Bullous and Bleb Diseases of the Lung
Talat Chughtai
Emilie Perron
Mathieu Simon
Jean Deslauriers
Bullae were defined at the 1959 Ciba Symposium as emphysematous spaces larger than 1 cm in diameter in the inflated lung, usually but not necessarily demarcated from surrounding lung by curved hairline shadows. Most bullae are secondary to emphysema; pathologically, they consist of enlarged airspaces covered by visceral pleura and connective tissue. Diffuse emphysema associated with multiple bullae is classified as bullous emphysema.
In general, bullous emphysema is treated expectantly. Surgical treatment is usually reserved for the management of specific complications such as pneumothorax or infection. Advances in surgical techniques, specifically minimally invasive techniques, have allowed surgery to be offered to a broader range of patients. The observed benefits, however, may not be sustained long-term.
Terminology and Classification
Blebs
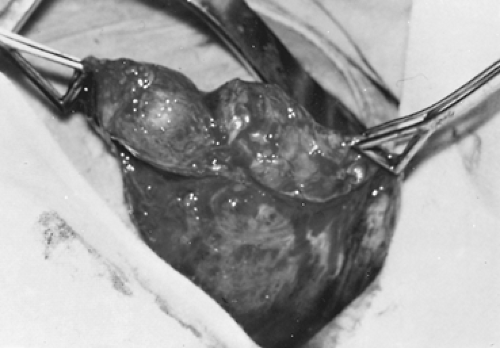
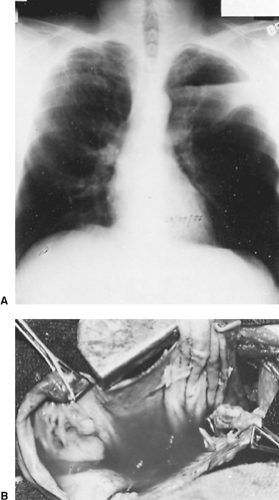
Miller68 defined pulmonary blebs (Fig. 87-1) as well-circumscribed intrapleural airspaces separated from the underlying parenchyma by a thin pleural covering. They result from subpleural alveolar rupture, which occurs when the elastic fibers in the alveoli have been stretched beyond the breaking point. The outer wall of a bleb is made up of visceral pleura; the underlying lung is normal. Blebs are small and peripheral and most are located at the lung apices. Not uncommonly, blebs will coalesce to form larger airspaces or even giant bullae. In 2007, Amjadi et al.,3 in examining the prevalence of blebs in 250 healthy adults who were undergoing thoracoscopic sympathectomy for essential hyperhydrosis, found a 6% prevalence of blebs. Individuals who had blebs versus those without blebs had a significantly lower body mass index (BMI) and trended toward being more likely to smoke.
Bullae
Bullae can be associated with any variety of emphysema. Their walls are made up of destroyed lung; inside, they are crisscrossed by fibrous strands that are the remnants of interlobular septa. Small bronchial openings are usually located at the base of a bulla. Reid94 distinguished three types of bullae: Type 1 projects from the pleural surface like a mushroom; it has a narrow neck and an empty sac except for a few strands of tissue. It represents a small amount of greatly overdistended lung. Type 2 has a broad neck, is produced by relatively less overinflation of a shallow subpleural layer of lung, and its sac usually contains strands of tissue, most frequently near its base. Type 3 has only moderate protrusion above the pleural surface and represents the least overinflation of a much deeper region of the lung. In addition, this bulla has no well-defined neck, and contains emphysematous lung evenly throughout.
Most surgeons prefer a more practical classification52 of bullous emphysema that is based on the presence or absence of significant anatomic emphysema in the nonbullous lung.
