Midulla et al. [20]
Number of patients
16
Age range
2–32 m
Sedation
LA
Number of aliquots
2
Lavage volume
20 ml
BALF recovered %
Mean ± SD
43.1 ± 12.2
Median
42.5
Range
20–65
Cell count (104 cells · ml−1)
Mean ± SD
59.9 ± 8.2
Median
51
Range
20–130
AM %
Mean ± SD
86 ± 7.8
Median
87
Range
71–98
Lym %
Mean ± SD
8.7 ± 5.8
Median
7
Range
2–22
Neu %
Mean ± SD
5.5 ± 4.8
Median
3.5
Range
0–17
Eos %
Mean ± SD
0.2 ± 0.3
Median
0
Range
0–1
Normal values of BALF lymphocyte subsets in children resemble those found in healthy adults, except for the CD4/CD8 ratio, which is often lower in children, possibly because children frequently suffer from viral infections [7, 8].
The concentration of serum-derived proteins is higher in children than in adults, whereas locally produced mediators do not differ (Tables 2.2 and 2.3). Surfactant phospholipid concentrations are higher in 3–8 year old than in older children, whereas surfactant protein concentrations are independent of the child’s age.
Table 2.2
Concentration (mg L−1) of serum-derived proteins in bronchoalveolar lavage fluid (BALF) from control children
Midulla et al. [20] | ||
|---|---|---|
Number of patients | 7 | |
Age | 1–3 y | |
Total protein | Mean ± SD | 108 ± 39 |
Median | 67 | |
Range | 44–336 | |
Albumin | Mean ± SD | 58 ± 26 |
Median | 29 | |
Range | 14–210 | |
Table 2.3
Concentration (mg L−1) of locally produced mediators in bronchoalveolar lavage fluid (BALF) from control children
Midulla et al. [20] | ||
|---|---|---|
Number of patients | 7 | |
Age | 1–3 y | |
Fibronectin | Mean ± SD | 172 ± 83 |
Median | 80 | |
Range | 25–640 | |
Hyaluronic acid | Mean ± SD | 26 ± 5 |
Median | 18 | |
Range | 16–45 | |
Indications for Bronchoalveolar Lavage
BAL is performed for diagnostic, therapeutic and research applications. The most important indication for BAL in children is in the work-up of infectious diseases. BAL can be done in both immunocompromised (lung transplant, HIV infection, chemotherapy) and immunocompetent children (chronic pneumonia, tuberculosis, cystic fibrosis). Other indications for BAL include non-specific chronic respiratory symptoms, non-specific radiological findings, and clinical symptoms suggestive of chronic interstitial lung disease (CILD; diffuse parenchymal lung disease, DPLD).
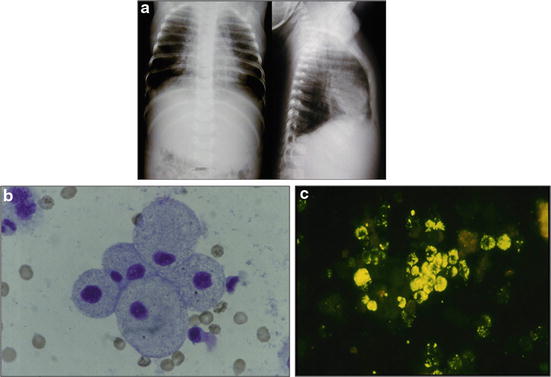
BAL results should be analysed carefully; in fact, BAL is diagnostic only when pathogens not usually found in the lung are recovered, such as Pneumocystis jirovecii, Toxoplasma gondii, Strongyloides stercoralis, Legionella pneumophila, Histoplasma capsulatum, Mycobacterium tuberculosis, Mycoplasma pneumoniae, influenza virus, and respiratory syncytial virus. The isolation of herpes simplex virus, cytomegalovirus, Aspergillus, Candida albicans, Cryptococcus, and atypical mycobacteria from BALF is not diagnostic but may contribute to diagnosis and management of infectious diseases (Fig. 2.1). The presence of equal to or more than 104 colony-forming units/ml BALF will identify patients with bacterial pneumonia with reasonable accuracy. Hence, when evaluating the microbiological results, the physician must take into account the underlying disease and the overall clinical picture.