Chapter 97
Cerebrovascular Disease
General Considerations
Caron B. Rockman, Thomas S. Maldonado
Based on a chapter in the seventh edition by William C. Mackey
Although the descriptions of extracranial vascular disease span many centuries, stroke was largely believed until fairly recently to be a result of intracranial pathology. Indeed, in the seventh edition of his textbook The Principles and Practice of Medicine, published in 1909, William Osler1 attributed stroke mainly to intracranial hemorrhage or vasospasm and makes no mention of carotid or vertebral occlusive disease in this section. Yet the relationship between extracranial carotid disease and stroke had been described as early as 1875, when Gowers2 reported on a patient with carotid occlusion, left visual loss, and right hemiplegia. Subsequently, in 1905, Chiari3 studied 400 consecutive autopsies and discovered thrombus superimposed on carotid artery atherosclerotic plaque in seven patients, four of whom had suffered embolic strokes. This important observation represented the first pathophysiologic description linking carotid plaque atheroemboli to ischemic stroke. Perhaps the greatest breakthrough in the study of the mechanism of cerebrovascular disease was C. Miller Fisher’s4,5 publications of his clinicoanatomic correlations on occlusion of the carotid arteries in 1951 and 1954. He described the atherosclerotic plaque as the culprit lesion in carotid artery disease and importantly noted that the distal internal carotid artery is usually free of disease, raising the possibility of surgical bypass to a healthy target vessel.
Fisher’s prediction of surgical treatment for carotid atherosclerosis was soon realized. In 1954, Eastcott et al6 reported on the first successful carotid surgery for occlusive disease, in which the carotid bifurcation was resected and in-line flow restored via a common carotid to internal carotid artery anastomosis. The first successful carotid endarterectomy (CEA) was performed by DeBakey in 1953, who reported a 19-year symptom-free follow-up in the Journal of the American Medical Association in 1975.7,8
Carotid endarterectomy became both more standardized and frequently performed, with up to 107,000 procedures performed annually by 1985. This trend was tempered by critics who viewed inconsistent results among centers and poor patient selection as leading to its misuse and overuse. The precise role for this operation in the treatment of cerebrovascular disease remained controversial until the early 1990s, when clinical trials showed its safety and effectiveness in both symptomatic and certain asymptomatic patients.9–13 Ultimately, although the pathophysiology of carotid atherosclerotic plaque as it relates to cerebral ischemia appears certain, surgical and medical advances, most notably endovascular techniques and the promise of statin medications, continue to challenge the role of endarterectomy as the mainstay of treatment in the prevention of ischemic stroke due to extracranial cerebrovascular disease.
Epidemiology
Stroke, or cerebral infarction, is the acute development of a focal neurologic deficit caused by the disruption of blood supply to an area of the brain. Strokes can be ischemic, due to occlusion of a blood vessel, or hemorrhagic, due to rupture of a blood vessel. Hemorrhagic strokes include both intracerebral hemorrhage, which is bleeding within the brain parenchyma, and subarachnoid hemorrhage, which is bleeding in the subarachnoid space.14 With regard to the vascular surgical management of stroke, the prevention of ischemic stroke is the prime area of consideration. The majority of strokes in the United States, about 87%, are ischemic in etiology.14 A major preventable cause of ischemic stroke is atherosclerotic occlusive disease of the extracranial carotid artery.