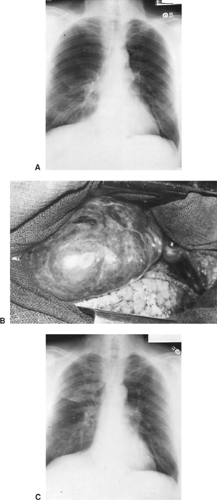
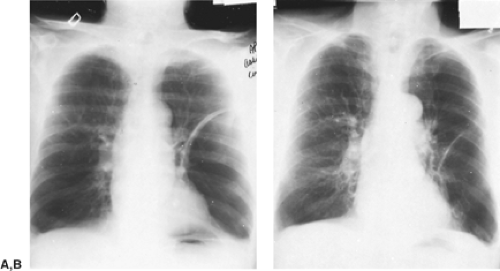
Type I: Bullae and Almost Normal Underlying Lung
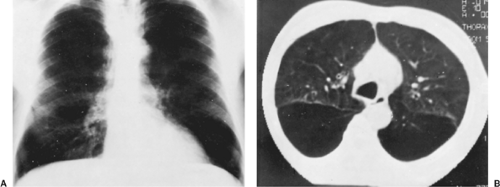
Type I bullae (Fig. 87-2) account for approximately 20% of all bullae. They are well demarcated from surrounding lung, are usually located at the apex, and typically have a narrow base of implantation. When the bulla becomes larger or even giant (fills half or more of the hemithorax), it displaces adjacent lung,
but patients remain relatively symptom-free with almost normal pulmonary function. If the bulla compresses normal lung to the point of causing symptoms, resection may be indicated.
but patients remain relatively symptom-free with almost normal pulmonary function. If the bulla compresses normal lung to the point of causing symptoms, resection may be indicated.
Type II: Bullae Associated with Diffuse Emphysema
Type II bullae are seen in over 80% of patients with bullous lung disease. Initially at least, these bullae represent simply a local exaggeration of diffuse panacinar emphysema (Fig. 87-3). These bullae are often multiple and bilateral, and they vary considerably in extent and size. Patients’ symptoms
depend on the severity of underlying emphysema rather than bulla size.
depend on the severity of underlying emphysema rather than bulla size.
Table 87-1 Wakabayashi Classification of Emphysematous Bullae | |
|---|---|
|
Vanishing lungs (type III bullae) feature complete loss of parenchymal architecture, distended airspaces disseminated throughout both lung fields, and absence of well-demarcated bullae.
High-resolution computed tomography (CT) may help in distinguishing type I bullae from diffuse bullous emphysema. Mineo and colleagues69 proposed a new classification based on their hypothesis that bigger bullae, in relation to residual volume, predicted benefit from bullectomy in terms of dyspnea index as well as improvement in forced expiratory volume in 1 second (FEV1) and quality of life. They showed that a ratio of bulla to residual volume of greater than 30% predicted better outcome. Their classification divided the ratio of bulla to residual volume as <20%, 20 to 30%, and >30%. Wakabayashi125 developed a classification system (Table 87-1) based on CT scan of the chest and findings at thoracoscopy. Type 2 bullae are the most common cause of spontaneous pneumothorax and type 3 are the most common in bullous emphysema. Giant bullae are either type 1 or type 4. Another practical classification of bullous emphysema is the one proposed by DeVries and Wolfe.23 In their system, group I includes patients with a single bulla and a normal underlying lung, while group II patients have multiple bullae but a still normal lung. Groups III and IV comprise bullous disease in patients with generalized emphysema and those with other diffuse lung diseases (group IV), respectively. With this classification, patients in groups I and II have good functional results following surgery compared with those in groups III and IV. These diffuse lung diseases may include histoplasmosis, idiopathic pulmonary fibrosis, pneumoconiosis, scleroderma, silicosis, Ehlers-Danlos syndrome, alpha1-antitrypsin deficiency, and others. Lymphangiomyomatosis (LAM) has also been described in association with a symptomatic giant bullae by Fujiwama29 in a 33-year-old premenopausal woman. This patient was successfully treated with bullectomy plus hormonal therapy.
