CHEST DISCOMFORT
Chest discomfort is a common challenge for clinicians in the office or emergency department. The differential diagnosis includes conditions affecting organs throughout the thorax and abdomen, with prognostic implications that vary from benign to life threatening (Table 4-1). Failure to recognize potentially serious conditions such as acute ischemic heart disease, aortic dissection, tension pneumothorax, or pulmonary embolism can lead to serious complications, including death. Conversely, overly conservative management of low-risk patients leads to unnecessary hospital admissions, tests, procedures, and anxiety.
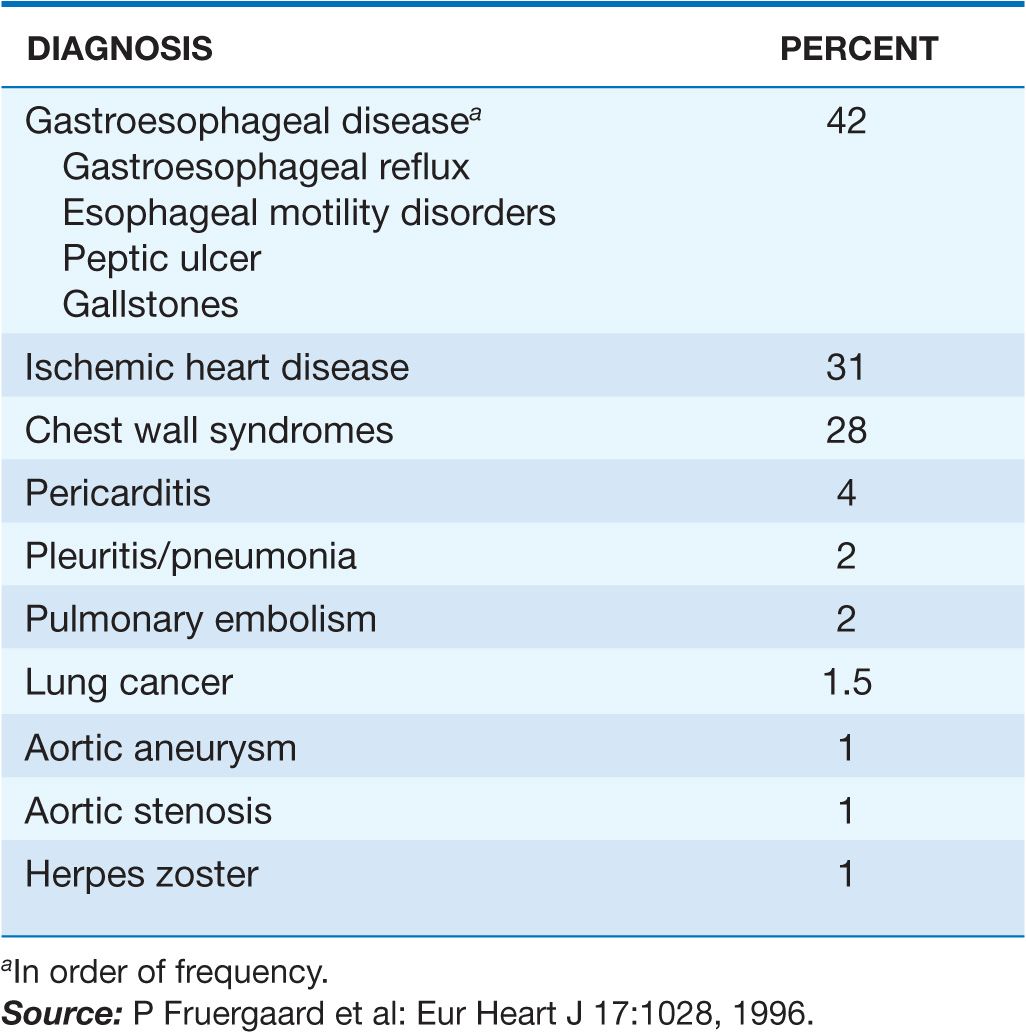
TABLE 4-1
DIAGNOSES AMONG CHEST PAIN PATIENTS WITHOUT MYOCARDIAL INFARCTION
CAUSES OF CHEST DISCOMFORT
Myocardial ischemia and injury
Myocardial ischemia occurs when the oxygen supply to the heart is insufficient to meet metabolic needs. This mismatch can result from a decrease in oxygen supply, a rise in demand, or both. The most common underlying cause of myocardial ischemia is obstruction of coronary arteries by atherosclerosis; in the presence of such obstruction, transient ischemic episodes are usually precipitated by an increase in oxygen demand as a result of physical exertion. However, ischemia can also result from psychological stress, fever, or large meals or from compromised oxygen delivery due to anemia, hypoxia, or hypotension. Ventricular hypertrophy due to valvular heart disease, hypertrophic cardiomyopathy, or hypertension can predispose the myocardium to ischemia because of impaired penetration of blood flow from epicardial coronary arteries to the endocardium.
