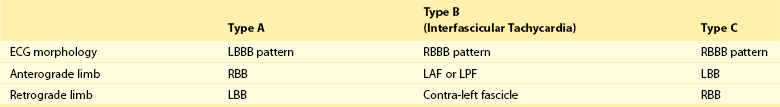
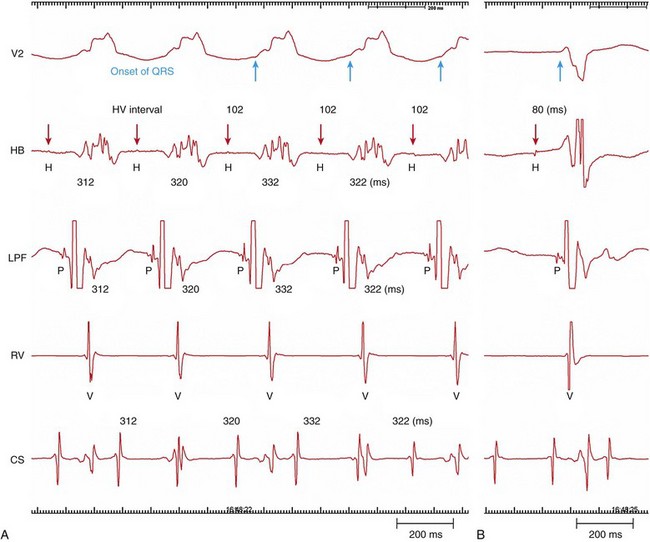
83 Bundle branch reentry (BBR) ventricular tachycardia (VT), first elucidated by Guerot et al. in 1974, is a unique, fast (200 to 300 beats/min), monomorphic tachycardia associated with hemodynamic collapse, syncope, and/or cardiac arrest and caused by a macroreentry circuit involving the right and left bundle branches, an upper common pathway, and septal ventricular muscle.1–3 BBR occurs in patients who have dilated cardiomyopathy and in those with coronary artery disease, valvular heart disease, myotonic dystrophy, or even no heart disease with associated His-Purkinje system disease.4–9 The incidence is reported to be 3.5% and 6% of ventricular tachycardias in separate series and 20% in a series of patients with nonischemic cardiomyopathy alone undergoing evaluation for ablation.10–12 Likely, BBR is underrecognized. The morphology of the tachycardia can have a typical left bundle branch block (LBBB)13 pattern (Figure 83-1, A) or right bundle branch block (RBBB) pattern (Figure 83-1, B). Some patients have both counterclockwise and clockwise BBR, causing an LBBB and RBBB morphology, respectively.14 It is possible for LBBB morphology BBR to have several morphologies presumably as the result of extensive right bundle branch (RBB) disease in patients with dilated heart.13 Multiple monomorphic morphologies can occur, as anterograde conduction via the left anterior or left posterior fascicle can be present along with retrograde activation of the RBB.15 BBR-VT with multiple morphologies has also been described in Ebstein’s anomaly.7 Figure 83-1 Twelve-Lead ECGs During Bundle Branch Reentry Tachycardias BBR can present with a similar or identical QRS complex morphology to that present in normal sinus rhythm. Although the QRS complex morphology in VT can be identical to that in sinus rhythm in all 12 electrocardiographic (ECG) leads,16 not all such VTs are necessarily BBR.17 An RBBB and left hemiblock pattern is more consistent with an interfascicular tachycardia (Figure 83-1, C, D). Attempts have been made to model the His-Purkinje system and to define the reentrant circuit(s) responsible for BBR.18 Under normal conditions, sustained reentry cannot occur, but under conditions of slowed conduction in the His-Purkinje system and ventricular muscle, the path length can be increased such that sustained anatomical reentry does occur using these structures and with an excitable gap (Figure 83-2). Figure 83-2 Successful Attempt to Stimulate Bundle Branch Reentry in a Model of Ventricular Conduction System During BBR-VT, activation proceeds anterograde via the RBB through the septum and retrograde via the LBB to activate the septal summit/His bundle and reactivate the RBB sequentially (“counterclockwise” reentry). The ECG morphology of counterclockwise BBR is a typical LBBB with an R-wave transition between leads V4 and V5. LBBB morphology BBR is the cause of 98% of episodes of BBR-VT.19 This may be due to the fact that the LBB is the preferred retrograde route of activation.20 Alternatively, activation can proceed anterograde via the LBB, through the septum, and retrograde via the RBB, creating an RBBB morphology (“clockwise” reentry).10,20 Anterograde activation via the RBB and retrograde via the left posterior fascicle (LPF) or the left anterior fascicle (LAF) alone is another possibility. Conduction delay, critical for initiation and perpetuation of BBR, may be present in connections between the bundles and even within the His bundle itself. Anisotropic conduction in the common His bundle, potentially critical for initiation and maintenance of BBR,21 may explain the greater degree of H-V delay often noted during tachycardia than in sinus rhythm. Other mechanisms potentially explaining the observed H-V prolongation during tachycardia could be due to progressive distal Purkinje system conduction delay in diseased bundles, whose slowing is more apparent at rapid rates (phase 3 block). BBR can occur in patients who have apparently normal His-Purkinje conduction during sinus rhythm but who have evidence of a functional conduction impairment at faster rates.22 Li et al.22 reported a series of 178 patients with VT, of whom 13 had BBR-VT. Of those 13, 6 had an H-V interval ≤55 ms during sinus rhythm (i.e., normal). In those BBR-VT patients with a normal H-V interval at baseline, the H-V interval was prolonged during BBR-VT (73 ± 18 vs. 47 ± 7 ms; P = .007). Functional His-Purkinje delay was present with rapid atrial pacing or premature extrastimuli in this group but not in those with prolonged H-V intervals in sinus rhythm who had BBR-VT. The explanation for BBR-VT in these patients may be the higher turnaround point in the BBR circuit in the proximal portion of the His bundle or in the N-H region of the AV node. Additionally, functional block initiating BBR may be perpetuated by persistent “linking.”23 BBR-VT is distinguished from interfascicular VT, in which the tachycardia depends on activation via the LPF and the LAF alone. His-bundle or RBBB activation is not necessary for the tachycardia to propagate. During interfascicular tachycardia, the morphology is an RBBB with right or left axis deviation. Right bundle reentry has been reported.24 BBR-VT has several modes of spontaneous initiation. Ventricular premature beats are often the trigger. Occasionally, premature atrial beats or atrial fibrillation25 can initiate BBR. Bradycardia-dependent LBBB initiation of BBR, without obvious intra-myocardial conduction delay, is possible spontaneously during sinus bradycardia.26 BBR has also been described in a patient with cycles of AV block and in association with bradycardia-dependent phase 4 bundle branch block.27 BBR-VT storm has been related to ventricular pacing that causes retrograde activation through the His-Purkinje system.28 In the electrophysiology laboratory, ventricular extrastimuli delivered with long-short coupling intervals (pacing train of 400 milliseconds with a delay of 600 or 800 milliseconds before the short-coupled premature coupling intervals are introduced) tend to cause unidirectional block or sufficient conduction delay in a bundle branch to initiate BBR. Long-short coupling intervals are specific for initiation of BBR.29 Atrial pacing and/or isoproterenol may be required.30 In one report, incremental atrial pacing during isoproterenol infusion initiated BBR with an RBBB pattern in four of six patients with inducible BBR-VT.31 Class IA or IC antiarrhythmic drugs may slow conduction sufficiently in one of the bundles to allow BBR to occur (and thus may be proarrhythmic for this condition32). Rarely are such drugs used to initiate BBR in the clinical context. Several criteria help in the diagnosis of BBR-VT: (1) The 12-lead ECG appearance during tachycardia is a typical LBBB or RBBB morphology. (2) A critical delay in His-Purkinje system conduction is needed to initiate tachycardia. (3) Although atrioventricular (AV) dissociation may be present, there is persistent 1 : 1 His-bundle/QRS activation with the H-V interval during the tachycardia equal to or longer than the H-V interval in sinus rhythm (and no H-V dissociation). (4) Tachycardia stops and cannot be reinitiated if conduction in one of the bundle branches is disrupted. In some instances, temporary disruption of conduction via one bundle may occur purposefully, or unintentionally, with a catheter bump.33 (5) His-bundle, RBB, and LBB activation sequences during tachycardia recorded by point-by-point mapping are consistent with the presence of bundle branch block (i.e., if there is an LBBB morphology tachycardia, activation is in the order of His bundle, RBB, and then LBB), and the activation relationship remains stable. (6) A predictable change in the V-V interval occurs after the H-H interval if rate fluctuations exist. H-H interval timing changes before timing of the V-V interval. The H-V timing remains constant. If no perturbation in the H-H interval is present, atrial pacing can advance to atrial then ventricular activation with a similar QRS complex morphology and H-V interval. (7) Entrainment with constant fusion (manifest entrainment) is present during pacing from the right ventricular apex.34 However, pacing from the right ventricular apex during BBR-VT results in a postpacing interval similar to the length of the tachycardia cycle (9 ± 11 ms), and never longer than 30 ms.35 These findings serve as evidence of macro-reentry within the His-Purkinje system.36 During resetting, when pacing from the right ventricular apex, an increasing reset response is noted (i.e., return cycle length is progressively longer), whereas recordings with respect to the H-V interval show a flat response consistent with a reentry circuit that has an excitable gap and involves the bundle branches but not the ventricular muscle.37 (8) Entrainment with concealed fusion is present during atrial pacing if AV nodal conduction allows faster pacing than is seen with tachycardia. Tchou et al. described three categories of BBR-VT (Table 83-1; Figure 83-3).38 Type A and type C are the classic counter-clockwise and clockwise BBR-VTs circuits. Type B is reentry within the LBB fascicles (interfascicular reentry). Figure 83-3 Schematic Illustrations of Reentrant Circuits for Bundle Branch Reentry and Interfascicular Reentry In types A and C BBR-VT, the onset of ventricular depolarization is preceded by His-bundle, RBB, or LBB potentials with an appropriate sequence of His-bundle->RBB>LBB activation and relatively stable H-V, RBB-V, or LBB-V intervals. Spontaneous variations in V-V intervals are preceded by similar changes in H-H/RBB-RBB/LBB-LBB intervals (Figure 83-4).
Bundle Branch Reentry Tachycardia
Electrocardiographic Appearance
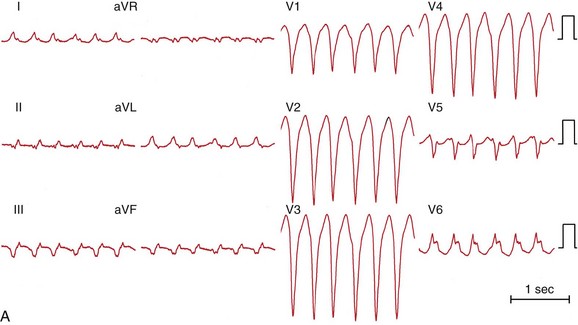
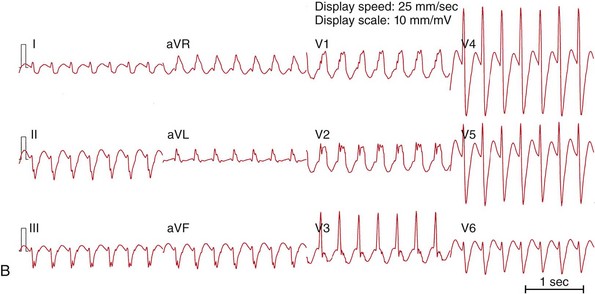
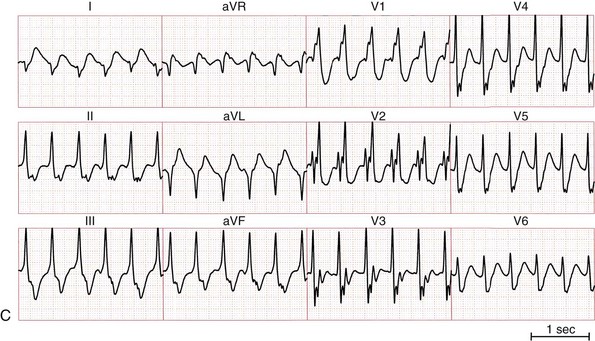
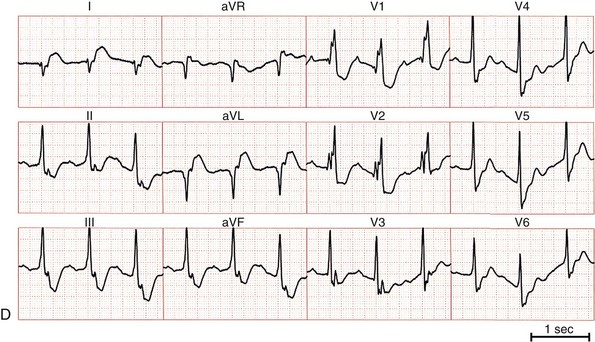
A, ECG of a bundle branch reentry with left bundle branch block morphology (type A). B, ECG of a bundle branch reentry with right bundle branch block morphology and left-axis deviation (type C). C, ECG of an interfascicular reentry with right bundle branch block morphology and right-axis deviation (type B). D, ECG during sinus rhythm of the patient with interfascicular reentry in (C), showing PR prolongation, right bundle branch block, and right-axis deviation. Note that QRS morphology in tachycardia is identical to that in sinus rhythm.