Prevalence of Stroke
Stroke is among the major causes of mortality and disabilities in the world.15 The overall stroke prevalence or proportion of the population affected by stroke, relative to the population as a whole in the United States during the years 2005 through 2008 was approximately 3.0%. The prevalence of clinically silent cerebral infarction is estimated to range from 6% to 28%.16–19 Projections show that by 2030, an additional 4 million people will have had a stroke, a 24.9% increase in prevalence from 2010.16,20
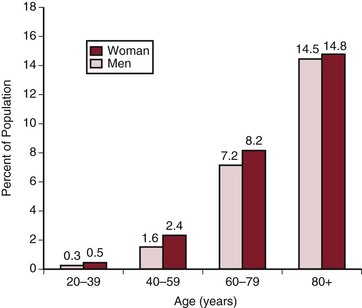
The prevalence of stroke varies with the population studied, and is related to age, ethnicity, sex, and risk factor profile16 (Fig. 97-1). The prevalence of ischemic stroke increases with age. In the United States, the prevalence of stroke varies by race and ethnicity, being 6% among American Indian/Alaska Native populations, 4.0% among blacks, 2.6% among Hispanics, 2.3% among whites, and 1.6% among Asians.21
Incidence of Stroke
In contrast to prevalence, the incidence of stroke is the rate at which new cases occur in a population over a specified period. Each year in the United States approximately 800,000 people experience a new or recurrent stroke16 (Fig. 97-2). Approximately 610,000 of these are initial episodes of stroke, and an additional 185,000 are recurrent strokes.16 Of all strokes, approximately 87% are ischemic, 10% are due to intracerebral hemorrhage, and 3% result from subarachnoid hemorrhage.16 Although women have a lower age-adjusted stroke incidence than men, women have a higher lifetime risk of stroke than men because of longer life expectancy.16,22,23 The risk of first-ever stroke in blacks is twice that in whites.16,24 Data from the Framingham Heart Study indicate that the age-adjusted incidences of clinical stroke per 1000 person-years in 1950 through 1977, 1978 to 1989 and 1990 to 2004 were 7.6, 6.2, and 5.3 in men and 6.2, 5.8 and 5.1 in women, respectively.25 This study additionally suggests that stroke incidence is declining over time in this largely white cohort.26 Unfortunately, a similar decline was not noted in blacks.
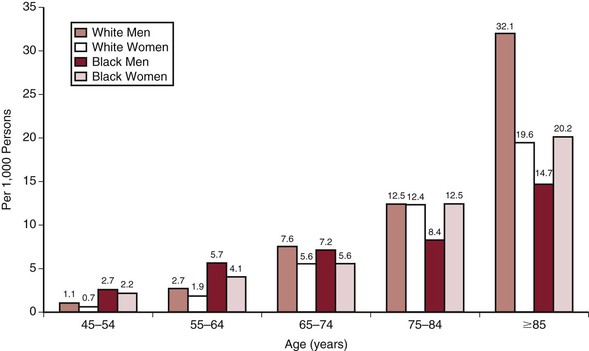
Figure 97-2 Annual incidence of first cerebral infarction by age, sex, and race (Greater Cincinnati/Northern Kentucky Stroke Study: 1999). Rates for black men and women 45 to 54 years of age and for black men ≥75 years of age are considered unreliable. (Unpublished data from the Greater Cincinnati/Northern Kentucky Stroke Study. Reprinted from Roger VL, et al: Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 125:e2-e220, 2012.)
Possible Decreases in Prevalence and Incidence of Stroke
In December 2010, the Centers for Disease Control and Prevention announced that stroke was now the fourth leading cause of death in the United States, down from the third place ranking it had held for decades.27,28 Several additional population-based studies have tracked stroke incidence in recent decades.29 Rothwell et al30 reported a decrease in stroke incidence of nearly 40% between the 1980s and the year 2002 in the United Kingdom. In the United States, the Framingham cohort study also found that the incidence of stroke has been declining over the past 50 years.25 In contrast to the prior study, the Minnesota Stroke Study noted that the incidence of stroke was stable in both men and women between the years 1990 and 2000.31
A review article by Zhang et al32 addressed the possible decreasing incidence of stroke in the United States in addition to several European countries. It is noted that the prevalences of stroke reported in the United States by the Centers for Disease Control Behavioral Risk Factor Surveillance System in the years 2005 and 2008 were equivalent at 2.6%. After a comprehensive review of multiple population-based studies, the Zhang investigators concluded that they were unable to prove or disprove the notion that the prevalence or incidence of stroke may be decreasing. However, they expressed the belief that there was abundant evidence that the mortality attributable to acute stroke is decreasing, likely related to improvements in acute stroke treatment.32 They further noted that an increase in the burden of stroke due to the aging populations of both the United States and European countries was to be expected.
Effect of Improved Medical Therapy on the Reduced Incidence of Stroke
The possible effect of improved modern medical therapy on the decreased incidence of stroke has received great attention. Previous randomized trials have demonstrated a clear benefit of surgical therapy with CEA over contemporaneous medical therapy with regard to stroke prevention in both asymptomatic and previously symptomatic patients with severe extracranial internal carotid artery (ICA) stenosis.11,13 Some later analyses have reported that the annual risk of stroke in patients with asymptomatic ICA stenosis is lower than that reported in the CEA trials, presumably as a result of improved medical therapy.33,34 This concept is covered in detail in Chapter 99. Nevertheless, it is clear that asymptomatic ICA stenosis continues to cause a meaningful number of strokes.35 Data from the Greater Cincinnati/Northern Kentucky Stroke Study has resulted in conservative estimates that about 41,000 strokes may be attributed to previously asymptomatic extracranial ICA stenosis annually in the United States.35
The epidemiologic association between elevated cholesterol and stroke is inconsistent and somewhat controversial.36 Nevertheless, treatment with statins has generally been associated with stroke reduction, including in a meta-analysis of more than 90,000 patients.37 It should be noted that many of the studies included in this meta-analysis involved secondary stroke prevention. Nevertheless, the relative stroke risk reduction was found to be 21%. Fatal strokes were reduced, but not significantly, by 9%. Statins have additionally been demonstrated to reduce strokes in a variety of patient populations, including those with known coronary artery disease,38 hypercholesterolemia,38 and normocholesterolemia,38 those who are elderly,38 and those with diabetes.39 Statins have also been demonstrated to consistently reduce carotid intima-media thickness (CIMT).40 Finally, a 2013 meta-analysis involving more than 113,000 patients has shown that the use of statin therapy at stroke onset is associated with improved late outcome, including both rates of functional independence and survival.41 Although data regarding the utility of statin medications for the primary prevention of stroke are less conclusive than for secondary prevention, current guidelines do in fact recommend statins for the prevention of first stroke in high-risk patients, including those with low-density lipoprotein (LDL) cholesterol levels higher than 4.1 mg/dL as well as for men older than 45 years and for women older than 55 years with any of the following risk factors: a positive family history, smoking, hypertension, and left ventricular hypertrophy.36
Types of Strokes and Relationship of Stroke to Carotid Artery Atherosclerosis
There are five general categories of ischemic stroke, according to the TOAST (Trial of ORG 10172 in Acute Stroke Treatment) classification: cardioembolic strokes, large vessel disease strokes, small vessel disease strokes, strokes related to unusual causes, and strokes of undetermined etiology. 42 This classification is based on clinical and radiologic findings as well as results of additional investigations such as duplex ultrasonography, electrocardiogram (ECG) analysis, echocardiography, and blood tests. However, most detailed studies on stroke subtype fail to identify a definitive cause of stroke in at least 25% to 39% of patients.43 Traditionally it has been estimated that large vessel disease caused stroke in 50% of cases.43 Later studies, however, have shown that small vessel disease is more frequent, and large vessel disease less frequent, than previously estimated.44
In the Rochester Epidemiology Project, 442 patients who had a first ischemic stroke from 1985 through 1989 in Rochester, Minnesota, were evaluated. Four major categories were identified: large vessel cervical or intracranial (16.7%), cardioembolic (29.9%), lacunar (16.3%), and of uncertain cause (37.1%). (Lacunar strokes are discussed in more detail later, in “Clinical Findings in Patients with Cerebrovascular Disease”). Therefore, the large vessel cervical etiology accounted for approximately 16% of all ischemic strokes and for 27% of strokes with determined causes. Patients with these categories of stroke had the highest rates of recurrent stroke at 30 days (18.5%).45
In another study, patients with first-ever or recurrent ischemic stroke in the greater Cincinnati area were identified during the year 2005.35 This study reported 2204 ischemic strokes, including 365 (16.6%) of the large vessel subtype. Carotid artery stenosis was associated with 8% of all ischemic strokes, whereas ICA occlusion was associated with an additional 3.5%. The annual rate of first-ever and recurrent strokes attributed to the extracranial carotid artery was 13.4 per 100,000 persons. On the basis of this analysis, the researchers conservatively estimated that about 41,000 strokes per year in the United States may be attributed to extracranial ICA stenosis alone (without consideration of additional strokes related to carotid artery occlusion).35
Most prior studies on this topic have examined patients who have sustained strokes and have tried to ascertain the etiology of the cerebrovascular events. An additional study took an alternative approach by monitoring a group of patients with known unilateral asymptomatic carotid artery stenosis and analyzing the types of strokes that occurred in these patients.46 The risk of stroke at 5 years in 1820 patients increased with the severity of stenosis; it reached 3.2% annually among the 216 patients with 60% to 99% stenosis. Among this cohort, however, the 5-year risk of a stroke in the territory of a large artery was 9.9%, that of lacunar stroke was 6%, and that of cardioembolic stroke was 2.1%. Risk factors for large artery stroke included silent brain infarction, a history of diabetes, and a higher severity of stenosis. The study concluded therefore, that 45% of strokes in patients with asymptomatic stenosis of 60% to 99% are attributable to either lacunar strokes or cardioembolism, and not a direct result of large artery disease.
