Several biologic and clinical factors contribute to the increased 30-day mortality and re-infarction rate in women with ST-segment elevation myocardial infarction (STEMI). Sex differences in cardiac hemodynamic parameters such as pulmonary capillary wedge pressure (PCWP) have not been examined and might play an important role. The objectives of the present study were to examine whether female sex is an independent determinant of PCWP during acute STEMI and whether an elevated PCWP contributes to all-cause 30-day mortality and re-infarction in women. The clinical, angiographic, and hemodynamic features of 470 consecutive patients with STEMI (n = 135 women) undergoing emergency coronary angiography with right-side heart catheterization were evaluated with respect to sex. Women had an elevated PCWP (20 ± 8 vs 16 ± 7 mm Hg, p <0.001) and reduced mixed venous oxygen saturation (67 ± 11% vs 71 ± 9%, p = 0.004). On multivariate analysis, female sex (β = 4.04, 95% confidence interval [CI] 2.04 to 6.04, p <0.001), hypertension (β = 2.07, 95% CI 0.31 to 3.83, p = 0.021), and creatine kinase-estimated infarct size (β = 0.001, 95% CI 0.001 to 0.002, p ≤0.001) were independent predictors of an elevated PCWP. Female sex exerted a minor independent effect on 30-day mortality and re-infarction (odds ratio 2.36, 95% CI 1.25 to 4.46, p = 0.008). However, once PCWP was entered into the mediation model, sex was no longer significant, suggesting that the effect of sex on the post-STEMI outcomes is potentially mediated through PCWP (odds ratio 1.07, 95% CI 1.02 to 1.12, p = 0.011). In conclusion, during acute STEMI, women have greater left ventricular filling pressures compared with men, independent of age, hypertension, and infarct size. The biologic explanation for this difference requires additional investigation, although it does not appear to contribute to the increased 30-day mortality and re-infarction rate observed in women.
Since its introduction by Swan and Ganz and their colleagues in 1970, the pulmonary arterial catheter has enabled direct measurement of right heart pressures and cardiac output. Although its routine use for monitoring hemodynamic status during acute myocardial infarction (AMI) has declined, it remains a significant adjunct to clinical assessment and acute management. Of particular use is the assessment of the pulmonary capillary wedge pressure (PCWP) as a marker of the left ventricular filling pressure. Accordingly, it is a marker of pulmonary congestion, with a PCWP of ≥18 mm Hg typically associated with clinical evidence of pulmonary congestion in AMI. Furthermore, PCWP is a hemodynamic marker of poor prognosis, a strong independent predictor of short and long-term mortality after AMI and varies directly with the AMI size. Mixed venous oxygen saturation is another hemodynamic measure that can be obtained by pulmonary artery catheterization, is a direct correlate of cardiac output, and might also have prognostic potential, although weaker than that of PCWP. Despite advances in the contemporary management of ST-segment elevation myocardial infarction (STEMI), the age-adjusted 30-day mortality/re-infarction rates have remained greater for women than for men. The reason for this disparity is unclear but might include sex differences in cardiac hemodynamics during acute STEMI. Therefore, the primary objective of the present study was to examine the relation between sex and hemodynamic status during acute STEMI and to determine whether this influenced subsequent cardiac events. We therefore tested the hypotheses that (A) female sex is an independent predictor of an elevated PCWP measurement at primary percutaneous coronary intervention (PCI) for acute STEMI, and (B) that female sex and PCWP both influence the incidence of 30-day all-cause mortality and re-infarction.
Methods
The present observational cohort study used data from a STEMI clinical registry that were collected from two South Australian teaching hospitals (the Queen Elizabeth and Lyell McEwin hospitals). These university teaching hospitals service the northwestern suburbs of Adelaide. From October 2005 to October 2010, 912 consecutive STEMI patients (n = 234 women, 26%) presented to the two hospitals and had extensive clinical data collected, including cardiovascular risk factors, medications, and STEMI details. The registry has been independently audited with >90% agreement reported with case-note abstraction.
The patients included in the present study had (1) a diagnosis of acute STEMI, defined by the presence of ischemic chest pain and ST-segment elevation or new left bundle branch block, and (2) performance of right-side heart catheterization (RHC) during acute STEMI. The performance and timing of RHC was at the discretion of the interventional cardiologist, but all were performed immediately before or after PCI. Patients were excluded if the PCWP was not obtained during the primary PCI procedure. The institutional ethics committee approved our access to the STEMI registry data and follow-up details (30-day outcomes).
The patients were urgently transferred to the catheterization laboratory for emergency coronary angiography and, if indicated, primary PCI. All patients received a loading dose of heparin and aspirin with or without clopidogrel before or during primary PCI. The use of glycoprotein IIb/IIIa inhibitors, a thrombus aspiration device, or an intra-aortic balloon pump was at the discretion of the treating cardiologist. All patients were subsequently monitored in the coronary or intensive care unit for ≥48 hours.
The sequential right atrial pressure, right ventricular pressure, pulmonary artery pressure, and PCWP were recorded using a Swan-Ganz catheter, with continuous recording of the systolic femoral artery pressure using a femoral artery sheath. Arterial and mixed venous blood samples were taken for determination of the arterial and mixed venous oxygen saturation using a blood gas analyzer (Radiometer Copenhagen NPT 7 Series blood gas analyzer; Radiometer Copenhagen, Denmark). The heart rate was continuously monitored using 3-lead electrocardiographic recording.
Detailed clinical data, including patient demographics, cardiovascular risk factors, medical history, maintenance medications, infarct characteristics and logistics, hospital arrival hemodynamic status, post-PCI outcomes (including peak creatine kinase [CK]-estimated infarct size), and the cardiac catheterization hemodynamic measurements were abstracted from the case notes and recorded in a prospectively maintained registry. The clinical outcome measures were determined from the administrative data sets and included 30-day mortality and 30-day re-infarction. The diagnosis of recurrent infarction was determined the presence of typical chest pain, new ST-segment changes, and an increase in CK of ≥50% greater than the previous trough level in ≥2 samples, with a minimum increase of twice the upper CK reference limit.
The clinical and outcome variables were compared between the sexes. Categorical variables are presented as frequencies and were compared using the Pearson chi-square or Fisher exact test. Continuous variables are expressed as the mean ± SD or median and interquartile range (25th and 75th percentiles), with comparisons made using Student’s independent t tests or nonparametric Mann-Whitney U tests, as appropriate. The myocardial infarction outcomes (composite end point of 30-day mortality and re-infarction) were compared between the men and women using logistic regression models, with adjustment for age.
A multivariate linear regression model was fit to identify independent predictors of PCWP and adjusted for conventional covariates (hypothesis A). These included age, cardiovascular risk factors (hypertension, diabetes mellitus, previous coronary disease, history of smoking), peak CK level, acute pulmonary edema, and location of the infarction (anterior vs nonanterior). In addition, clinically relevant determinants of cardiac mortality were incorporated into the model, including sex, office hours presentation, arrival by the ambulance service, door-to-balloon time, blood urea nitrogen/creatinine ratio, hemoglobin, Thrombolysis In Myocardial Infarction (TIMI) grade 3 before and after PCI, stroke, ventricular fibrillation arrest, arrival heart rate, and arrival systolic blood pressure.
To assess the relation among sex, PCWP, and early adverse outcomes (hypothesis B), 2 logistic regression models were performed. The first assessed the total effect of sex on 30-day mortality and re-infarction and the second the direct and indirect effect of sex, after adjustment for PCWP. For all analyses, the complete and available data set was used, with no imputation for missing variables. A p value of <0.05 was considered statistically significant. All analyses were performed using Statistical Package for Social Sciences, version 18.0, for Macintosh (SPSS, Chicago, Illinois).
Results
From the 912 consecutive cases in the STEMI registry, hemodynamic data were available for 470 patients (n = 135 women, 15%). More than half of the hospital interventional cardiologists routinely performed RHC (68%) in the patients with acute STEMI they attended but only on selected patients by other cardiologists (32% RHC). Thus, the study cohort essentially represented consecutive patients treated by these interventional cardiologists. Moreover, compared with the overall cohort (n = 912), the hemodynamic subset evaluated in the present investigation was similar in regard to sex, cardiovascular risk factors, door-to-balloon time, heart rate, systolic blood pressure, and 30-day all-cause mortality and re-infarction ( Appendices 1 and 2 ). Accordingly, except for age (which was adjusted for in subsequent analyses), no evidence was found of a systematic selection bias, suggesting that the study hemodynamic cohort was representative of the total STEMI population.
The prehospital clinical characteristics of the 470 consecutive patients with STEMI are listed in Table 1 . The women were significantly older than the men, with many >75 years old ( Table 1 ). Furthermore, women were more likely to have hypertension and be treated with β blockers, and the men were more likely to be smokers and to weigh more. Although the women had prolonged pain-to-door and door-to-balloon times compared with men, they were similar in relation to other infarct characteristics, admission clinical hemodynamic status, and post-PCI outcomes, including infarct site and size ( Table 2 ).
| Variable | Total Sample (n = 470) | Men (n = 335) | Women (n = 135) | p Value |
|---|---|---|---|---|
| Age (yrs) | 63 ± 13 | 61 ± 13 | 69 ± 13 | 0.001 ∗ |
| <55 | 155 (33) | 128 (38) | 27 (20) | 0.001 ∗ |
| 56–64 | 98 (21) | 75 (22) | 23 (17) | 0.211 |
| 65–74 | 101 (22) | 73 (21) | 28 (21) | 0.901 |
| ≥75 | 116 (25) | 59 (18) | 57 (42) | 0.001 ∗ |
| Hypercholesterolemia † | 226 (53) | 159 (52) | 67 (56) | 0.518 |
| Hypertension ‡ | 217 (51) | 143 (46) | 74 (62) | 0.005 ∗ |
| Diabetes mellitus | 123 (28) | 83 (27) | 40 (32) | 0.288 |
| Family history of CAD | 82 (19) | 59 (19) | 23 (19) | 1.000 |
| Smoker | 246 (58) | 195 (64) | 51 (43) | 0.001 ∗ |
| Previous CAD § | 103 (24) | 72 (24) | 31 (26) | 0.615 |
| Weight (kg) | 83 ± 17 | 86 ± 16 | 73 ± 16 | 0.001 ∗ |
| Maintenance medications | ||||
| Aspirin | 65 (18) | 43 (16) | 22 (24) | 0.115 |
| Statin | 94 (26) | 67 (25) | 27 (29) | 0.411 |
| ACE inhibitor ‡ | 68 (19) | 49 (18) | 19 (21) | 0.642 |
| β Blocker | 28 (8) | 12 (4) | 16 (17) | 0.001 ∗ |
| Calcium channel blocker | 14 (4) | 8 (3) | 6 (7) | 0.205 |
| Insulin therapy | 14 (4) | 8 (3) | 6 (7) | 0.206 |
† Hypercholesterolemia defined by any of the following: (1) total cholesterol >200 mg/dl (5.18 mmol/L), (2) low-density lipoprotein ≥130 mg/dl (3.37 mmol/L), and (3) high-density lipoprotein <40 mg/dl (1.04 mmol/L).
‡ Hypertension defined by any 1 of the following: (1) history of hypertension diagnosed and treated with medication, diet, and/or exercise, (2) previous documentation of blood pressure >140 mm Hg systolic and/or 90 mm Hg diastolic for patients without diabetes or chronic kidney disease, or previous documentation of blood pressure >130 mm Hg systolic or 80 mm Hg diastolic on ≥2 occasions for patients with diabetes or chronic kidney disease, and (3) currently receiving pharmacologic therapy for hypertension.
| Variable | Total Sample (n = 470) | Men (n = 335) | Women (n = 135) | p Value |
|---|---|---|---|---|
| Infarct characteristics | ||||
| PTD time (min) | 111 (60–240) | 101 (55–218) | 141 (60–307) | 0.040 ∗ |
| DTB time (min) | 76 (56–104) | 73 (54–101) | 85 (67–115) | 0.004 ∗ |
| Office hours presentation † | 194 (42) | 143 (43) | 51 (38) | 0.350 |
| Anterior infarction | 170 (37) | 125 (38) | 45 (35) | 0.520 |
| Triple vessel disease | 231 (51) | 170 (52) | 61 (48) | 0.529 |
| Pre-PCI TIMI-3 flow | 71 (15) | 44 (13) | 27 (20) | 0.065 |
| BUN/creatinine ratio (μmol/L) | 93 ± 42 | 94 ± 34 | 90 ± 58 | 0.529 |
| eGFR ≤60 ml/min | 95 (20) | 51 (16) | 44 (36) | 0.001 ∗ |
| Arrival hemoglobin (g/dl) ‡ | 14.1 ± 19 (13.8–14.2) | 14.4 ± 19 (14.2–14.6) | 13.0 ± 17 (12.7–13.3) | 0.001 ∗ |
| Clinical hemodynamic status | ||||
| Arrival heart rate (beats/min) | 79 ± 22 | 79 ± 21 | 79 ± 24 | 0.696 |
| Arrival SBP (mm Hg) | 137 ± 30 | 137 ± 29 | 136 ± 30 | 0.879 |
| Acute pulmonary edema | 22 (5) | 16 (5) | 6 (4) | 1.000 |
| Stroke | 3 (1) | 1 (1) | 2 (2) | 0.178 |
| Ventricular fibrillation arrest | 28 (6) | 21 (6) | 7 (5) | 0.830 |
| Intra-aortic balloon pump use | 35 (7) | 25 (8) | 10 (7) | 1.000 |
| Post-PCI outcomes | ||||
| Post-PCI TIMI-3 flow achieved | 406 (87) | 289 (86) | 117 (87) | 1.000 |
| No re-flow phenomenon | 16 (4) | 9 (3) | 7 (6) | 0.160 |
| Bare metal stent | 336 (72) | 248 (74) | 88 (65) | 0.070 |
| Drug-eluting stent | 21 (5) | 13 (4) | 8 (6) | 0.331 |
| GPIIb/IIIa antagonist | 109 (23) | 83 (25) | 26 (19) | 0.228 |
| Export catheter | 27 (6) | 23 (7) | 4 (3) | 0.182 |
| Peak creatine kinase (IU/L) | 1,886 ± 4,787 | 2,100 ± 5,541 | 1,320 ± 1,416 | 0.127 |
| Hospital stay (days) | 4 ± 3 | 4 ± 3 | 4 ± 4 | 0.568 |
† Normal catheterization office hours (8:30 a.m. to 5:00 p.m. , Monday to Friday).
‡ Normal reference range for hemoglobin level in men, <13.0 g/dl, and women, <12.0 g/dl.
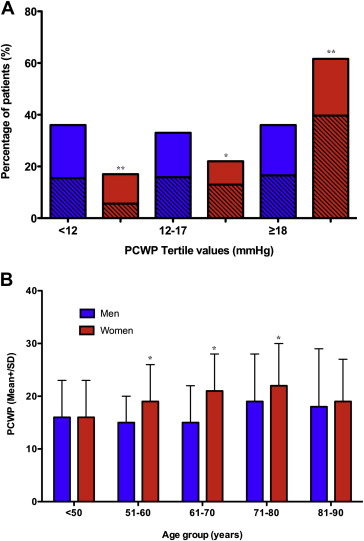
Despite similar right atrial and right ventricular pressures to men, women had greater pulmonary artery pressures and PCWP, with almost 2/3 having a PCWP of ≥18 mm Hg compared with 1/3 of the men ( Table 3 and Figure 1 ). Furthermore, as illustrated in Figure 1 , this appeared to be independent of hypertension (because 22 women [36%] with a PCWP of ≥18 mm Hg did not have a history of hypertension) and age ( Figure 1 ). Also, women with AMI had a significantly lower mixed venous oxygen saturation despite preserved arterial oxygen saturation ( Table 3 ). Thus, compared with the men, more women with acute STEMI had hemodynamic markers consistent with increased left ventricular filling pressure and/or reduced cardiac output.
| Variable | Total Sample (n = 470) | Men (n = 335) | Women (n = 135) | p Value |
|---|---|---|---|---|
| Hemodynamic measurements | ||||
| Mean RA pressure (mm Hg) | 10 ± 9 | 10 ± 11 | 10 ± 5 | 0.876 |
| Systolic RV pressure (mm Hg) | 40 ± 12 | 39 ± 12 | 41 ± 9 | 0.095 |
| Mean PA pressure (mm Hg) | 23 ± 8 | 22 ± 8 | 26 ± 8 | 0.001 ∗ |
| Mean PCWP (mm Hg) | 17 ± 7 | 16 ± 7 | 20 ± 8 | 0.001 ∗ |
| Patients with PCWP ≥18 mm Hg | 179 (38) | 111 (36) | 68 (61) | 0.001 ∗ |
| Mean FA pressure (mm Hg) | 95 ± 20 | 95 ± 19 | 95 ± 20 | 0.838 |
| MVO 2 (%) | 70 ± 10 | 71 ± 9 | 67 ± 11 | 0.004 ∗ |
| Femoral artery saturation (%) | 98 ± 3 | 98 ± 3 | 97 ± 3 | 0.364 |
| Cardiac event | ||||
| 30-Day all-cause mortality | 28 (6) | 15 (5) | 13 (10) | 0.242 |
| 30-Day re-infarction | 16 (3) | 8 (2) | 7 (5) | 0.069 |
| 30-Day all-cause mortality and re-infarction | 43 (9) | 23 (7) | 20 (15) | 0.034 ∗ |
| Cardiac cause of death | 21 (4) | 10 (53) | 11 (65) | 0.516 |