Origin and Behavior of Bullous Lung Disease
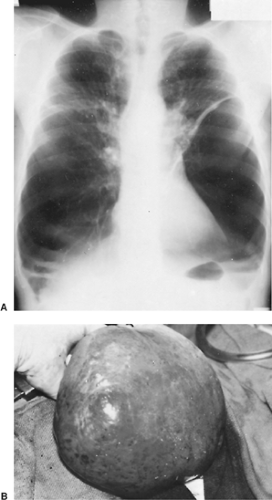
Controversial views on the origin and behavior of bullous lung disease are based on early observations made by Baldwin and colleagues5 and Cooke and Blades,18 who believed that a ball-valve mechanism, present in the bronchial communication between the bulla and adjacent airways, was responsible for progressive enlargement of the bulla. It was postulated that because destroyed and inflamed bronchi existed at the base of the bulla, gas was allowed to enter the airspace but not allowed to leave. The bulla thus became progressively larger over time because of increased intrabullous pressure, which eventually caused compression and collapse of the unsupported adjacent emphysematous lung tissue. A giant unilateral bulla may even cause bilateral lung compression, as described in a report by Van Natta121 in 2007 (Fig. 87-4). The physiologic alterations associated with
a bulla were therefore those of a space-occupying lesion that compressed and interfered with adjacent normal and functional lung. FitzGerald and coworkers26 further believed that the resulting decrease in lung volume and loss of elastic recoil caused by emphysema would lead to relaxation of peribronchial tension, narrowing of small airway diameter, and eventually expiratory obstruction affecting the less diseased portions of the lung.
a bulla were therefore those of a space-occupying lesion that compressed and interfered with adjacent normal and functional lung. FitzGerald and coworkers26 further believed that the resulting decrease in lung volume and loss of elastic recoil caused by emphysema would lead to relaxation of peribronchial tension, narrowing of small airway diameter, and eventually expiratory obstruction affecting the less diseased portions of the lung.
Morgan and colleagues74,76 have shown—through dynamic CT observations, intrabullous gas and pressure measurements, as well as pathologic examination—that bullae are unlikely to grow and behave in the manner previously thought. According to these researchers and to Klingman and associates,52 the lung surrounding a bulla is less compliant than the bulla itself; therefore the pressure required to inflate it exceeds the pressure necessary to inflate the bulla. In other words, when bulla and lung are exposed to the same negative intrapleural pressure, the bulla is preferentially and always completely full before the adjacent lung. Consequently, once a parenchymal weakness exceeds a certain size, it results in a space within the lung that fills preferentially. Progressively, the forces of elastic recoil produce more retraction of the adjacent lung away from the bulla, and this action tends to further enlarge the bulla.
Based on this understanding, the purpose of surgery in bullous lung disease may be more to permit the lung to regain its architecture and elasticity than to remove a space-occupying lesion.
Other diverse associations with bullae have been described. Hii42 reported on 10 patients with a history of marijuana smoking who presented with symptomatic bullae. They hypothesized that marijuana smokers had larger inspiratory volumes and held their breath longer compared with cigarette smokers, which could potentially cause barotrauma. Van Der Klooster120—after reporting a case in a 40-year-old man with bilateral symptomatic bullous disease—suggested that cocaine use may be associated with premature bullous emphysema. Bullous emphysema has also been described in a 2-year-old patient 3 months after being treated for Legionnella pneumonia. Gervais32 reported this as a rare complication that ultimately required a lobectomy to prevent pneumothorax.
Surgical Management of Bullous Disease
Among all procedures that have ever been promoted for the surgical management of chronic obstructive lung disease, the only operation that has stood the test of time is “bullectomy,” in which distended airspaces are resected to allow the reexpansion of restricted but potentially functional adjacent lung tissue.
Rationale and Indications for Surgery
Nondyspneic Patients
Surgery for Complications of the Bulla.
