Bullous Disease
Presentation
A 49-year-old man presents to the emergency department with complaints of shortness of breath. He describes persistent and worsening symptoms of shortness of breath and wheezing over several years. He relates a longer than 20-year history of respiratory problems, including a previous pneumothorax requiring tube thoracostomy. He reports a 35-pack-per-year smoking history. On physical examination, you find that he is thin, and although not in respiratory distress, his respiratory rate is elevated (34 breaths/min), with an oxygen saturation of 90%. On auscultation, both lung fields have diminished breath sounds and bilateral wheezing. There is egophony and hyperresonance bilaterally. The emergency department physician obtains chest x-rays and requests an immediate thoracic surgery consult.
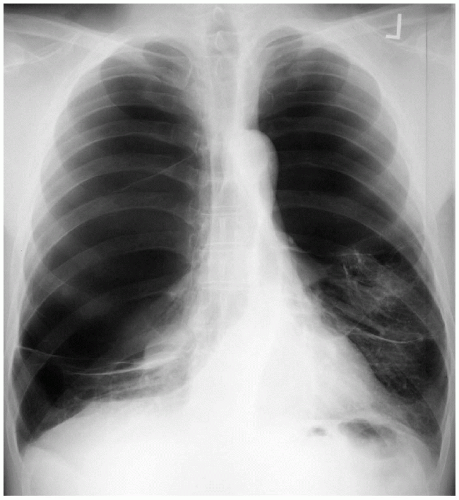
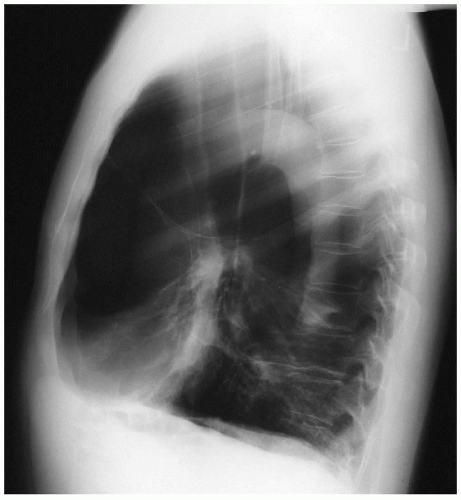
▪ Chest X-rays
Chest X-ray Report
There is a lack of lung markings in both the right and left lung fields. There are bilateral transverse markings suggestive of septation in a giant bulla. The diaphragms are flattened, and the anteroposterior diameter is widened, suggestive of chronic obstructive pulmonary disease. The heart is normal in size. There are no pleural effusions.
Differential Diagnosis
Often, the absence of lung markings is associated with the diagnosis of pneumothorax. It is important not to make this general assumption. A pneumothorax of this size would require a tube thoracostomy, which in this case would be erroneous and would subject the patient to unnecessary complications, such as a significant air leak and loss of tidal volume. Tension pneumothorax may also be present in a patient who lacks lung markings on chest x-ray. When evaluating an x-ray of a patient with a suspected diagnosis of tension pneumothorax, the position of the trachea should be noted. In this case, the positions of the trachea and mediastinum are midline, which suggests against the diagnosis of a tension pneumothorax. Furthermore, bilateral pneumothorax, although possible, is very rare.
Discussion
Pulmonary blebs are due to subpleural alveolar rupture, which results in an intrapleural air space. They are small and are usually located in the apices of the upper lobes; they can also be found at the apices of the lower lobe. Blebs can be acquired as a consequence of chronic obstructive lung disease or can be present at birth and enlarge over time. Typical presentation includes a tall, thin male between the ages of 20 and 40 years who presents with shortness of breath and is found to have a unilateral spontaneous pneumothorax. The first occurrence of a spontaneous pneumothorax can be observed if the pneumothorax is small; in patients with a large pneumothorax, a tube thoracostomy is necessary. The incidence of a second pneumothorax is 20%, and it is 50% for a third pneumothorax. Patients with recurrent pneumothoraces require excision of the bleb to prevent recurrences. In contrast to blebs, bullae are larger than 1 cm and are not sharply demarcated from surrounding lung. Instead, the walls are made up of destroyed lung and a thin membrane composed of visceral pleura and connective tissue. Bullae communicate with bronchi at the base of the bullae. They can form anywhere in the lung but are usually found in the upper lobes. Typically, bullae are divided into two groups: they may be associated with normal lung parenchyma (20%) or with diffuse emphysema (80%). Patients with bullae and normal lung parenchyma have some compression of adjacent lung but near-normal pulmonary function. Bullae with diffuse emphysema may be the result of severe diffuse panacinar emphysema and can be multiple and bilateral. Giant bullae fill at least one half of the hemithorax.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree