasugrel at the time of intervention. We prospectively randomized 213 patients with NSTE-ACS to a 180 mg of ticagrelor LD given as soon as possible after admission and before PCI or to a 60 mg LD of prasugrel given at the time of PCI. The primary end point was the rate of periprocedural myonecrosis as defined by an increase of >5 times the ninety-ninth percentiles in troponin-negative patients or a 20% increase in troponin-positive patients. The 2 groups were similar regarding baseline characteristics including clinical setting (p = 0.2). Procedural characteristics were also identical including the number of treated vessels and stenting procedures. Patients in the prasugrel group more often required emergent PCI (p = 0.001). Patients in the ticagrelor group had less periprocedural myonecrosis compared with those in the prasugrel group (19.8% vs 38.3%; p = 0.03). The rate of major adverse cardiovascular events and Bleeding Academic Research Consortium ≥2 at 1-month follow-up was low and similar between the 2 groups. In conclusion, a ticagrelor LD as soon as possible before PCI is superior to prasugrel at the time of PCI to prevent periprocedural myonecrosis in NSTE-ACS.
The current non–ST-elevation acute coronary syndrome (NSTE-ACS) guidelines advocate either a ticagrelor loading dose (LD) as soon as possible and before percutaneous coronary intervention (PCI) or a prasugrel LD at the time of intervention. However, to date no study has compared these 2 strategies. Of importance, despite their fast onset of action, ticagrelor and prasugrel require 1 to 6 hours to achieve optimal PR inhibition in ACS. Therefore, this difference in the timing of LD between the 2 drugs may have an impact on periprocedural myonecrosis. In fact, previous observational studies have clearly demonstrated that efficient P2Y12-ADP receptor blockade during PCI was associated with a significant reduction in periprocedural myonecrosis. Of importance, this event is of prognostic significance and correlates with mortality. We hypothesized that a ticagrelor protocol with an LD before PCI, because it allows for an optimal periprocedural PR inhibition, would be superior to a protocol of prasugrel loading at the time of PCI to prevent periprocedural myonecrosis. We, therefore, compared the rate of periprocedural myonecrosis between a ticagrelor and a prasugrel protocol in patients with NSTE-ACS who underwent PCI.
Methods
A prospective, monocenter, open-label randomized study was performed from January 2014 to September 2014. Patients between 18 and 75 years old who underwent PCI for an intermediate or high-risk NSTE-ACS and agreeing to participate in the study were eligible. The present study protocol conforms to the ethical guidelines of the 1975 Declaration of Helsinki as reflected in a priori approval by the institution’s human research committee. All patients gave an informed consent.
They were randomized according to a sequence generated using R software (blockrand package with block size randomly varying among 2, 4, and 6) to ticagrelor or prasugrel therapy. Ticagrelor and prasugrel were given according to the protocol recommended in the 2014 ESC guidelines for revascularization. In the ticagrelor group, patients received a 180 mg LD as soon as possible after the diagnosis of NSTE-ACS followed by 90 mg twice daily as maintenance dose. All patients received their LD at least 4 hours before PCI (13.4 ± 8.3 hours). In the prasugrel group, patients who underwent PCI received a 60 mg LD as soon as the coronary anatomy was known and the decision to proceed to PCI taken. They received prasugrel 10 mg daily as maintenance dose. The flow chart of the study is displayed in Figure 1 .
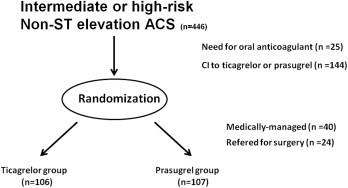
Exclusion criteria included ST-elevation ACS, NSTE-ACS medically managed or intended for surgery after PCI, cardiogenic shock, cardiac arrest, contraindication to antiplatelet therapy, treatment with a P2Y12-ADP antagonist <1 month, a platelet count <100 G/L, history of bleeding diathesis, history of hemorrhagic stroke, stroke, recent surgery (<1 month), age ≥75 years old, hemodialysis, weight <60 kg, treatment with a P2Y12-ADP receptor during the previous month, oral anticoagulant therapy, and use of medication with known interference with ticagrelor or prasugrel and bradycardia.
PCI was performed using the radial route in all cases but 4 (2 patients in each group). All patients received either a bolus of heparin (100 IU/kg) during the procedure followed by ACT-adjusted additional bolus or standard bivalirudin infusion. All patients received an LD of 150 mg of aspirin IV at the time of PCI. Drug-eluting stents were used in all patients.
Blood samples were collected and drawn by atraumatic venipuncture of the antecubital vein on admission, before PCI, 6, 12, and 24 hours after PCI and at any other time if clinically required.
Troponin Ic was measured on Centaur (SIEMENS, Munich, Germany) apparatus. This immunodosage implicates 1 polyclonal and 2 monoclonal antibodies for chemiluminescence signal. The ninety-ninth percentile value in a healthy population given by the manufacturer was 0.04 μg/L and the detection threshold 0.006 μg/L. The coefficient of variation was <10% in the measuring range.
The primary end point was the rate of periprocedural myonecrosis defined by an increase of >5 times the ninety-ninth percentiles of the assay in troponin-negative patients before PCI or a 20% increase compared with pre-PCI value in case of elevated baseline value within 24 hours after intervention.
Secondary end points included myocardial insults, which were defined as any troponin elevation more than the ninety-ninth percentiles in troponin-negative patients before PCI and any troponin increase in those with elevated baseline troponin levels within 24 hours after intervention. We also recorded clinical end points at 1-month post-PCI. These end points included major adverse cardiovascular events (MACE) and bleedings events. MACE comprised cardiovascular death, myocardial infarction, urgent revascularization, and stroke. Bleeding were classified according to the Bleeding Academic Research Consortium (BARC) classification. BARC score >2 were recorded.
The rate of periprocedural myonecrosis was assumed to be 40% in the prasugrel group. A sample size of 103 patients per group was required based on the ability to detect a relative reduction of 45% for the primary end point in the ticagrelor group, with a power of 80% and a p <0.05. The number of participants was increased to 106 per group to allow for 3% of loss to follow-up.
Statistical analyses were performed with IBM SPSS Statistics 20.0 (IBM Inc., New York, New York). All tests were 2 sided and considered significant if <0.05. Categorical data are expressed as counts (%) and were compared using the chi-square or Fisher’s exact tests. Continuous variables are expressed as mean ± SD and were compared using Student’s t tests.
Results
The present study included 213 patients: 106 in the ticagrelor group and 107 in the prasugrel group. The 2 groups were similar in terms of baseline characteristics as summarized in Table 1 . In particular, the rate of non–ST-elevation myocardial infarction as defined by a preprocedural troponin Ic more than the ninety-ninth percentiles was similar between the 2 groups (ticagrelor vs prasugrel: 53.8% vs 45.8%; p = 0.2).
| Variables | Ticagrelor (n=106) | Prasugrel (n=107) | p value |
|---|---|---|---|
| Age (Mean ±SD) Years | 61.5 ±10.4 | 60 ± 9.6 | 0.3 |
| Men | 74 (69.8%) | 85 (79.8%) | 0.1 |
| Body Mass Index, (Kg/m 2 )(Mean ±SD) | 28.1 ± 8.1 | 28.2 ± 8.6 | 0.7 |
| Smoker | 44.9 (48%) | 38 (36.8%) | 0.2 |
| Hypercholesterolemia | 57 (53.3%) | 48 (45.3%) | 0.2 |
| Hypertension | 56 (52.8%) | 62 (57.9%) | 0.5 |
| Diabetes mellitus | 31 (29.2%) | 44 (41.1%) | 0.1 |
| Family history of coronary artery disease | 16 (15.1%) | 25 (23.4%) | 0.1 |
| Previous PCI | 13 (12%) | 13 (12%) | 1 |
| Previous MI | 12 (11%) | 13 (12%) | 0.7 |
| Previous CABG | 3 (3%) | 3 (3%) | 1 |
| Non ST-Elevation Myocardial Infarction | 57 (53.8%) | 49 (45.8%) | 0.2 |
| Leucocytes (x10 9 /l) | 8.4 ± 3.3 | 9.2 ± 3.2 | 0.3 |
| Hemoglobin (g/dl) | 13.7 ± 1.5 | 14.3 ± 1.7 | 0.01 |
| Platelets (x10 9 /l) | 230 ± 62 | 244 ± 7 | 0.2 |
| Fibrinogen (g/l) | 4 ± 1.3 | 4.1 ± 1.1 | 0.7 |
| Creatinin (μmol/l) | 86.7 ± 35.4 | 83.8 ± 37.2 | 0.6 |
| Aspirin | 64 (60.4%) | 58 (54.2%) | 0.4 |
| Beta-Blockers | 53 (50%) | 55 (51.4%) | 0.8 |
| Statins | 67 (63.2%) | 64 (59.8%) | 0.6 |
| Angiotenin Renine Blockers | 50 (47.2%) | 46 (43%) | 0.5 |
| Insulin | 6 (5.7%) | 14 (13.1%) | 0.1 |
| Oral anti-diabetics | 20 (18.9%) | 24 (22.4%) | 0.5 |
The main angiographic and interventional characteristics are depicted in Table 2 . The main characteristics of intervention were similar between the 2 groups including the number of treated vessel and rate of direct stenting (ticagrelor vs prasugrel: 1.3 ± 0.6 and 1.2 ± 0.5, p = 0.2; and 52.8% vs 52.3% p = 0.9, respectively).