Mechanisms
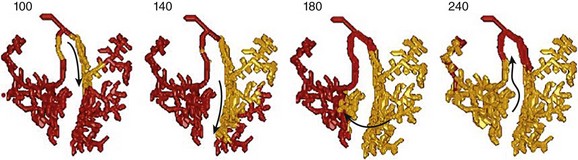
Activation sequence in the Purkinje system under simulated temporal conduction block in the right Purkinje branch. Arrows indicate the direction of wave propagation. Excitation goes from the LBB to the septum, up the RBB, toward the LBB, where it runs into the previous excitation wave. To attain sustained BBR-VT, the effective path length of the reentry circuit needs to be increased (such as slowing conduction sufficiently). (Modified from Tusscher KH, et al: Modeling of the ventricular conduction system. Prog Biophys Mol Biol 96:152-170, 2008.18)
Initiation of Tachycardia
Diagnosis of Bundle Branch Reentry
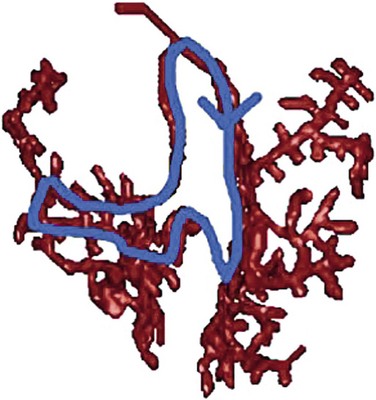
Activation Patterns
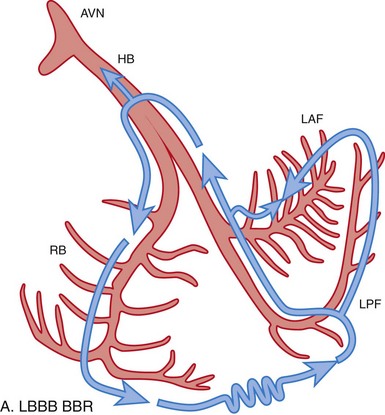
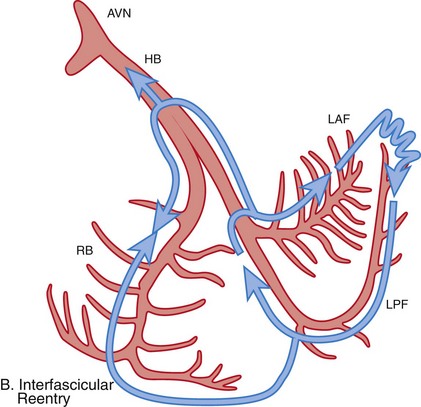
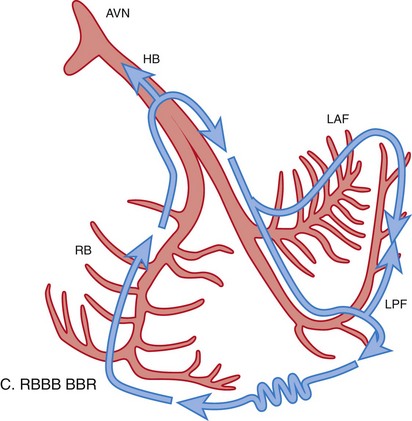
A, Typical type of BBR in which retrograde conduction occurs via the left bundle (LBB) branch and anterograde conduction over the right bundle (RBB) branch. B, Interfascicular reentry with anterograde and retrograde conduction over opposing fascicles of the LBB. C, Reversal of the circuit depicted in (A). AVN, Atrioventricular node; BBR, bundle branch reentry; HB, His bundle; LAF, left anterior fascicle; LPF, left posterior fascicle; RBB, right bundle branch. (Modified from Nogami A: Purkinje-related arrhythmias. Part I: Monomorphic ventricular tachycardias. Pacing Clin Electrophysiol 34: 624-650, 2011.46)
Bundle Branch Reentry Tachycardia