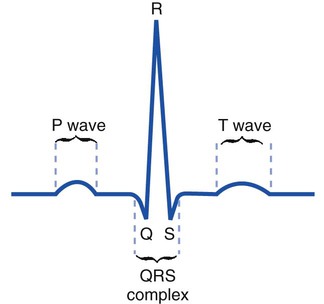
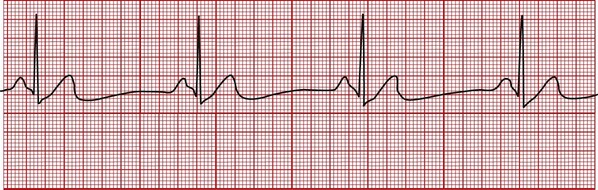
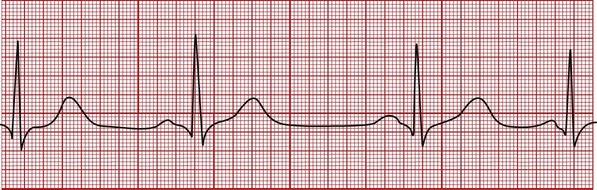
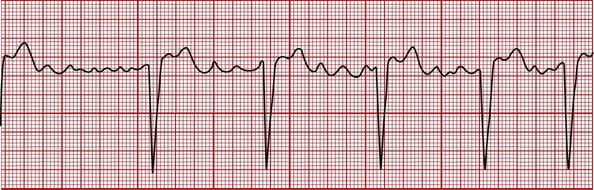
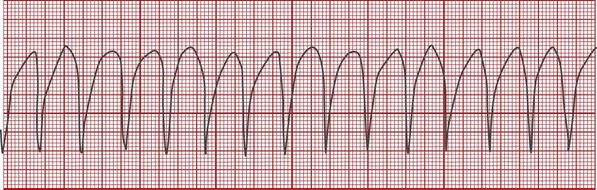
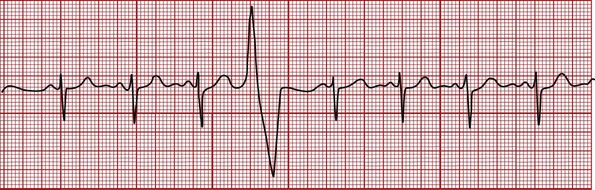
After reading this chapter, you will be able to: • Describe the ECG pattern of a normal cardiac cycle, and include the following: • Describe the characteristics of the following arrhythmias: • Premature ventricular contractions • Asystole (cardiac standstill) • Describe the noninvasive hemodynamic monitoring assessments, and include the following: • The definition of hemodynamics • The evaluation of the patient’s heart rate, cardiac output, blood pressure, and perfusion state • Describe the basic pathophysiologic mechanisms for the following hemodynamic changes that frequently develop during the acute stages of respiratory disease: • Increased heart rate (pulse), cardiac output, and blood pressure • Describe the invasive hemodynamic monitoring assessments, and include the following: • Pulmonary artery catheter measurements • Arterial catheter measurements • Central venous pressure catheter measurements • Describe how the hypoxemia, acidemia, or pulmonary vascular obstruction associated with respiratory disease alters the hemodynamic status. • Define key terms and complete self-assessment questions at the end of the chapter and on Evolve. Because the transport of oxygen to the tissue cells and the delivery of carbon dioxide to the lungs are functions of the cardiovascular system, a basic knowledge and understanding of (1) normal electrocardiogram (ECG) patterns, (2) common heart arrhythmias, (3) noninvasive hemodynamic monitoring assessments, (4) invasive hemodynamic monitoring assessments, and (5) determinants of cardiac output are essential components of patient assessment.* Because the respiratory care practitioner frequently works with critically ill patients who are on cardiac monitors, a basic understanding of normal and common abnormal ECG patterns is important. An ECG monitors, both visually and on recording paper, the electrical activity of the heart. Figure 6-1 illustrates the ECG pattern of a normal cardiac cycle. The P wave reflects depolarization of the atria. The QRS complex represents the depolarization of the ventricles, and the T wave represents ventricular repolarization. In sinus bradycardia the heart rate is less than 60 bpm. Bradycardia means “slow heart.” Sinus bradycardia has a normal P-QRS-T pattern, and the rhythm is regular (Figure 6-2). Athletes often normally demonstrate this finding because of increased cardiac stroke volume and other poorly understood mechanisms. Common pathologic causes of sinus bradycardia include a weakened or damaged sinoatrial (SA) node, severe or chronic hypoxemia, increased intracranial pressure, obstructive sleep apnea, and certain drugs (most notably the beta-blockers). Sinus bradycardia may lead to decreased cardiac output and blood pressure. In severe cases, sinus bradycardia may lead to a decreased vascular perfusion state and tissue hypoxia. The patient may demonstrate a weak or absent pulse, poor capillary refill, cold and clammy skin, and a depressed sensorium. In sinus tachycardia the heart rate is greater than 100 bpm. Tachycardia means “fast heart.” Sinus tachycardia has a normal P-QRS-T pattern, and the rhythm is regular (Figure 6-3). Sinus tachycardia is the normal physiologic response to stress and exercise. Common causes of sinus tachycardia include hypoxemia, severe anemia, hyperthermia, massive hemorrhage, pain, fear, anxiety, hyperthyroidism, and sympathomimetic or parasympatholytic drug administration. In sinus arrhythmia the heart rate varies by more than 10% from beat to beat. The P-QRS-T pattern is normal (Figure 6-4), but the interval between groups of complexes (i.e., the R-R interval) varies. Sinus arrhythmia is a normal rhythm in children and young adults. The patient’s pulse will often increase during inspiration and decrease during expiration. No treatment is required unless significant alteration occurs in the patient’s arterial blood pressure. In atrial flutter the normal P wave is absent and replaced by two or more regular sawtooth waves. The QRS complex is normal and the ventricular rate may be regular or irregular, depending on the relationship of the atrial to the ventricular beats. Figure 6-5 shows an atrial flutter with a regular rhythm with a 4 : 1 conduction ratio (i.e., four atrial beats for every ventricular beat). The atrial rate is usually constant, between 250 and 350 bpm, whereas the ventricular rate is in the normal range. Causes of atrial flutter include hypoxemia, a damaged SA node, and congestive heart failure. In atrial fibrillation the atrial contractions are disorganized and ineffective, and the normal P wave is absent (Figure 6-6). The atrial rate ranges from 350 to 700 bpm. The QRS complex is normal, and the ventricular rate ranges from 100 to 200 bpm. Causes of atrial fibrillation include hypoxemia and a damaged SA node. Atrial fibrillation may reduce the cardiac output by 20% because of a loss of atrial filling (the so-called “atrial kick”). The premature ventricular contraction (PVC) is not preceded by a P wave. The QRS complex is wide, bizarre, and unlike the normal QRS complex (Figure 6-7). The regular heart rate is altered by the PVC. The heart rhythm may be quite irregular when there are many PVCs. PVCs can occur at any rate. They often occur in pairs, after every normal heartbeat (bigeminal PVCs), and after every two normal heartbeats (trigeminal PVCs). Common causes of PVCs include intrinsic myocardial disease, hypoxemia, acidemia, hypokalemia, and congestive heart failure. PVCs also may be a sign of theophylline or alpha- or beta-agonist toxicity. In ventricular tachycardia the P wave is generally indiscernible, and the QRS complex is wide and bizarre in appearance (Figure 6-8). The T wave may not be separated from the QRS complex. The ventricular rate ranges from 150 to 250 bpm, and the rate is regular or slightly irregular. The patient’s blood pressure is often decreased during ventricular tachycardia.
Cardiovascular System Assessments
The Electrocardiogram
Common Heart Arrhythmias†
Sinus Bradycardia
Sinus Tachycardia
Sinus Arrhythmia
Atrial Flutter
Atrial Fibrillation
Premature Ventricular Contractions
Ventricular Tachycardia
Cardiovascular System Assessments