| Angiography and Intervention | Ticagrelor (n=106) | Prasugrel (n=107) | p Value |
|---|---|---|---|
| Number of narrowed coronary arteries: | |||
| 1 | 56 (57%) | 57 (59%) | |
| 2 | 22 (22%) | 28 (29%) | 0.4 |
| 3 | 19 (19%) | 12 (12%) | |
| Coronary artery involved | |||
| Left main | 16 | 12 | |
| Left anterior descending | 49 | 63 | |
| Left circumflex | 39 | 23 | |
| Right | 26 | 27 | |
| Delays (hours) | |||
| Onset symptom to LD (mean ±SD) | 11 ± 12.2 | 20.5 ± 13 | <0.001 |
| Admission –PCI (mean ±SD) | 17.8 ± 8.2 | 18.2 ± 11.1 | 0.8 |
| Loading dose –PCI (mean ±SD) | 13.4 ± 8.3 | 0 | <0.001 |
| Intervention | |||
| Direct stenting | 56 (53%) | 56 (52%) | 0.9 |
| Balloon pre-dilatation | 50 (47%) | 48 (45%) | 0.7 |
| Post-dilatation | 69 (65%) | 66 (62%) | 0.9 |
| Number of treated vessels (mean ±SD) | 1.3 ± 0.6 | 1.2 ± 0.5 | 0.2 |
| Number of stents (mean ±SD) | 1.5 ± 0.7 | 1.4 ±0.7 | 0.6 |
| Drug eluting stent | 96% | 96% | 0.6 |
| Total Stent length, (mean ±SD) | 22.7 ± 11.7 | 23.5 ± 12.7 | 0.7 |
| Mean stent diameter, (mean ±SD) | 3.2± 0.5 | 3.3 ±0.8 | 0.7 |
| Bail-out Glycoprotein 2b/3a inhibitor | 0 | 5 (5%) | 0.01 |
| Emergent Percutaneous coronary intervention | 0 | 6 (6%) | 0.01 |
| Heparin | 39 (37%) | 49 (46%) | |
| Bivalirudin | 67 (63%) | 58 (54%) | 0.2 |
The time between admission to PCI was similar between the 2 groups (ticagrelor vs prasugrel: 17.8 ± 8.2 vs 18.2 ± 11.1 hours, p = 0.8). According to the treatment protocol of each group, there was a significant difference in the timing of drug intake. In the ticagrelor group, the LD was given a mean of 13.4 ± 8.3 hours before PCI.
We observed a significant difference in the rate of emergent PCI with significantly more patients requiring PCI related to recurrent ischemia during the interval between admission and scheduled PCI in the prasugrel group (ticagrelor vs prasugrel: 0% vs 5.6%, p <0.001). We observed no periprocedural complications in either groups including stent thrombosis.
In the ticagrelor group, the rate of periprocedural myonecrosis was significantly lower than in the prasugrel group (19.8% vs 38.3%, p = 0.03). Regarding the secondary end point of myocardial insults, again, the ticagrelor group had a lower rate of events (41.5% vs 71.5%, p <0.001; Figure 2 , Table 3 ). The absolute troponin level did not differ 24 hours after PCI (2.5 ± 6.3 vs 2.6 ± 8.2; p = 0.9).




