Cardiac Resynchronization Therapy
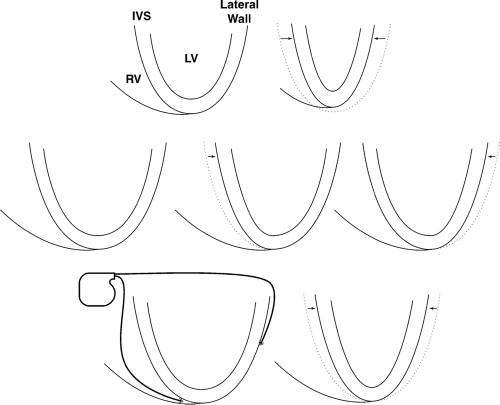
As mentioned in Chapter 1, one relatively new approach in cardiac pacing is biventricular pacing or cardiac resynchronization. This is pacing of patients with congestive heart failure to maintain synchrony between the interventricular septum of the left ventricle and the lateral wall of the left ventricle, thus improving cardiac output, and improving the patient’s symptoms and possibly patient longevity (Fig. 7-1).
The terminology can be somewhat misleading; although it is often referred to as biventricular pacing, the goal is to coordinate the contractility of the left ventricular septum and the lateral wall. This may also improve synchronization in the left and right ventricles, but the benefit appears to be synchronization of the walls of the left ventricle.
Indications
Several studies have proved the value of biventricular pacing. Basically the current indications are that the patient has a left ventricular ejection fraction of equal to or less than 35%. The source of the cardiomyopathy can be ischemic or nonischemic. The QRS duration should be greater than or equal to 120 msec. The patient should be in the American Heart Association’s Class III or IV congestive heart failure ranking and should be on optimal pharmacologic therapy for congestive heart failure.
There will be fine-tuning of the indications. Many of the studies were done with QRS complex durations much longer than 120 msec, usually with left bundle branch block (LBBB). The problem that is being treated is the dyssynchrony. There are efforts to try to identify patients who would benefit from this therapy by documenting the dyssynchrony on an echocardiogram, or by using other noninvasive approaches such as magnetic resonance imaging (although this is not commonly used and is more expensive). Cardiac resynchronization may be a benefit in some patients who have a rather narrow QRS, but still have dyssynchrony. Also it may help clarify patients with
right bundle branch block (RBBB) (the majority of patients treated with this modality have had LBBB, although there is experience with RBBB and RBBB does not rule out potential benefit). In the future, Class II patients may warrant therapy, but this is not an indication at the time this textbook is being written. Cardiac resynchronization, at this point, should be considered as part of routine therapy for patients who meet the appropriate criteria.
right bundle branch block (RBBB) (the majority of patients treated with this modality have had LBBB, although there is experience with RBBB and RBBB does not rule out potential benefit). In the future, Class II patients may warrant therapy, but this is not an indication at the time this textbook is being written. Cardiac resynchronization, at this point, should be considered as part of routine therapy for patients who meet the appropriate criteria.
Implantation
Patients undergoing cardiac resynchronization therapy (CRT) have a right atrial lead and a right ventricular lead placed using the traditional methods.
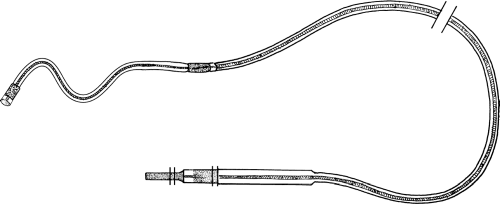
In the case of atrial fibrillation, the atrial lead is not implanted. The new, and more complex, portion of the implantation is to place a lead through the coronary sinus and down a vein on the posterolateral side of the heart. This can be a technically challenging portion of pacemaker implantation, as discussed in Chapter 10. Figure 7-2 demonstrates an example of one type of posterolateral lead. It is an “inactive” lead with no tines or the ability to be secured with screw-in leads. The curve at the end is built into the lead itself (it is not there for aesthetic purposes). There are different types of curves available, but the general principle is that the curve is designed to cause pressure of the pacemaker tip against the myocardium within the narrow vein. The lateral threshold may be slightly higher than a typical threshold, but the difference is fairly minimal. The sensing is done through the right ventricular lead (the posterolateral lead paces but does not generally sense).
In the case of atrial fibrillation, the atrial lead is not implanted. The new, and more complex, portion of the implantation is to place a lead through the coronary sinus and down a vein on the posterolateral side of the heart. This can be a technically challenging portion of pacemaker implantation, as discussed in Chapter 10. Figure 7-2 demonstrates an example of one type of posterolateral lead. It is an “inactive” lead with no tines or the ability to be secured with screw-in leads. The curve at the end is built into the lead itself (it is not there for aesthetic purposes). There are different types of curves available, but the general principle is that the curve is designed to cause pressure of the pacemaker tip against the myocardium within the narrow vein. The lateral threshold may be slightly higher than a typical threshold, but the difference is fairly minimal. The sensing is done through the right ventricular lead (the posterolateral lead paces but does not generally sense).
Programming and Follow-Up
Twenty to thirty percent of patients do not respond to CRT. There are several potential problems. Not every patient with wide QRS complex has dyssynchrony (and not every narrow QRS complex is synchronous). The lead placement is critical. If the leads are very close to each other, the dyssynchronous walls may not be paced appropriately to allow synchrony.
There can be areas of scar that impair capture or propagation of an appropriate wavefront. This is a situation in which it is important to have
consistent ventricular capture (unlike perhaps a patient with an ICD and no conduction abnormalities in whom you would want to avoid ventricular pacing). The whole point of this therapy is to synchronously pace the RV apex and thus the interventricular septum along with the posterolateral wall. If a patient develops rapid atrial fibrillation with a rapid native ventricular response, then the benefit is lost. If the patient develops short AV conduction and is functioning with intrinsic QRS complex, the benefit is lost.
consistent ventricular capture (unlike perhaps a patient with an ICD and no conduction abnormalities in whom you would want to avoid ventricular pacing). The whole point of this therapy is to synchronously pace the RV apex and thus the interventricular septum along with the posterolateral wall. If a patient develops rapid atrial fibrillation with a rapid native ventricular response, then the benefit is lost. If the patient develops short AV conduction and is functioning with intrinsic QRS complex, the benefit is lost.
The most common causes for loss of CRT effect are atrial tachyarrhythmias and loss of capture of the left ventricular lead. Occasionally, the lateral lead will cause diaphragmatic stimulation and have to be turned off. The LV lead is more prone to dislodgement than most pacemaker leads because of the lack of fixation. Occasionally a high pacing threshold can occur. Frequent ventricular ectopy can also complicate the situation.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree