Catheter-directed interventions (CDI) are increasingly used for the treatment of acute pulmonary embolism (PE), despite the scarcity of comparative prospective data. Although systemic thrombolysis improves the PE hemodynamic profile, this comes at the cost of a high major bleeding risk assumed to be negligible if CDIs are used. Mostafa et al are to be commended for this much needed review of the studies that summarize the technologies available for CDIs and the complications associated with this technique. The purpose of this letter is to call attention to the safety profile of CDIs.
The conclusion of Mostafa et al that the pooled major bleeding complication rate of ultrasound assisted thrombolysis (USAT) is “below 1%” is a significant underestimation of the published data, given the variable definition of major bleeding as reported in each study. To be consistent with the reporting of major bleeding, a Prospective, Single-arm, Multi-center Trial of EkoSonic Endovascular System and Activase for Treatment of Acute Pulmonary Embolism (SEATTLE II) study reported a 15/150 (10.0%) and not 1/150 (0.7%) major bleeding rate. Apart from the 1 patient requiring vasopressor support, all except 1 event involved at least 2 units of blood transfusion. For consistency again, since in the presented meta-analysis only USAT cases have been included, the Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis (PERFECT) study has 36 and not 100 such cases, changing its relative weight (0/36 instead of 0/100) in the pooled analysis.
Interestingly, for the study period analyzed (2008 to 2015), 2 more USAT studies are available, reporting bleeding rates of 9.4% and 3.1%, and have not been included in the analysis. Their inclusion would increase the pooled major bleeding rate.
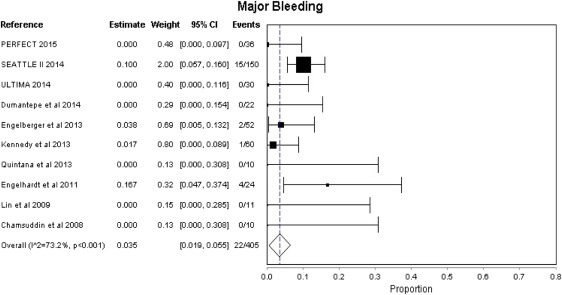
Defining major bleeding per the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Arteries (GUSTO) criteria or per the Bleeding Academic Research Consortium (BARC) classification for cardiovascular clinical trials, we constructed a forest plot using a fixed effects analysis for the same studies reported by Mostafa et al ( Figure 1 ). Both the GUSTO criteria (moderate and severe) and the BARC classification (types 3 to 5) capture all the major bleeding events in these studies. The pooled major bleeding rate is 3.5% and it better reflects the safety profile of this intervention. Any pooled analysis of this intervention’s safety profile remains both statistically and clinically heterogeneous because of differences in patient selection and study design making it difficult to capture the accurate complication rate of CDIs. This pooled major bleeding rate is similar to that obtained from the US Nationwide Inpatient Sample analysis (4.9%) and our recently published experience (6.2%). We and others have not seen any difference in outcomes and complication rates between ultrasound assisted and standard catheter thrombolysis.