Extracranial carotid fibrodysplasia represents a heterogeneous nonatherosclerotic, noninflammatory vascular disease. Principal forms of carotid arterial fibrodysplasia include medial fibroplasias and intimal fibroplasia. These two entities represent distinctly different pathologic processes. Combinations of these occlusive lesions exist, as do other less easily categorized dysplastic derangements of the vessel wall.
Most patients with carotid artery fibrodysplasia are likely to be asymptomatic, although the number of asymptomatic cases described in the literature is small because most reports are surgical experiences encompassing more advanced disease. Clinical complications of carotid fibrodysplasia when they do occur are related to the encroachment on the lumen, causing flow reductions, occasional collection of thrombi within the cul-de-sacs that embolize, dissections, and on rare occasions rupture with arteriovenous formation.
The most catastrophic complication of carotid fibrodysplasia is a stroke from embolization or acute occlusion of the dysplastic vessel with subsequent cerebral infarction. Unfortunately, the actual risk of neurologic complications is unpredictable. For instance, stroke has been described in 6% to 28% of patients with this disease, and transient ischemic attacks have been reported in 7% to 67% of these patients. Pancerebral ischemic episodes form multiple-vessel disease manifest by dizziness, and nonfocal events have been described in 2% to 50% of patients with carotid fibrodysplasia. The reported range of these events is so great as to prevent any firm conclusion as to the risk in an individual patient.
Medial fibroplasia of the extracranial internal carotid artery was initially reported in 1964. A decade later this entity was reported to affect 0.42% of 3600 patients undergoing cerebral arteriographic examinations at the University of Michigan. On the basis of arteriographic examinations, others have reported similar incidences; however, most of these studies were performed for suspected cerebrovascular disease. Thus, the true incidence of carotid fibrodysplasia in the general population is undoubtedly less.
The disease has been diagnosed most often during the fourth and fifth decades of life, although in some series the mean age at the time of recognition has been in the sixth decade. Although cumulative data on all types of carotid dysplasia reveal that 85% occur in women, classic medial fibrodysplasia with its string-of-beads appearance has rarely been encountered in men. Progression of medial fibroplasia in the carotid artery approaches 30%, but the exact rate of progression and factors contributing to it have yet to be defined. It is believed to be more progressive in women during their active reproductive years than after menopause.
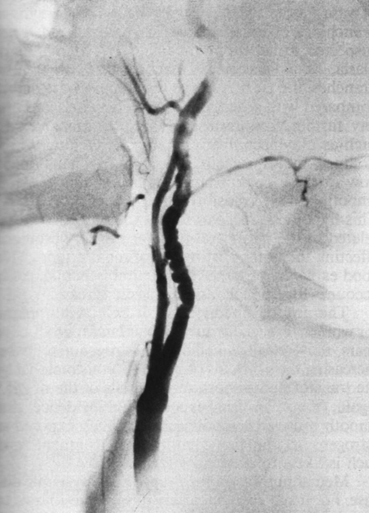
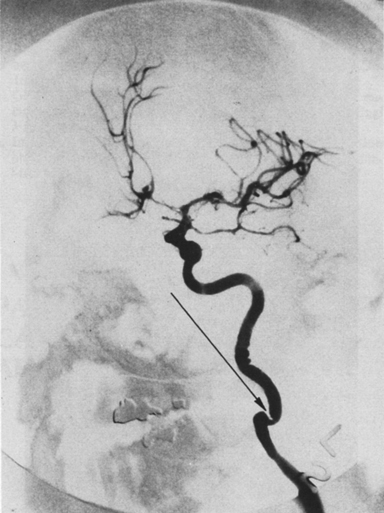
Medial fibroplasia usually involves a 2- to 6-cm segment of the internal carotid artery adjacent to the second and third cervical vertebrae (Figure 1). Bilateral medial fibrodysplastic disease occurs in approximately 65% of patients. Multiple stenoses in series with intervening mural dilations are characteristic of this disease entity. These stenoses often appear as serial narrowings on external examination of the artery. Within the interior of the vessel, a stenosis appears as an irregular luminal lining composed of linear ridges of hyperplastic-like tissue. The area of the carotid bulb has not been observed to be involved with typical medial fibroplasia. Carotid arteries that exhibit medial fibrodysplasia are often elongated, causing obvious kinking and critical narrowings in approximately 5% of patients (Figure 2). Typical medial fibroplastic disease of the intracranial arteries has been observed but is very rare.
Although the stenotic ridges of medial fibroplasias can cause stagnation of blood flow, thrombus formation in the intervening aneurysmal cul-de-sacs is a more important event. Similarly, dissections are an unusual accompaniment of medial fibroplasia. The precise incidence of the latter complication is unknown but certainly occurs in less than 10% of patients. On the other hand, dissections can obscure the underlying fibrodysplastic process, and many patients who experienced this complication might have been classified erroneously as having spontaneous dissections.
Medial fibroplastic stenoses are characterized by replacement of the media by disorganized secretory cells, considered to be modified smooth muscle cells, which appear to be myofibroblasts (Figure 3). These cells are surrounded by excess fibrous connective tissue, including considerable amounts of collagen and amorphous ground substance. Between these stenoses are aneurysmal dilations that result from a scarcity of vascular smooth muscle and medial thinning in areas of advanced disease. In most instances of medial fibroplasia, the intima and internal elastic lamina are relatively unaffected, although continuity of the external elastic lamina is often lost. Secondary intimal fibroplasia can occur in areas of advanced disease and is considered a potential adaptive response to altered flow patterns and abnormal blood-surface interactions.
Only gold members can continue reading.
Log In or
Register to continue
Related
![]()