Racial differences have been noted in stroke subtypes.47 Of patients suffering ischemic stroke, large vessel strokes were believed to account for 10% in black patients and 12% in white patients. However, stroke cause was judged to be undetermined in approximately 50% of both racial groups. Only 60% of patients in both racial groups underwent a carotid duplex ultrasonography examination, and only 3% to 5% underwent a cerebral angiogram.
On the basis of these and other studies, and in consideration of the fact that most studies on this topic fail to determine with certainty the etiology of ischemic stroke in a high percentage of cases, most experts in this field believe that at least 20% of ischemic strokes are likely related to extracranial carotid artery atherosclerosis. Carotid artery stenosis typically causes strokes in the territories of the anterior cerebral artery (ACA) or the middle cerebral artery (MCA).
Risk Factors for Stroke
The risk factors for ischemic stroke include many of the risk factors for generalized atherosclerosis, as listed here and shown in Figure 97-314,16,48 In addition to these risk factors for ischemic stroke, prior transient ischemic attack (TIA) and carotid artery atherosclerosis represent major clinical risk factors for future ischemic stroke.
Age: For each decade after 55 years of age, the risk of stroke approximately doubles.49
Sex: Ischemic stroke is in general more prevalent in men than in women.50 However, women tend to account for a higher percentage of stroke mortalities, likely because of their greater longevity.14
Race: The risk of first-ever stroke in blacks and Hispanics have is approximately twice that of whites.51
Hypertension: Appropriate treatment of blood pressure in hypertensive patients is associated with a significant reduction in the risk of ischemic stroke; the lifetime risk of stroke in patients with a blood pressure less than 120 mm Hg systolic/80 mm Hg diastolic (120/80) is half that of subjects with hypertension.16,52
Family history: A parental history of stroke, transient ischemic attack, or myocardial infarction is associated with a 1.4- to 3.3-fold increased risk of stroke.53
Atrial fibrillation: Patients with atrial fibrillation have a threefold to fivefold increased risk of cardioembolic ischemic stroke.54
Cigarette smoking: Current cigarette smokers have a two to four times higher risk of stroke than with nonsmokers and smokers who have not smoked for more than 10 years.16,55,56
Hypercholesterolemia: Trials specific to ischemic stroke have demonstrated that there may be a 25% higher risk of ischemic stroke with each 38.7-mg/dL increase in total cholesterol levels.57 However, not all trials have consistently demonstrated a correlation between hypercholesterolemia and ischemic stroke.14
Physical activity: Increased leisure time physical activity is protective against stroke across all race, sex and age categories, the protective effect being related to the level of intensity and the duration of activity.58
Diabetes: Diabetes mellitus nearly doubles the risk of stroke in patients with normal glucose levels.59
Diet: A protective relationship between fruit and vegetable consumption and decreased ischemic stroke risk has been reported.60
Obesity: Obesity is a specific risk factor for ischemic stroke in both men and women.61,62 There is an additional association between abdominal obesity and ischemic stroke in men.63
Alcohol: There is a reported increased risk of ischemic stroke with “irregular” drinking, including heavy and binge drinking.64 However, moderate drinking may be associated with a decreased risk of ischemic stroke.65
Renal insufficiency: Mild to moderate renal insufficiency is an independent predictor of ischemic stroke in both asymptomatic patients and patients with peripheral arterial disease.66–68
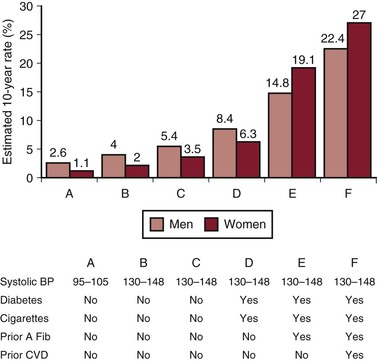
Figure 97-3 Estimated 10-year stroke risk in a 55-year-old adult according to risk factors (Framingham Heart Study). A fib, Atrial fibrillation; BP, blood pressure; CVD, cardiovascular disease. (From Roger VL, et al: Heart disease and stroke statistics—2012 update: a report from the American Heart Association. Circulation 125:e2-e220, 2012.)