In patients without ventilatory symptoms (Table 87-2), surgical intervention is mostly indicated for complications such as pneumothorax, infection, or hemoptysis that are clearly attributable to the bulla.
Gaensler and coworkers30 noted that bullous emphysema predisposes to pneumothorax and that, in such circumstances, a pneumothorax can be troublesome because of further reduction of function in already compromised patients, prolonged air leaks often unresponsive to tube drainage, and higher risk for recurrence than in patients with primary spontaneous pneumothorax. In a series of 67 patients with secondary spontaneous pneumothoraces, Tanaka and colleagues113 showed that the most common underlying diseases were emphysema and tuberculosis and that the most frequent presenting symptom was dyspnea. Pneumothorax was the most common complication, occurring in 107 patients, in a series (reported by Potapenkov90) of 118 patients who had complications of bullous lung diseases. In this series, 8 patients had respiratory failure and 2 had recurrent hemoptysis.
Table 87-2 Rationale and Indications for Surgery in Patients With Complications of Their Bullae | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
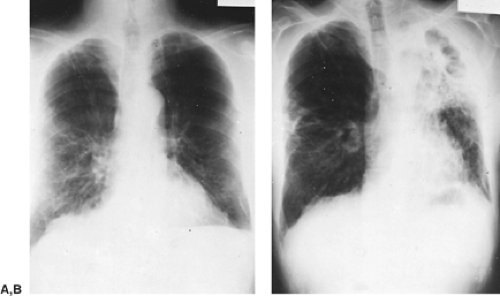
Infection of bullae is unusual; most bullae containing a fluid level (Fig. 87-5) are only the site of an inflammatory reaction secondary to peribullous infection. Surgery is not indicated for this problem alone, and Rubin and Buchberg99 showed that fluid resorption may be associated with significant shrinkage and resolution of the bulla (autobullectomy) (Fig. 87-6). In a series of 10 patients with fluid within a bulla reported by Mahler and colleagues,61 the air–fluid levels disappeared in 3 days to 36 weeks (mean 11 weeks), whereas the alveolar infiltrate generally cleared at a slower rate. Rothstein98 has also shown that the usual course of events in bullae infected by Mycobacterium tuberculosis was that of gradual shrinkage and eventual replacement of the previous radiologic shadows by nondescript and linear densities.
Truly infected bullae (Fig. 87-7) should be managed conservatively, even though medical treatment is often unsuccessful because of the poor communication between the infected bulla and the bronchial tree. Surgical indications for resection are essentially the same as for primary lung abscesses; they include failure of response to a 6-week course of adequate medical management, suspicion of occult bronchial carcinoma, and specific complications, such as hemoptysis or free pleural space rupture. Dean and colleagues21 showed that percutaneous drainage of the infected bulla should be considered in these high-risk patients.
Hemoptysis from an eroded artery is even more uncommon than infection. Berry and Ochsner7 reported one of the few cases in which hemoptysis was thought to be secondary to rupture of thin-walled pulmonary vessels passing through the alveolar wall and fibrous septa of a bulla. Because hemoptysis is seldom
associated with bullous emphysema, another lesion in a different lung zone that could account for the bleeding should always be ruled out before surgery.
associated with bullous emphysema, another lesion in a different lung zone that could account for the bleeding should always be ruled out before surgery.
Gaensler and associates31 and Witz and Roeslin129 have described cases in which chest pain was the main symptom and sole indication for surgery. The pain was most often retrosternal and related to exercise, and in some cases it mimicked angina. This symptom was explained by overdistention of the bulla during hyperventilation with secondary mediastinal shift. All patients improved after surgical removal of their bullae.
Primary lung cancer closely associated with a large bulla was analyzed in 32 patients by Tsutsui and colleagues118 in an attempt to elucidate radiographic features of the tumor. They proposed three radiographic patterns of neoplasm development: nodular opacity within or adjacent to the bulla, partial or diffuse thickening of the bulla wall, and secondary signs of the bulla, such as changed diameter, fluid retention, and pneumothorax. Maki et al.62 recently published a report of 20 patients with histologically proven bronchogenic carcinoma associated with bullous lung disease. They classified the CT appearance of the cancer into three types (Fig. 87-8): type 1, a nodule or mass extending from the bulla; type 2, a nodule or mass within the bullae; and type 3, a density extending along the bulla’s wall. The histologic types of the 20 carcinomas included adenocarcinoma (9), squamous cell carcinoma (7), adenosquamous carcinoma (3), and small-cell carcinoma (1). The authors suggest paying close attention and even performing a biopsy of any abnormal densities associated with a bulla owing to the potential of its being a carcinoma. Mizuguchi et al.71 suggest that any lesion associated with a bulla on CT scan indicates the need for its complete surgical removal. They report on a rare case of asymptomatic bilateral bullae and an associated lesion on one of the bullae that was followed for 1 year. The patient was ultimately found to have adenocarcinoma associated with the bulla on the suspicious side and a papillary adenocarcinoma on the wall of the bulla on the unsuspicious other side. This case of synchronous cancers associated with bullae led the authors to suggest mandatory pathologic evaluation of all resected bullae. Stoloff and associates111 investigated the population of Philadelphia between 1947 and 1967 and found that the frequency of lung cancer in men without emphysema was 0.19%, whereas in individuals with bullous emphysema, the frequency was 6.1%. Similarly, Goldstein and
coworkers33 found that in 411 patients with bullous emphysema, 4.3% had lung cancer. Nickoladze82 proposed the following hypothesis to explain this phenomenon: (a) lung cancer occurs more frequently in lung scars that favor development of bullae, (b) dystrophic changes in lung parenchyma caused by bullous emphysema promote development of lung cancer, and (c) bullae are unventilated or poorly ventilated spaces in which carcinogens linger and predispose to the development of lung cancer. It is important to remember that it is often difficult to make a definite diagnosis of lung cancer within a bulla and that thoracotomy may be necessary to confirm the presumption of neoplasm.
coworkers33 found that in 411 patients with bullous emphysema, 4.3% had lung cancer. Nickoladze82 proposed the following hypothesis to explain this phenomenon: (a) lung cancer occurs more frequently in lung scars that favor development of bullae, (b) dystrophic changes in lung parenchyma caused by bullous emphysema promote development of lung cancer, and (c) bullae are unventilated or poorly ventilated spaces in which carcinogens linger and predispose to the development of lung cancer. It is important to remember that it is often difficult to make a definite diagnosis of lung cancer within a bulla and that thoracotomy may be necessary to confirm the presumption of neoplasm.
Other unusual complications of bullous emphysema include cervical herniation of an apical bulla, as in the case reported by Victor and colleagues,123 and in dysphagia, as reported by Ueda and associates.119 Placental transmogrification (the presence of placental-type chorionic villi) has also been seen on histologic examination of resected bullae by Khoury et al.51
Preventive Surgery.
Preventive surgery is defined as resection of asymptomatic bullae on the premise that most of them will ultimately lead to serious and irreversible complications. It is also assumed that with longer periods of compression, it is less likely that function will return to normal even if the lung appears to reexpand well. This, in part, relates to the loss of surfactant in chronically functionless parenchyma and to the development of various degree of interstitial fibrosis.
The role of preventive surgery is unclear, however, because little is known about the natural history of untreated asymptomatic bullae. Boushy and associates10 observed that apical bullae tend to enlarge, but this enlargement was not seen in every case and could not be predicted. Furthermore, these investigators were unable to document any relationship between a change in a bulla’s size and the deterioration of pulmonary function. Ribet95 reported 23 patients in whom the bullae were first discovered on chest radiography before the appearance of any symptoms. In this group, only 4 of 23 patients were still symptomless when surgery was performed, with a delay between discovery of the bulla and surgery of 0 to 12 years (mean 39 months). Ribet95 concluded that giant bullae may be symptomless but remain so in a minority of cases, and that symptomless bullae can suddenly become complicated and cause death despite emergency aspiration. As a general principle, a planned operation is always better and associated with less morbidity than an emergency operation.
