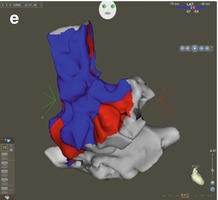
Figure 1.1
(a–e) Three dimensional reconstruction using CARTO (Biosense-Webster) of the RA showing sinus rhythm impulse propagation represented by the red wavefront as it spreads across the right atrium from the right anterior oblique view
Figure 1.2
Three dimensional reconstruction using CARTO (Biosense-Webster) of the RA showing electroanatomical activation map showing site of origination of a sinus rhythm impulse, from the right anterior oblique (left) and right lateral (right) views. Red represents earliest activation and the sinus node’s location. Yellow, green, teal, and blue represent respective later activation timing relative to the sinus node impulse. SVC superior vena cava, CS coronary sinus, RAA right atrial appendage
The AV node is located at the apex of the triangle of Koch, which is represented by the septal tricuspid valve annulus anteriorly, the coronary sinus ostium posteriorly, and the tendon of Todaro superiorly [1]. Acting as a gateway, the AV node exhibits decremental properties which help protect the ventricles from tachyarrhythmias starting from the atria. From here propagation continues inferiorly and anteriorly to the bundle of His. Once the depolarizing wavefront exits the His bundle, the signal divides into three fascicles, the left anterior, the left posterior and the right bundle branch. Finally the impulse disseminates throughout the ventricular myocardium via smaller purkinje fibers. Conduction velocity is most rapid through the above activation sequence.
Patients may present in sinus rhythm with some clues to conduction disease on the surface ECG which may include either a prolonged PR interval, left anterior fascicular block (LAFB), left posterior fascicular block (LPFB), right bundle branch block (RBBB) or left bundle branch block (LBBB). Some patients may have more than one type of block such as first-degree AV block, fascicular block (either left anterior or left posterior) and RBBB. This combination is more commonly referred to trifascicular block. The remaining conduction to the ventricle is dependent on a single fascicle. In those patients with a left bundle branch block (both the left anterior and posterior fascicles are blocked) the conduction to the ventricle is through the right bundle. Usually the remaining bundle’s conduction velocity is adequate to prevent symptoms, however, one should be more suspicious of a bradyarrhythmia as an etiology if multiple blocks are observed on the surface ECG. Of particular concern is alternating RBBB and LBBB as it is clear evidence of infra-nodal conduction disease. These patients should undergo pacemaker placement without the need for invasive electrophysiology testing as they are at high risk for complete heart block. Patients with bundle branch block particularly those with LBBB have been found to be at higher than normal risk for ventricular tachyarrhythmias and therefore it is important that such patients be thoroughly evaluated when presenting with syncope.
Each region of cardiac tissue is capable of generating an impulse (automaticity), however, the sinus node generally fires more rapidly and captures the remaining cardiac segments. A hierarchy of automaticity exists from the atria with a lower end rate limit of 40 bpm, to the AV node roughly 30–40 bpm, and the purkinje fibers 20–30 bpm. When there is impulse dysfunction in the atria the signal no longer suppresses the AV nodes automaticity and a junctional rhythm (usually narrow complex unless known bundle brach block) may be evident. If the rhythm originates from the purkinje fibers it is best described as an idioventricular rhythm, and will appear very slow with a wide QRS complex.
Sinus Node Dysfunction
Sinus node dysfunction is an umbrella term that refers to abnormalities in SN impulse formation and propagation and includes conditions such as sinus bradycardia, sinus pause/arrest, chronotropic incompetence, sinus exit block, sick sinus syndrome and tachy-brady syndrome where rapid periods of atrial fibrillation terminate often into symptomatic episodes of sinus bradycardia or sinus pauses. Sinus node dysfunction is a disease of the elderly and its initial presentation may include syncope due to inadequate impulse formation and propagation resulting in cerebral hypoperfusion and collapse [2]. Sinus node dysfunction is the most common diagnosis in patients requiring permanent pacemaker implant.
The action potentials of both the SA and AV node are dependent on sodium “funny” currents. These channels are recognized as funny because they open as the cell repolarizes rather than reaching a more positive threshold to evoke an action potential. The SA node traditionally depolarizes and repolarizes most rapidly and therefore is responsible for setting the heart rate if cardiac conduction is normal. Sympathetic (adrenaline) and parasympathetic (vagal) signals from the autonomic nervous system have strong influences on heart rate due to their primary inputs to the SA and AV node. Historically, a “normal” heart rate ranges from 60 to 100 beats per minute (bpm), however, it is not uncommon for those with high vagal tone (well conditioned athletes, or during sleep) to have rates as low as 40 bpm [3]. Electrocardiogram (ECG) tracings may reflect either a sinus bradycardia mechanism or a junctional escape rhythm (an impulse originating from the AV node.) Bradycardia in and of itself is not problematic unless it is associated with symptoms such as dizziness, fatigue, shortness of breath, chest pain or syncope [4]. On the contrary, patient’s may present with exertional symptoms despite resting heart rates in the 60s. Placing these patients on a treadmill or on a Holter monitor may reveal chronotropic incompetence, or lack of the SA node to increase the heart rate appropriately with activity [5]. It is important to make the distinction between physiologic bradycardia and symptomatic pathologic bradycardia to avoid unnecessary testing or treatments which may only cause harm and or provide little to no benefit. Furthermore, the etiology of the arrhythmia must strongly be considered. Electrolyte imbalance, ischemia, infection, hypoxia, vagal tone, hypothermia, hypothyroidism, post surgical as well as other causes may be transient and treating the underlying cause may very well resolve the cardiac conduction disturbance [6, 7]. Temporary pacemakers may be considered in specific emergent situations as deemed necessary.
Atrioventricular Block
AV block can be classified as first, second or third degree (also known as complete heart block). Although a distinct conduction fiber between the sinus node and this His-bundle does not exist, first degree AV block refers to a PR interval exceeding 0.2 s. A long PR interval in the setting of a normal QRS duration usually represents conduction delay in the AV node. If the QRS duration is prolonged, the most common site of conduction delay is still in the AV node, however the possibility of infra-Hisian conduction disease needs to be considered, especially in the presence of left bundle branch block. It is important however to recognize that a normal PR interval does not itself rule out the possibility of more advanced and severe conduction disease. In general, first degree AV block is clinically well tolerated and is not associated with an increase in overall mortality. However, in rare cases a PR exceeding 0.3 s can produce pacemaker syndrome-like symptoms where atrial activation begins as ventricular systole continues, and atrial contraction occurs across closed atrio-ventricular valves.
Second degree AV block (Fig. 1.3) is subdivided into Mobitz Type 1 and Mobitz Type 2 block.
Figure 1.3
12 lead electrocardiogram demonstrating 2:1 AV block. There are 2 p waves for every qrs complex. It is not possible to tell where the level of block is without provocative maneuvers such as having the patient ambulate, vagal maneuvers or administering medications which can inhibit or enhance AV node conduction
Electrocardiographically, Mobitz type 1 exhibits the Wenckebach phenomenon where progressive prolongation in the PR interval is seen leading up to a non-conducted P wave. Following the non-conducted beat, conduction with a normal PR interval is usually seen. The block cycle recurs repetitively with a fixed P to QRS ratio. Most commonly AV block in Mobitz 1 occurs at the level of the AV node less so in the His-Purkinje system. Mobitz Type 1 block is common in healthy individuals and in states of high vagal innervation such as during sleep. However, Mobitz Type 1 block that occurs during high sympathetic innervation such as with exercise usually denotes infra-Hisian disease possibly requiring electrophysiologic testing [8]. Contrary, Mobitz Type 2 block demonstrates a fixed PR interval with a non-conducted P wave. Maneuvers like carotid sinus massage can be useful for differentiating between Mobtiz Type 1 and Type 2 block when there is 2:1 conduction. For Mobitz Type 1 block the higher vagal input to the AV node will increase the amount of blocked p waves. However, for Mobitz Type 2 block the higher vagal input to the AV node will slow conduction enough to let the diseased infrahisian tissue time to recover allowing for a 1:1 relationship (Fig. 1.4).
 < div class='tao-gold-member'>
< div class='tao-gold-member'>




Only gold members can continue reading. Log In or Register to continue
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