The INTERSTROKE Study, published in 2010, reported a case-control study of 2337 ischemic stroke cases in 22 countries worldwide. Patients with an acute first stroke were compared with controls with no history of stroke, who were matched for both age and sex.48 The investigators found that five factors accounted for more than 80% of the global risk of all ischemic strokes: hypertension, current smoking, abdominal obesity, diet, and physical inactivity.48 Hypertension was the most important risk factor for all stroke subtypes.48,69
Incidence of Transient Ischemic Attack
A transient ischemia attack is a neurologic event that manifests as stroke-like symptoms lasting less than 24 hours. (The clinical findings in TIAs are discussed in detail later.) The estimated annual incidence of self-reported physician-diagnosed TIA in the United States is approximately 2.3%, but the true incidence is likely higher.16,70 Patients who have had a TIA are at significantly increased risk of a subsequent ischemic stroke. Approximately 15% of ischemic strokes are heralded by a prior TIA.16,71 TIAs confer a substantial short-term risk of ischemic stroke, hospitalization for cardiovascular disease–related events, and death. In one study, 10% of patients with TIA experienced a stroke within 90 days, and 5% within 2 days. Independent predictors of stroke following a TIA included age higher than 60 years, diabetes mellitus, the presence of focal symptoms, and TIAs that lasted more than 10 minutes.16,70 Individuals who have a TIA and survive the initial high-risk period have a 10-year stroke risk of about 19%.16,72 Approximately one third of episodes characterized as TIAs according to the clinical definition would probably be considered cerebral infarctions on the basis of diffusion-weighted magnetic resonance imaging (MRI) findings.16,73 Because of the substantial risk of ischemic stroke following a TIA, patients should be expediently evaluated for the presence of significant carotid artery disease.
Prevalence of Carotid Artery Disease
As with atherosclerosis in other vascular territories, cerebrovascular disease, particularly in the extracranial carotid artery, is relatively prevalent in the general population. Several large population studies have been reported. In the Tromsø Study involving nearly 7000 adults aged 25 to 84 years, ICA stenosis was detected in 3.8% of men and 2.7% of women. The prevalence increased with age, total cholesterol, systolic blood pressure, and cigarette use.74 In another population-based study of older healthy patients aged 60 to 79 years, the prevalence of ICA stenosis found by duplex ultrasonographic examination was 10.5% in men and 5.5% in women.75
In a screening program of asymptomatic patients in the United States for treatable causes of ischemic stroke, 610 patients were evaluated. Unilateral or bilateral ICA stenosis of 50% or greater was detected in 66 patients (10.8%). The finding of occult ICA stenosis was more frequent than that of new hypertension (2.6%) or new atrial fibrillation (0.5%); therefore, ICA stenosis was the most frequently detected treatable cause of ischemic stroke. Patients with known hypertension were significantly more likely to have ICA stenosis (12.7% vs. 7.8%), as were patients with heart disease (18.2% vs. 8%). Patients with both risk factors were significantly more likely to have ICA stenosis than patients without either risk factor (22.1% vs. 8.5%; P < .0001).76
Finally, in an analysis of nearly 3 million patients in the United States who underwent voluntary screening for vascular disease, 2.4% were found to have ICA stenosis. Independent risk factors for ICA stenosis included advanced age, smoking, peripheral arterial disease, hypertension, coronary artery disease, diabetes, hypercholesterolemia, and abdominal aortic aneurysm. Exercise and the consumption of fruit, vegetables, and nuts were noted to have a modest protective effect.77
An additional study from the same database reported that women had a 3.4% prevalence of ICA stenosis of 50% or greater severity, while men had a 4.2% prevalence.78 Prevalence increased dramatically with age (Fig. 97-4). It was also noted that the prevalence of ICA stenosis varied significantly by race. Native American subjects had the highest prevalence of ICA stenosis across all age ranges and in both sexes, whereas white subjects had the second highest prevalence of ICA stenosis across most age ranges and in both sexes. African American males and Asian women appeared to have the lowest prevalence (Figs. 97-5 and 97-6).
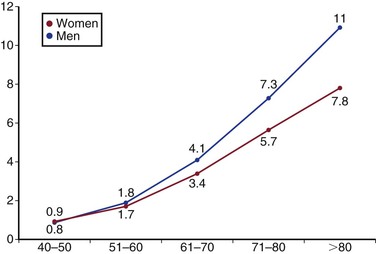
Figure 97-4 Relationship between age, sex, and prevalence of carotid artery stenosis of ≥ 50% severity. (From Rockman CB, et al: The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg 57:327-337, 2012.)
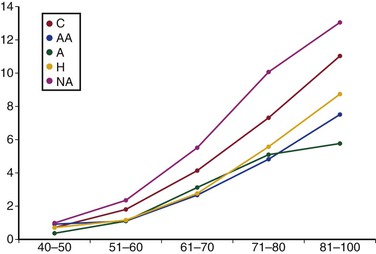
Figure 97-5 Relationship between age and the prevalence of carotid artery stenosis of ≥ 50% severity in male subjects. A, Asian; AA, African American; C, Caucasian; H, Hispanic; NA, Native American. (From Rockman CB, et al: The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg 57:327-337, 2012.)
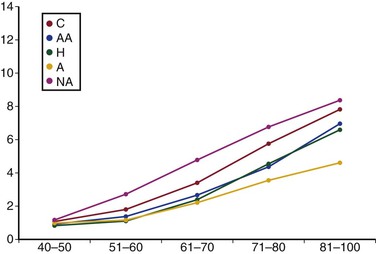
Figure 97-6 Relationship between age and the prevalence of carotid artery stenosis of ≥ 50% severity in female subjects. A, Asian; AA, African American; C, Caucasian; H, Hispanic; NA, Native American. (From Rockman CB, et al: The prevalence of carotid artery stenosis varies significantly by race. J Vasc Surg 57:327-337, 2012.)
In patients with ICA stenosis, the treatment of risk factors, including hypertension, diabetes, and lipid disorders, as well as lifestyle modifications, particularly smoking cessation, are of utmost importance.79,80 Medical therapy of ICA stenosis includes treatment of hypertension with a target blood pressure less than 140/90 mm Hg and statin therapy with a goal of decreasing LDL cholesterol level to less than 100 mg/dL and triglycerides level to less than 150 mg/dL and increasing high-density lipoprotein (HDL) level to more than 40 mg/dL. Statins lower stroke risk by approximately 30% and likely work by improving plaque stabilization.81 Antiplatelet therapy in the form of aspirin is also recommended for all patients with asymptomatic ICA stenosis.82 Some studies have reported that the combination of aspirin and clopidogrel may be more effective than aspirin alone, but larger trials have not confirmed the benefit of adding clopidogrel.83 Further details regarding the medical management of carotid artery disease are discussed in Chapter 99.
The presence of significant atherosclerotic disease at the carotid artery bifurcation is believed to represent a major treatable risk factor for future stroke, and the pathophysiologic mechanisms underlying this process are discussed in the next section of this chapter. The specific risks of stroke associated with varying degrees of carotid artery disease, the natural history of extracranial cerebrovascular disease, and the results of the randomized trials of medical versus surgical and interventional treatments of extracranial cerebrovascular disease are discussed in detail in Chapter 99.
Outcome of Stroke and Stroke Mortality
Following an ischemic stroke, the risk of recurrent ischemic stroke is 2% at 7 days, 4% at 30 days, 12% at 1 year, and 29% at 5 years.84 The risk of death after an initial ischemic stroke is 7% at 7 days, 14% at 30 days, 27% at 1 year, and 53% at 5 years.84 Someone in the United States dies every 4 minutes from a stroke.16,85 Strokes account for 1 out of every 18 deaths in the United States.16,85 When considered separately from other cardiovascular diseases, stroke currently ranks fourth among all causes of death, behind heart disease, cancer, and chronic lower respiratory disease.16,85 Stroke death rates appear to be decreasing; from 1998 to 2008 the actual number of stroke deaths declined 19.4%.16,86
Stroke is the leading cause of serious long-term disability in the United States.16,87 Among ischemic stroke survivors who were 65 years or older, the following disabilities were observed at 6 months after a stroke: 50% had hemiparesis, 30% were unable to walk without some assistance, 26% were dependent in activities of daily living, 19% had aphasia, 35% had depressive symptoms, and 26% were institutionalized.16,88 Finally, a contemporary perspective on the impact of stroke is available from the CREST (Carotid Revascularization Endarterectomy Versus Stenting Trial) data89; although few of the strokes related to either CEA or carotid artery angioplasty and stenting were major in extent, the estimated 4-year mortality for patients who experienced stroke was 21.1% compared with 11.6% for those without stroke. The adjusted risk of death at 4 years was higher after periprocedural stroke (hazard ratio, 2.78).
Cost of Caring for Patients with Stroke
The estimated total direct and indirect cost of stroke in the United States in 2008 was 34.3 billion dollars.16 The direct costs, 18.8 billion dollars, included hospital outpatient or office provider visits, hospital inpatient stays, emergency department visits, medicines, and home health care.16,90 The total cost of stroke from 2005 to 2050 is projected to be approximately 1.52 trillion dollars for non-Hispanic white patients, 313 billion dollars for Hispanic patients, and 379 billion dollars for black patients.16,91
Treatment of Acute Stroke
The acute treatment of ischemic stroke is generally supportive and medical. The role of urgent surgical or endovascular treatment of acute ischemic stroke related to carotid artery occlusive disease is controversial, and its indications are uncertain. Although urgent thrombolytic therapy given within 3 hours after an ischemic stroke is an attractive option, its widespread application is limited from a practical point of view. In one study of patients with ischemic stroke, only 23.5% arrived at the emergency department within 3 hours of symptom onset, and 4.3% received thrombolysis.16,92 Therefore, stroke prevention remains the principal approach to the battle against cerebrovascular disease and its role in causing ischemic stroke.
Thrombolysis for Acute Ischemic Stroke
Any patient presenting with an acute ischemic stroke regardless of etiology should be considered for thrombolysis, assuming there is no evidence of intracranial hemorrhage (ICH) on brain imaging. Detailed discussion regarding thrombolysis for acute ischemic stroke is presented in Chapter 36.
Pathology, Pathogenesis, and Pathophysiology of Stroke Related to Extracranial Cerebrovascular Disease
Atherosclerotic Carotid Plaque
Development of Atherosclerosis
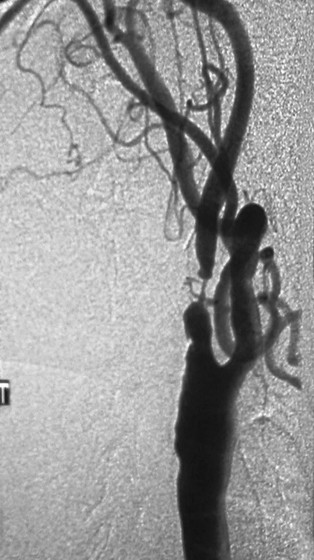
Carotid atherosclerotic plaque is similar to that found at other arterial locations (see Chapter 5).82 The carotid bulb is the major site of involvement (Fig. 97-7). Hemodynamic factors are thought to be involved in the predisposition of this particular location to the development of atherosclerotic plaque. Specifically segments with low wall shear stress and resulting flow stagnation, such as occurs in the carotid bulb, appear to be at increased risk. (See Chapters 5 and 10.)
Relationship Between Carotid Artery Atherosclerosis and Ischemic Stroke
Most acute coronary syndromes are caused by thrombus formation in moderately stenotic coronary arteries at the site of a ruptured or eroded fibrous cap.93,94 Atherosclerotic plaque in the carotid artery causes a substantial proportion of ischemic strokes, but the mechanism is less well understood than that of acute coronary thrombosis.93 Carotid artery plaque can cause TIA or stroke by two mechanisms: embolization and hypoperfusion. Owing to the abundant collateral circulation in the brain, global cerebral hypoperfusion is rare, occurring only in patients with severe multivessel occlusive disease in both the carotid and vertebral artery territories. Atheroembolization of debris originating from carotid artery plaque and traveling to the brain is believed to be the predominant cause of both TIA and ischemic stroke related to carotid artery disease (Fig. 97-8). Evidence for the role of embolization comes from the early reports of Hollenhorst,95 who found embolic debris in the retinal vessels of patients with transient monocular blindness. The severity of carotid artery stenosis is strongly associated with stroke risk in symptomatic patients.10,93,96 Currently, it is the most important predictor of benefit of carotid artery intervention.97 However, other factors predictive of stroke clearly exist, including an ulcerated appearance on carotid arteriography or duplex ultrasonography, which is also a strong independent risk factor for acute stroke93,98,99 (Fig. 97-9).
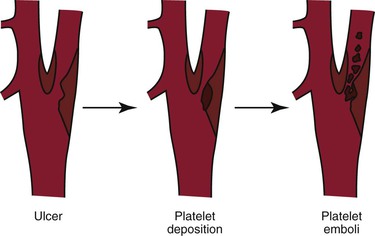
Figure 97-8 After fibrous cap rupture and plaque ulceration, the irregular, thrombogenic surface serves as a nidus for the deposition of platelet aggregates and other thrombotic debris, which can become dislodged and embolize to the brain, causing a transient ischemic attack or stroke.
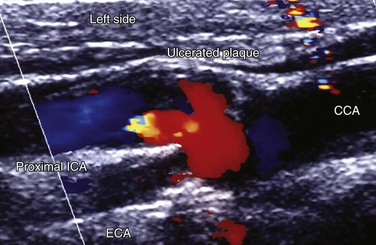
Figure 97-9 Color-flow duplex ultrasonogram of deeply ulcerated carotid plaque in a patient with multiple episodes of transient monocular blindness. CCA, Common carotid artery; ECA, external carotid artery; ICA, internal carotid artery.
Carotid artery plaque and stenosis are easily identified on noninvasive duplex ultrasound examinations. However, the severity of carotid artery stenosis is only one factor involved in identifying patients at increased risk of future ischemic stroke; it is clear that, in fact, most asymptomatic patients with moderate degrees of carotid artery stenosis are at relatively low risk of future ischemic stroke. On the other hand, only 15% of ischemic strokes are preceded by a warning TIA. Therefore waiting for stenosis to become symptomatic fails to prevent most strokes caused by carotid artery disease.100 Hence, there is a critical need to improve the selection of asymptomatic patients for carotid intervention to improve the potential effectiveness of treatment in stroke prevention.101 With this goal in mind, researchers have put a great deal of focus on identifying other characteristics of both the patient and the carotid plaque itself that would be distinguishable on imaging studies and allow the clinician to identify patients at increased risk of ischemic stroke who would most benefit from vascular intervention.
The term “vulnerable plaque” is often used to denote an unstable plaque, or a plaques that is prone to complications, including embolization and subsequent stroke. Vulnerable plaques are described histologically as having a thin fibrous cap overlying a large necrotic lipid core, and they often contain intraplaque hemorrhage and/or calcification and neovascularization93,102 (Fig. 97-10). The pathophysiologic mechanisms that lead to plaque vulnerability or instability include inflammation, degradation of extracellular matrix components, particular by matrix metalloproteases, and neovascularization.102 These cellular processes may be modified by accompanying diseases, when present, including chronic kidney disease and diabetes mellitus, which often contribute to calcification of the plaque.
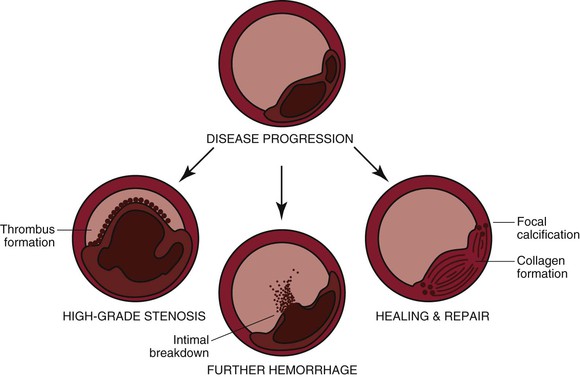
Figure 97-10 Diagram illustrating the possible events after an initial intraplaque hemorrhage. (Redrawn from Bergan JJ, et al, editors: Cerebrovascular insufficiency, New York, 1983, Grune & Stratton, p 51.)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree