CHAPTER
12
Bradycardia and Blocks
SINUS BRADYCARDIA AND SINOATRIAL (SA) NODE DYSFUNCTION
General Information
○Impairment of the sinoatrial (SA) node ability to generate propagated impulses
▪ Consider a 2:1 sinus exit block.
Epidemiology and Clinical Features
○Sinus bradycardia occurs in 1/600 patients over 65 years of age.
○Variable symptoms:
▪ Asymptomatic to fatigue, exercise intolerance, dyspnea, presyncope, or syncope.
▪ May lead to angina or heart failure.
○Often these patients are highly sensitive to cardiac medications (non-dihydropyridine calcium-channel blocker [ND-CCB], β-blockers, and antiarrhythmic drugs [AAD]).
○Frequently coexists with atrial tachyarrhythmia (atrial fibrillation [AF] and atrial flutter [AFL]).
Etiology
Intrinsic
○Degenerative: Idiopathic age-related fibrosis (most common)
▪ SA node fibrosis: Inappropriate sinus bradycardia and exaggerated overdrive suppression
▪ Atrial myocardial fibrosis: Propensity to AF or AFL
▪ Atrioventricular node (AVN) fibrosis: atrioventricular (AV) block
○Myocardial ischemia
▪ SA node: Supplied by right coronary artery (60%) or left circumflex artery (40%)
▪ Sarcoidosis, amyloidosis, hemochromatosis
○Inflammatory
▪ Pericarditis, myocarditis
○Familial diseases
▪ Myotonic dystrophy, Friedrich ataxia, Na+ channel mutations
○Collagen vascular disease
▪ Systemic lupus erythematosus, rheumatoid arthritis, scleroderma, ankylosing spondylitis
○Trauma or surgery
▪ Valve replacement, ablation, atrial septal defect (ASD) repair, heart transplantation
Extrinsic
○Drugs
▪ AADs (class I, class III), β-blockers, diltiazem/verapamil, digoxin, ivabradine
▪ Sympatholytic (reserpine, methyldopa, clonidine), alcohol, lithium
○Electrolyte imbalances
▪ Potassium, calcium, or magnesium
○Metabolic
▪ Hypothyroidism, hypothermia
○Myocardial ischemia
▪ Inferior myocardial infarction (MI): Neural reflex
○Autonomic-mediated syndromes
▪ Neurocardiogenic syncope, carotid-sinus hypersensitivity
▪ Situational: Coughing, micturition, defecation, vomiting
○Infection
▪ Chagas, endocarditis, Salmonella, diphtheria, rheumatic fever, viral myocarditis
Classification
○ Inappropriate sinus bradycardia
▪ Sinus bradycardia in the absence of an appropriate cause or that results in symptoms
○ Tachycardia-bradycardia syndrome
▪ Atrial tachycardia (AT; usually AF) alternating with sinus bradycardia, sinus pauses, and/or an AV block
○ Intermittent sinus pauses include:
▪ Sinus arrest: Transient cessation of SA node firing (>2 seconds)
▪ Sinoatrial (SA) exit block: Depolarization fails to exit the SA node (the RR interval is unchanged).
• Type 1 (Mobitz): The time between sinus firing and when the atrial capture progressively prolongs leading to gradual shortening in the PP intervals before the pause (pause PP < two preceding PP).
• Type 2 (Mobitz): The PP interval is constant before and after the pause and is a multiple (2×, 3×…) of the basic PP interval.
○ Chronotropic incompetence: Inappropriately low heart rate response during exercise.
▪ Absolute: Inability to increase heart rate to 60% age-predicted target (220 – age) or to >100–120 bpm.
▪ Relative: Able to reach target heart rate but at a significant delay with reduced exercise tolerance.
12-Lead ECG
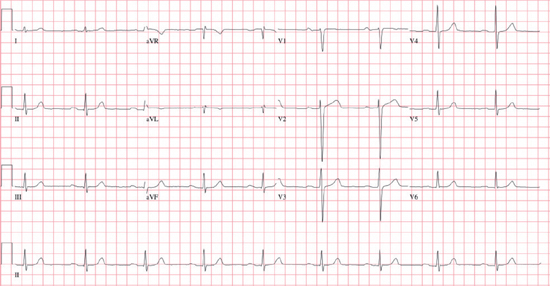
○Heart rate <60 bpm with characteristics of sinus rhythm
▪ 1:1 P:QRS relationship
• Every P wave is followed by a QRS complex and every QRS complex is preceded by a P wave.
▪ Sinus P-wave morphology and axis
• Upright in I, II, aVF, and V2–V6 (best seen in II)
• Inverted in aVR
• Upright or biphasic in V1 and V2; upright in V3–V6
Other Investigations
○Carotid sinus massage or tilt table testing to identify neurocardiogenic causes
○Treadmill stress test
▪ Assesses the chronotropic response to exercise
○Ambulatory electrocardiogram (ECG) monitoring (Holter, event monitor, ILR)
▪ Correlates symptoms with the electrical disorder
○Assessment of intrinsic heart rate (IHR: Rarely performed)
▪ IV atropine 0.04 mg/kg + IV propranolol 0.2 mg/kg
▪ Predicted IHR = 118.1 – [0.57 × age]:
• Low IHR = intrinsic sinus node dysfunction (SND)
• Normal IHR = autonomic imbalance
○Electrophysiology study (see Assessment of SA Node Function section)
Management
Acute Management
○Atropine or isoproterenol
Chronic Management
○Stop medications that suppress the SA node (e.g., β-blockers, verapamil/diltiazem, digoxin).
○Pacemaker indications:
▪
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