 Angina pectoris
Angina pectoris
(See also Chap. 33) The chest discomfort of myocardial ischemia is a visceral discomfort that is usually described as a heaviness, pressure, or squeezing (Table 4-2). Other common adjectives for anginal pain are burning and aching. Some patients deny any “pain” but may admit to dyspnea or a vague sense of anxiety. The word “sharp” is sometimes used by patients to describe intensity rather than quality.
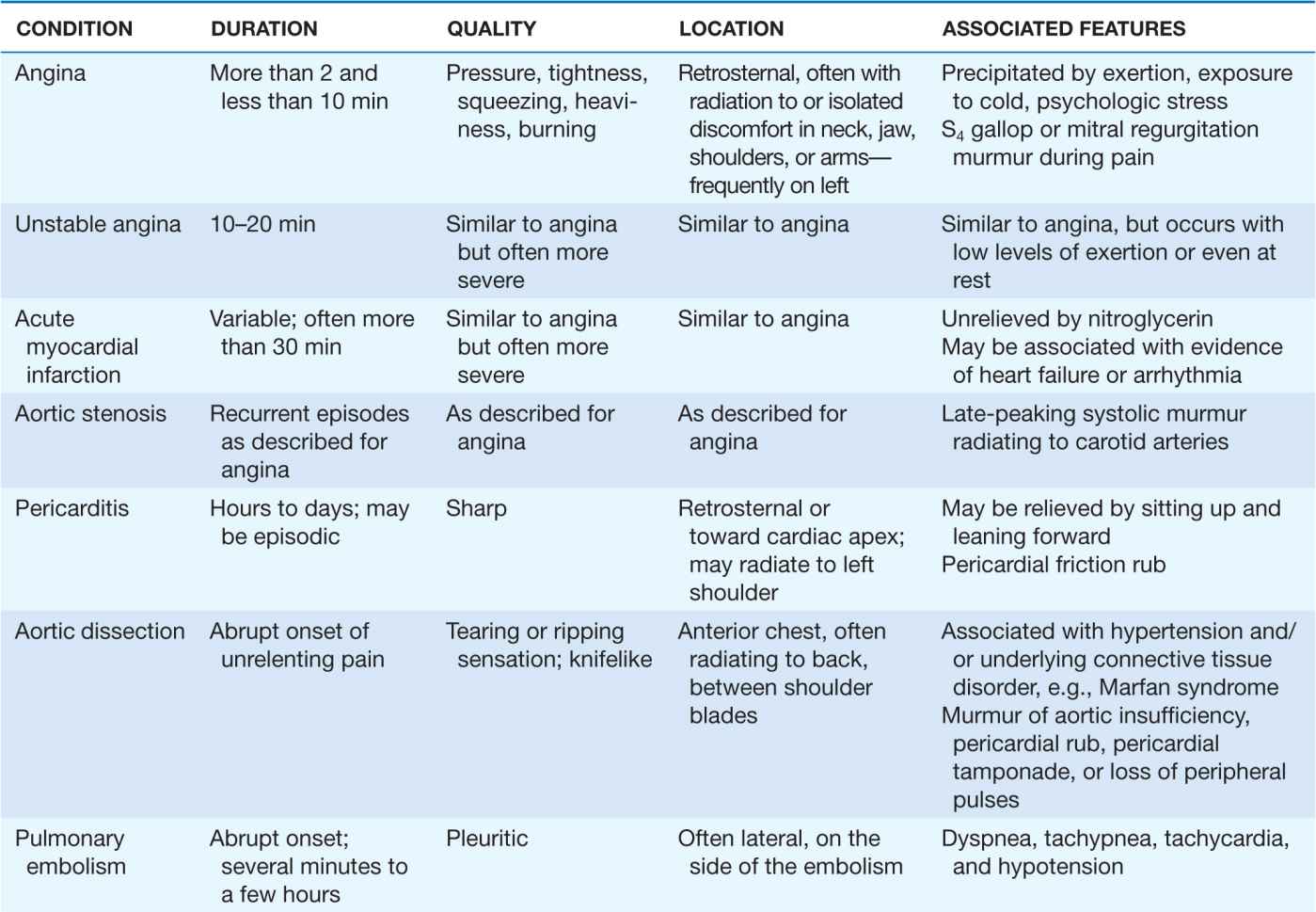
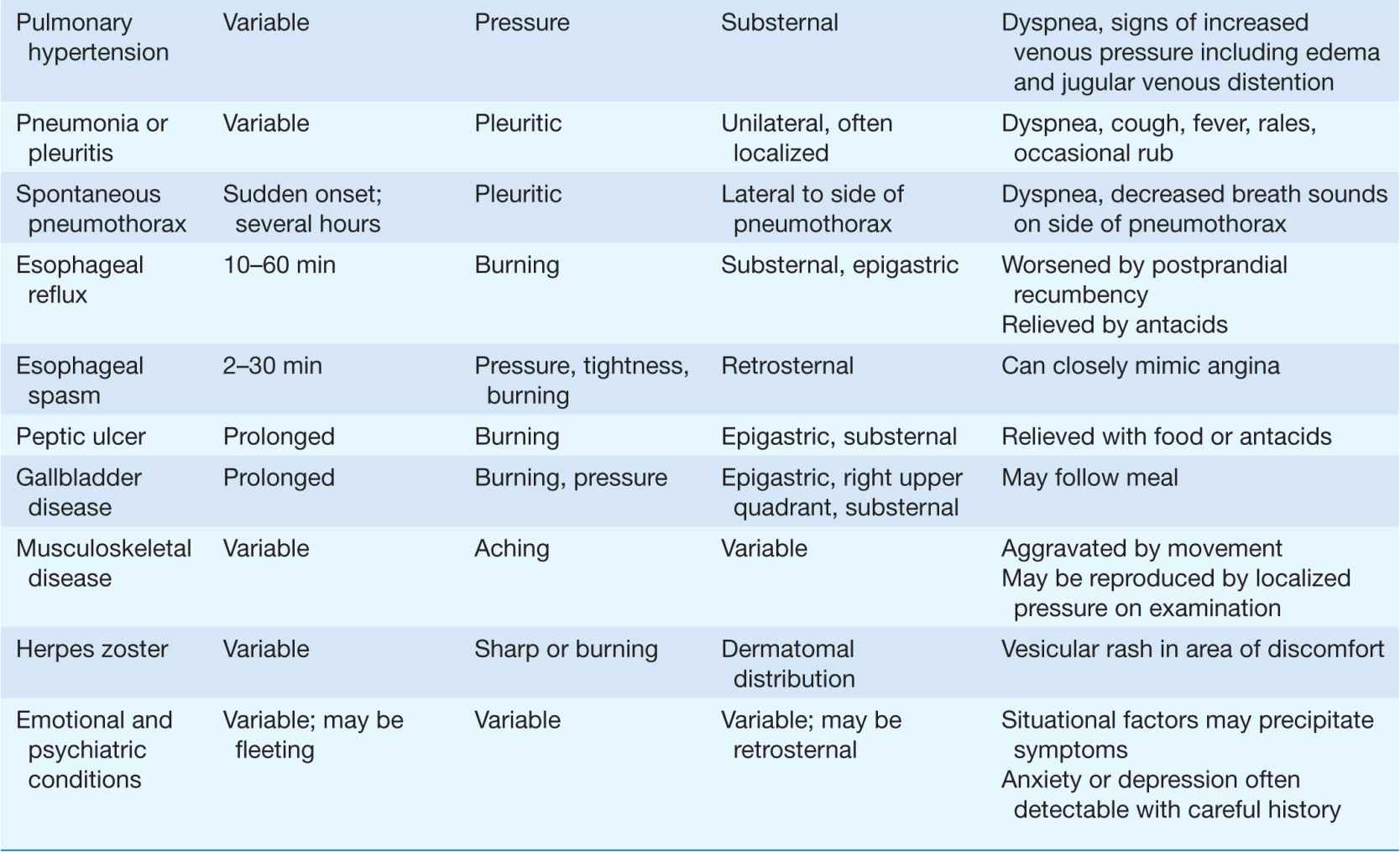
TABLE 4-2
TYPICAL CLINICAL FEATURES OF MAJOR CAUSES OF ACUTE CHEST DISCOMFORT
The location of angina pectoris is usually retrosternal; most patients do not localize the pain to any small area. The discomfort may radiate to the neck, jaw, teeth, arms, or shoulders, reflecting the common origin in the posterior horn of the spinal cord of sensory neurons supplying the heart and these areas. Some patients present with aching in sites of radiated pain as their only symptoms of ischemia. Occasional patients report epigastric distress with ischemic episodes. Less common is radiation to below the umbilicus or to the back.
Stable angina pectoris usually develops gradually with exertion, emotional excitement, or after heavy meals. Rest or treatment with sublingual nitroglycerin typically leads to relief within several minutes. In contrast, pain that is fleeting (lasting only a few seconds) is rarely ischemic in origin. Similarly, pain that lasts for several hours is unlikely to represent angina, particularly if the patient’s electrocardiogram (ECG) does not show evidence of ischemia.
Anginal episodes can be precipitated by any physiologic or psychological stress that induces tachycardia. Most myocardial perfusion occurs during diastole, when there is minimal pressure opposing coronary artery flow from within the left ventricle. Since tachycardia decreases the percentage of the time in which the heart is in diastole, it decreases myocardial perfusion.
 Unstable angina and myocardial infarction
Unstable angina and myocardial infarction
(See also Chaps. 34 and 35) Patients with these acute ischemic syndromes usually complain of symptoms similar in quality to angina pectoris, but more prolonged and severe. The onset of these syndromes may occur with the patient at rest, or awakened from sleep, and sublingual nitroglycerin may lead to transient or no relief. Accompanying symptoms may include diaphoresis, dyspnea, nausea, and light-headedness.
The physical examination may be completely normal in patients with chest discomfort due to ischemic heart disease. Careful auscultation during ischemic episodes may reveal a third or fourth heart sound, reflecting myocardial systolic or diastolic dysfunction. A transient murmur of mitral regurgitation suggests ischemic papillary muscle dysfunction. Severe episodes of ischemia can lead to pulmonary congestion and even pulmonary edema.
 Other cardiac causes
Other cardiac causes
Myocardial ischemia caused by hypertrophic cardiomyopathy or aortic stenosis leads to angina pectoris similar to that caused by coronary atherosclerosis. In such cases, a loud systolic murmur or other findings usually suggest that abnormalities other than coronary atherosclerosis may be contributing to the patient’s symptoms. Some patients with chest pain and normal coronary angiograms have functional abnormalities of the coronary circulation, ranging from coronary spasm visible on coronary angiography to abnormal vasodilator responses and heightened vasoconstrictor responses. The term “cardiac syndrome X” is used to describe patients with angina-like chest pain and ischemic-appearing ST-segment depression during stress despite normal coronary arteriograms. Some data indicate that many such patients have limited changes in coronary flow in response to pacing stress or coronary vasodilators.
Pericarditis
(See also Chap. 22) The pain in pericarditis is believed to be due to inflammation of the adjacent parietal pleura, since most of the pericardium is believed to be insensitive to pain. Thus, infectious pericarditis, which usually involves adjoining pleural surfaces, tends to be associated with pain, while conditions that cause only local inflammation (e.g., myocardial infarction or uremia) and cardiac tamponade tend to result in mild or no chest pain.
The adjacent parietal pleura receives its sensory supply from several sources, so the pain of pericarditis can be experienced in areas ranging from the shoulder and neck to the abdomen and back. Most typically, the pain is retrosternal and is aggravated by coughing, deep breaths, or changes in position—all of which lead to movements of pleural surfaces. The pain is often worse in the supine position and relieved by sitting upright and leaning forward. Less common is a steady aching discomfort that mimics acute myocardial infarction.
Diseases of the aorta
(See also Chap. 38) Aortic dissection is a potentially catastrophic condition that is due to spread of a subintimal hematoma within the wall of the aorta. The hematoma may begin with a tear in the intima of the aorta or with rupture of the vasa vasorum within the aortic media. This syndrome can occur with trauma to the aorta, including motor vehicle accidents or medical procedures in which catheters or intraaortic balloon pumps damage the intima of the aorta. Nontraumatic aortic dissections are rare in the absence of hypertension and/or conditions associated with deterioration of the elastic or muscular components of the media within the aorta’s wall. Cystic medial degeneration is a feature of several inherited connective tissue diseases, including Marfan and Ehlers-Danlos syndromes. About half of all aortic dissections in women under 40 years of age occur during pregnancy.
Almost all patients with acute dissections present with severe chest pain, although some patients with chronic dissections are identified without associated symptoms. Unlike the pain of ischemic heart disease, symptoms of aortic dissection tend to reach peak severity immediately, often causing the patient to collapse from its intensity. The classic teaching is that the adjectives used to describe the pain reflect the process occurring within the wall of the aorta—“ripping” and “tearing”—but more recent data suggest that the most common presenting complaint is sudden onset of severe, sharp pain. The location often correlates with the site and extent of the dissection. Thus, dissections that begin in the ascending aorta and extend to the descending aorta tend to cause pain in the front of the chest that extends into the back, between the shoulder blades.
Physical findings may also reflect extension of the aortic dissection that compromises flow into arteries branching off the aorta. Thus, loss of a pulse in one or both arms, cerebrovascular accident, or paraplegia can all be catastrophic consequences of aortic dissection. Hematomas that extend proximally and undermine the coronary arteries or aortic valve apparatus may lead to acute myocardial infarction or acute aortic insufficiency. Rupture of the hematoma into the pericardial space leads to pericardial tamponade.
Another abnormality of the aorta that can cause chest pain is a thoracic aortic aneurysm. Aortic aneurysms are frequently asymptomatic but can cause chest pain and other symptoms by compressing adjacent structures. This pain tends to be steady, deep, and sometimes severe.
Pulmonary embolism
Chest pain due to pulmonary embolism is believed to be due to distention of the pulmonary artery or infarction of a segment of the lung adjacent to the pleura. Massive pulmonary emboli may lead to substernal pain that is suggestive of acute myocardial infarction. More commonly, smaller emboli lead to focal pulmonary infarctions that cause pain that is lateral and pleuritic. Associated symptoms include dyspnea and, occasionally, hemoptysis. Tachycardia is usually present. Although not always present, certain characteristic ECG changes can support the diagnosis.
Pneumothorax
Sudden onset of pleuritic chest pain and respiratory distress should lead to consideration of spontaneous pneumothorax, as well as pulmonary embolism. Such events may occur without a precipitating event in persons without lung disease, or as a consequence of underlying lung disorders.
Pneumonia or pleuritis
Lung diseases that damage and cause inflammation of the pleura of the lung usually cause a sharp, knifelike pain that is aggravated by inspiration or coughing.
Gastrointestinal conditions
Esophageal pain from acid reflux from the stomach, spasm, obstruction, or injury can be difficult to differentiate from myocardial syndromes. Acid reflux typically causes a deep burning discomfort that may be exacerbated by alcohol, aspirin, or some foods; this discomfort is often relieved by antacid or other acid-reducing therapies. Acid reflux tends to be exacerbated by lying down and may be worse in early morning when the stomach is empty of food that might otherwise absorb gastric acid.
Esophageal spasm may occur in the presence or absence of acid reflux and leads to a squeezing pain indistinguishable from angina. Prompt relief of esophageal spasm is often provided by antianginal therapies such as sublingual nifedipine, further promoting confusion between these syndromes. Chest pain can also result from injury to the esophagus, such as a Mallory-Weiss tear caused by severe vomiting.
Chest pain can result from diseases of the gastrointestinal tract below the diaphragm, including peptic ulcer disease, biliary disease, and pancreatitis. These conditions usually cause abdominal pain as well as chest discomfort; symptoms are not likely to be associated with exertion. The pain of ulcer disease typically occurs 60 to 90 min after meals, when postprandial acid production is no longer neutralized by food in the stomach. Cholecystitis usually causes a pain that is described as aching, occurring an hour or more after meals.
Neuromusculoskeletal conditions
Cervical disk disease can cause chest pain by compression of nerve roots. Pain in a dermatomal distribution can also be caused by intercostal muscle cramps or by herpes zoster. Chest pain symptoms due to herpes zoster may occur before skin lesions are apparent.
Costochondral and chondrosternal syndromes are the most common causes of anterior chest musculoskeletal pain. Only occasionally are physical signs of costochondritis such as swelling, redness, and warmth (Tietze’s syndrome) present. The pain of such syndromes is usually fleeting and sharp, but some patients experience a dull ache that lasts for hours. Direct pressure on the chondrosternal and costochondral junctions may reproduce the pain from these and other musculoskeletal syndromes. Arthritis of the shoulder and spine and bursitis may also cause chest pain. Some patients who have these conditions and myocardial ischemia blur and confuse symptoms of these syndromes.
Emotional and psychiatric conditions
As many as 10% of patients who present to emergency departments with acute chest discomfort have panic disorder or other emotional conditions. The symptoms in these populations are highly variable, but frequently the discomfort is described as visceral tightness or aching that lasts more than 30 min. Some patients offer other atypical descriptions, such as pain that is fleeting, sharp, and/or localized to a small region. The ECG in patients with emotional conditions may be difficult to interpret if hyperventilation causes ST-T-wave abnormalities. A careful history may elicit clues of depression, prior panic attacks, somatization, agoraphobia, or other phobias.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


