Celiac Occlusion with Pancreaticoduodenal Aneurysm
AUDRA A. DUNCAN
Presentation
A 68-year-old woman with small bowel obstruction is incidentally found to have a 2.4-cm pancreaticoduodenal artery (PDA) aneurysm on a computed tomography (CT) scan performed for obstruction. Also identified on CT was an asymptomatic celiac artery occlusion due to median arcuate compression. She subsequently underwent abdominal exploration, lysis of adhesions, and bowel resection for the obstruction and remained asymptomatic regarding the PDA aneurysm.
Differential Diagnosis
PDA aneurysms and gastroduodenal aneurysms account for 1.5% to 2% of all splanchnic aneurysms and are frequently associated with pancreatic or biliary tract disease. Diagnosis must include a differentiation between true and false aneurysm because they have different etiologies and varying prognoses. For example, false aneurysm may occur in the setting of pancreatic necrosis, pseudocyst, septic emboli, or iatrogenic trauma from biliary or pancreatic interventions. Therefore, false aneurysms may require management of the primary problem first before or concomitant with aneurysm treatment. The mean age of PDA aneurysms is 50 years old with men:women ratio of 4:1, possibly because of the higher incidence of alcoholic pancreatitis in men. True PDA aneurysms, as in this patient, are less common and occur equally in men and women. It is hypothesized that these aneurysms occur in response to increased flow through pancreatic arcades in the setting of celiac stenosis or occlusion.
Workup
By history, patients with PDA aneurysms are typically asymptomatic or have vague epigastric or abdominal pain radiating to the back. If rupture occurs, as occurs in up to 75% of all PDA aneurysms, the pain can be sudden and severe. Because of the frequency of concomitant pancreatic or biliary tract disease, it is often difficult to differentiate the pain from the aneurysm compared to the pain from the underlying cause. Laboratory values of liver function studies, bilirubin, and pancreas enzymes may help differentiate underlying etiologies.
Diagnosis and Treatment
Although ultrasound may be an appropriate initial study in symptomatic patients, CT scan is often used to identify the anatomy of the biliary tract and visceral arterial anatomy. Many times, asymptomatic PDA aneurysms are identified incidentally, especially true aneurysms. CT angiography (CTA) can help delineate the presence of a celiac artery occlusion or stenosis and its cause (i.e., atherosclerotic vs. median arcuate compression) as well as identifying coexisting pancreatic or gastroduodenal disease (Fig. 1).
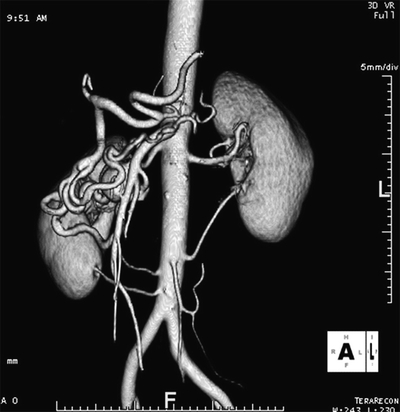
FIGURE 1 CTA with 3D reconstruction demonstrates an occluded celiac artery origin and 2.4-cm pancreaticoduodenal artery aneurysm.
Digital subtraction angiography may be used as the first imaging modality in ruptured aneurysms in order to both diagnose and treat the aneurysm at the same time. Angiography may be superior to CT at identifying efferent and afferent arteries (Fig. 2). Inspiration and expiration views of the celiac artery origin with a CTA or angiogram may reinforce the diagnosis of median arcuate compression.

FIGURE 2 Digital subtraction angiography identifies large PDA aneurysm.
Surgical Approach
Regardless of size, PDA aneurysms should be treated due to the poor correlation between size and rupture risk. A ruptured PDA aneurysm can be treated solely with embolization or surgical ligation to facilitate hemodynamic stability. Open repair has been reported to include partial pancreatectomy or pancreaticoduodenectomy when necessary.
For PDA aneurysm in the setting of celiac stenosis or occlusion, treatment of celiac lesion should precede aneurysm treatment based on the theory that increased blood flow through collaterals is the primary cause (Fig. 3). In addition, the revascularization with bypass or patch angioplasty of the celiac artery provides a pathway to place the endovascular sheath and catheters to treat the aneurysm. Once the celiac artery is reperfused, the PDA aneurysm can typically be coil embolized percutaneously (Fig. 4). Percutaneous and ultrasound-guided thrombin injection of PDA aneurysms may play a role in patients with acute pancreatitis.

FIGURE 3 Intraoperative photograph of aorta to common hepatic artery bypass with 7-mm prosthetic graft.