Most researchers agree that preventive surgery is legitimate when the bulla occupies half or more of the hemithorax,
compresses normal lung, or has enlarged over a period of years. Spear and associates109 believed that any bulla occupying one-third or more of the hemithorax would ultimately be associated with impaired drainage, infection, and permanent tissue damage to the adjacent compressed lung.
compresses normal lung, or has enlarged over a period of years. Spear and associates109 believed that any bulla occupying one-third or more of the hemithorax would ultimately be associated with impaired drainage, infection, and permanent tissue damage to the adjacent compressed lung.
Dyspneic Patients
Based on physiologic observations, the removal of bullae in patients with emphysema and dyspnea can be performed for the following reasons: removal of a space-occupying and possibly compressive lesion, reduction in expiratory airway resistance, and reduction of dead-space ventilation (Table 87-3).
As summarized by De Giacomo and colleagues,22 the physiopathologic basis of respiratory improvement after bullectomy relates to the reduction of residual volume (RV) and thoracic hyperinflation, reexpansion of adjacent functional lung, and improvements in diaphragmatic contractility, chest wall mechanics, and intrathoracic hemodynamics.
Removal of a Space-Occupying Lesion.
Compression of relatively healthy lung near the bullae may impair overall gas exchange, with low ventilation/perfusion ratios in the restricted lung zone. Expansion of previously restricted lung should therefore increase vital capacity (VC) and arterial oxygen saturation.
High intrathoracic pressures generated by the bullae may also result in major hemodynamic dysfunction. Expiratory compression of the pulmonary arterial system and systemic venous return may decrease cardiac output both at rest and, more importantly, during exercise. By lowering intrathoracic pressures through the removal of large bullae some of these hemodynamic parameters may be corrected and the degree of dyspnea decreased.
Bullous emphysema, particularly when localized in the lower lobes, may finally have a deleterious effect on the function of the diaphragm and the chest wall muscles, including the intercostals. In one patient reported by Travaline and colleagues,116 impairment of diaphragmatic function was dramatically corrected by bullectomy, which restored the diaphragm to a more normal configuration with significant improvement in its strength. Removal of a large bulla is also likely to improve chest wall mechanics.
Reduction in Expiratory Airway Resistance.
Ting and colleagues114 showed that bullae have little if any elastic recoil. At low volume, small variations in pressure bring important volumetric changes. At a critical level, however, compliance becomes extraordinarily low and the bulla cannot be stretched any more. Bullae can be compared with paper bags that are extremely compliant until they are full, when they become tense.
In association with emphysema, the low compliance of the bulla significantly decreases the elastic recoil of the intervening lung and reduces peribronchial tension. Ultimately, it creates an extrinsic airway obstruction affecting the less diseased portions of parenchyma around the bulla.
Removal of bullae may improve the elastic recoil of the previously restricted lung tissue, thus reducing the tendency of airways to collapse on exhalation.
Reduction of Dead-Space Ventilation.
If a bulla is well ventilated and underperfused, the objective of surgery is to reduce this physiologic dead space and thereby decrease the work of breathing. Isotopic perfusion/ventilation studies have shown, however, that most bullae are neither perfused nor ventilated. The bulla was acting as a site of significant dead-space ventilation in only 1 of 14 patients studied by Pride and coworkers.93
Selection of Patients for Surgery
Because of the emergence of modern techniques for lung imaging and functional evaluation, guidelines have been proposed to help select those individuals most likely to benefit from surgical intervention (Table 87-4). Although no single preoperative test is considered an absolute predictor of improvement, the main determinants of a successful outcome after surgery are the size of the bulla, the condition of the rest of the lung, and the evidence of compression. The best results are obtained in patients with large bullae and in whom compression of a significant volume of potentially functional surrounding lung parenchyma can be demonstrated. This concept may be best summarized by the ratio of bulla to residual volume ratio proposed by Mineo,69 as previously described.
Because these are the premises for successful surgery, a complete evaluation should attempt to answer the following questions: (a) Is there a localized or enlarging bulla or both? (b) Is the bulla nonfunctional and does it compress adjacent lung, mediastinum, and/or diaphragm? (c) Can the compressed lung reexpand, and what is its potential to function once reexpanded? (d) What is the extent and severity of emphysema in the remaining lung? (e) What is the level of cardiac performance?
(f) Does the patient have significant associated comorbidities, weight loss, or both? (g) Can the patient withstand an operation?
(f) Does the patient have significant associated comorbidities, weight loss, or both? (g) Can the patient withstand an operation?
Table 87-3 Rationale and Indications for Bullectomy in Dyspneic Patients With or Without Diffuse Emphysema | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Table 87-4 Selection of Patients for Surgery | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Anatomy of the Bullous Area
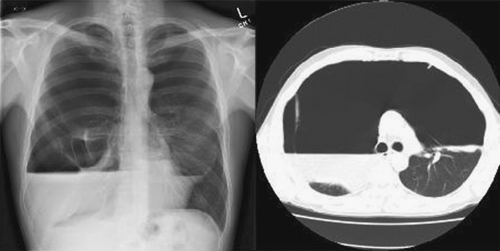
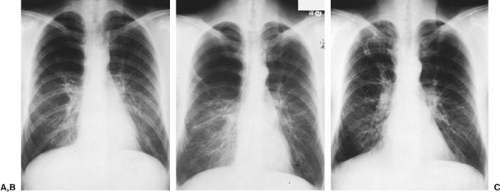
Bullae are recognized by increased radiolucencies (avascular areas) surrounded by arcuate hairline shadows (cyst wall). Their diagnosis, number, location, and volume can be estimated from standard radiographs, but CT scanning should be used to determine the true size of a given bulla. The observation that a bulla has enlarged over time is pertinent, especially if the enlargement is associated with a concomitant deterioration in pulmonary reserve (Fig. 87-9).
CT scanning is a sensitive diagnostic tool because it clearly shows the full extent and anatomic severity of bullous disease, features often not discernible on simple posteroanterior and lateral radiographs (Fig. 87-10). CT scanning may also help in differentiating a pneumothorax from a large emphysematous bulla. Ultrasound has also been reported to be useful in distinguishing between pneumothorax and bullae. Simon et al.106 described visualization of the pleural layers “sliding” with bullae, but not pneumothorax, as well as lack of reverberation artifact, “comet tailing,” coming from the visceral pleura, seen in pneumothorax but not with bullae. Ultrasound is well known to be user-dependent, however.
With the help of CT scanning, Morgan and associates74 were able to differentiate between patients with generalized emphysema that was locally worse in the area of the suspected bulla and patients with well-defined bullae that were potentially operable. They also used CT scanning to measure the volume and ventilation of bullae, and these measurements confirmed that most true bullae do not contribute to ventilation.
Morgan and Strickland75 also showed that CT scans obtained during expiration (dynamic CT) can offer important advantages
over traditional radiology. According to these researchers, the advantages of CT scanning are (a) clarification of features visible on plain radiographs, such as number, size, and position of bullae; (b) disclosure of features invisible on the plain radiographs, such as small bullae at the lung apices or in the costophrenic sinuses; (c) assessment of features often obscured by other diseases on standard radiographs, such as scoliosis; and (d) clarification and assessment of associated lung diseases.
over traditional radiology. According to these researchers, the advantages of CT scanning are (a) clarification of features visible on plain radiographs, such as number, size, and position of bullae; (b) disclosure of features invisible on the plain radiographs, such as small bullae at the lung apices or in the costophrenic sinuses; (c) assessment of features often obscured by other diseases on standard radiographs, such as scoliosis; and (d) clarification and assessment of associated lung diseases.
As suggested 20 years ago by Carr and Pride,14 CT scanning has now become the ultimate imaging technique to delineate the anatomy of bullous lung disease.
In general, the best results after bullectomy are obtained with bullae occupying one-third to one-half of one or both hemithoraces (giant bullae); the results are worse when bullae are small, multiple, and bilateral. In an interesting study of 25 patients, Baldi and associates4 showed that, statistically, the radiographic volume of a bulla was the single most important factor determining the increase in FEV1 after bullectomy (r = 0.80, p < 0.0001).
Function of the Bulla
The distinction between communicating and noncommunicating bullae may be relevant to the understanding of the pathophysiology of a given bulla, but it is relatively unimportant in making a surgical decision. Pulmonary areas that are to be resected, however, must be areas of poor perfusion.
Most bullae are not ventilated or poorly ventilated, so the change in size in inspiration and exhalation is small. The amount of trapped air in the bulla, however—as estimated by the difference between functional residual capacity measured by the helium dilution method and by plethysmography—is large. This difference reflects the true volume occupied by the bulla. After resection of such bullae, an increase in VC and FEV1 is expected. Morgan and associates74 have shown by CT studies of the volume of bullae and of their VC that with few exceptions, little change in the volume of true bullae occurs between full inspiration (mean 1,454 mL) and full exhalation (mean 1,333 mL).
Bullae that communicate freely have large volume variations between inspiratory and expiratory images but small volume difference between plethysmographic and helium dilution measurements. Little change is expected in postoperative VC, but FEV1 improves if the space taken by the bulla is replaced by normal lung parenchyma.
Isotope scans can also be used to determine the function of a bulla with respect to perfusion. It is particularly helpful to demonstrate that the bulla to be resected is not perfused or is underperfused when compared with the adjacent lung, thus improving the chances of a good outcome after bullectomy (Fig. 87-11).
Compression Index
Once it is decided that a symptomatic space-occupying bulla is present, the next step is to demonstrate that it is compressive and prevents adequate expansion of adjacent parenchyma. This is a key consideration, because overstretching of unrestricted lung may ultimately lead to some functional loss. Laros and colleagues55 noted that in patients with vanishing lung syndrome, for instance, the destroyed lobe had a buffer function in preventing overexpansion of the remaining lung.
Brochard and associates11 described a simple but effective compression index based on initial radiographic data. Patients were rated 0 to 6, according to the number of compression signs present: 1 = vascular crowding in the parenchyma adjacent to the hyperinflated lung; 2 = arcuate displacement of blood vessels in the periphery of the bulla; 3 = displacement of the hilum; 4 = mediastinal displacement during inspiration, exhalation, or both; 5 = anterior mediastinal herniation of the lung; and 6 = displacement of lung fissures. They were able to correlate subjective results of surgery with the severity of compression.
Most of these signs can readily be seen on standard radiog- raphy or contrast-enhanced CT of the chest. Although pulmonary artery angiography is no longer routinely used and has been replaced by contrast-enhanced CT, it may occasionally be
useful to document vascular crowding (Fig. 87-12) and assess capillary filling in the periphery of adjacent parenchyma. Thinning or disruption of pulmonary capillaries (Fig. 87-13) suggests the presence of widespread emphysema and poor response to surgery.
useful to document vascular crowding (Fig. 87-12) and assess capillary filling in the periphery of adjacent parenchyma. Thinning or disruption of pulmonary capillaries (Fig. 87-13) suggests the presence of widespread emphysema and poor response to surgery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree