Chapter 105
Brachiocephalic Artery
Surgical Treatment
Sapan S. Desai, Hazim J. Safi
Based on a chapter in the seventh edition by David L. Lau and Hazim J. Safi
The innominate, left common carotid, and left subclavian arteries constitute the branches of the transverse aortic arch. Known as the brachiocephalic arteries, together these vessels supply blood to the upper extremities, head, and neck. Atherosclerosis of these vessels can lead to flow-limiting stenosis or distal embolization, which can result in transient ischemic attacks, stroke, upper extremity ischemia, and vertebrobasilar insufficiency. In addition to atherosclerosis, aneurysmal degeneration, dissection, vasculitides (including Takayasu disease and giant cell arteritis), infection, and fibrosis, such as from radiation therapy, can develop in the brachiocephalic arteries. In this chapter, we discuss the open surgical management of brachiocephalic arterial occlusive and/or aneurysmal disease.
Anatomy
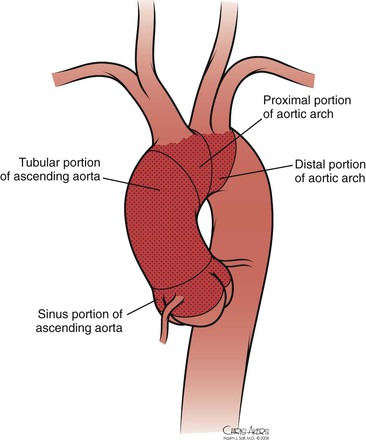
The thoracic aorta develops during the fourth week of gestation, eventually leading to development of the common carotid arteries from the third aortic arch and the brachiocephalic arteries from the third and fourth aortic arches (see Chapter 2). Anatomically, the ascending aorta and transverse arch can be divided into three segments (Fig. 105-1): (1) the aortic root houses the aortic valve, three sinuses, and the two main coronary arteries; (2) the tubular portion of the ascending aorta lies between the supracoronary ascending aorta and the innominate artery; and (3) the transverse arch is located between the innominate artery and the left subclavian artery. The brachiocephalic arteries arise from the dorsal aspect of the transverse arch.
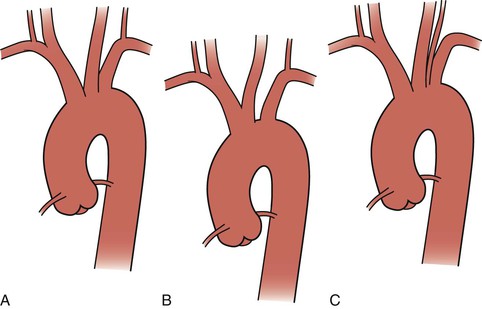
The most common configuration of the arch is three separate trunks, with the innominate artery giving rise to the right subclavian and right common carotid arteries, the left common carotid in close proximity, and the left subclavian artery originating posterior to and to the left of the left common carotid artery. However, a variety of congenital alterations to the aortic arch exist. The true bovine arch is a single, large, common brachiocephalic trunk that comes off the apex of the arch and then separates into the right and left subclavian arteries and a bicarotid trunk. The bicarotid trunk bifurcates into the right and left common carotid arteries. A true bovine arch is much rarer than the commonly named “bovine arch,” in which the left common carotid artery comes off as a branch off the brachiocephalic trunk instead of the aortic arch. Up to 20% of patients may have the so-called bovine arch variation.1 Typically in an aortic origin of the vertebral artery (6%), the left vertebral artery arises between the left common carotid and left subclavian arteries (Fig. 105-2). An aberrant right subclavian artery (0.5%-1%) occurs when the right subclavian artery arises distal to the left subclavian artery (Fig. 105-3).2
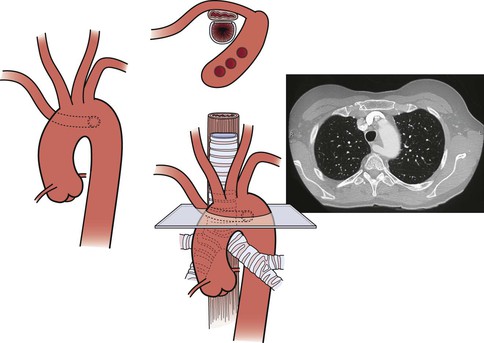
Figure 105-3 Aberrant right subclavian artery with a retroesophageal course. Variations of aberrant subclavian artery include aberrant left subclavian artery in association with a right-sided aortic arch and the association of such aberrant arteries with a diverticulum of Kommerell, which in turn may be aneurysmal (see Chapter 140).
Clinical Findings
The clinical manifestations of lesions involving the brachiocephalic arteries depend on the etiology of the disease, the presence of single-vessel or multivessel disease, and anatomic location. Atherosclerosis is the most common disease affecting the brachiocephalic arteries. Severe disease is defined as stenosis greater than 75% of the vessel’s diameter. Deep ulcerated plaque or thrombus within the arterial lumen is also considered a severe lesion. Atherosclerotic disease can be unifocal, multifocal, single vessel, or multivessel. In the series of 282 transthoracic and transcervical brachiocephalic revascularizations reported by Berguer et al,3,4 there was a 40% incidence of multivessel disease (Fig. 105-4).
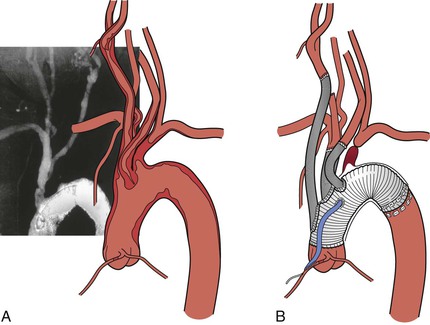
Figure 105-4 A, Severe multivessel atherosclerotic disease with involvement of the ascending and arch aorta. B, Replacement of the ascending and arch aorta with individual brachiocephalic bypasses.
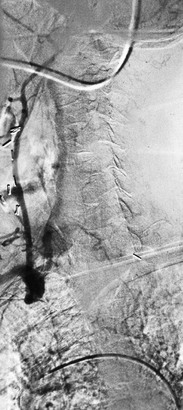
Single-vessel atherosclerotic occlusive disease typically causes symptoms as a result of hemispheric or upper extremity emboli. When the innominate artery is involved, patients may suffer from stroke, transient ischemic attack, and/or upper extremity ischemia. Isolated common carotid disease commonly manifests as stroke or transient ischemic attack. Single-artery occlusion involving the origin of the subclavian artery can cause subclavian-vertebral steal and lead to vertebrobasilar insufficiency, myocardial ischemia (in the case of prior LIMA coronary artery bypass grafting), and hemiparesis or aphasia.5 Reversal of flow in the ipsilateral vertebral artery to provide blood supply to the arm also may result in so-called subclavian steal syndrome, resulting in vertebrobasilar insufficiency. This syndrome is often accompanied by vertigo, nausea, vomiting, imbalance, and diplopia (Fig. 105-5) (see Chapter 97). In patients who have previously undergone coronary artery bypass with the internal mammary artery, angina may recur because of flow reversal in the bypass, which can lead to myocardial ischemia (subclavian-coronary steal).6 Occlusion of the innominate artery can manifest as subclavian-carotid steal, with reversal of flow in the ipsilateral carotid artery causing anterior cerebral symptoms, such as aphasia and hemiparesis.7 Multiple-vessel disease usually results in vertebrobasilar insufficiency, secondary to a low-flow state.8–10
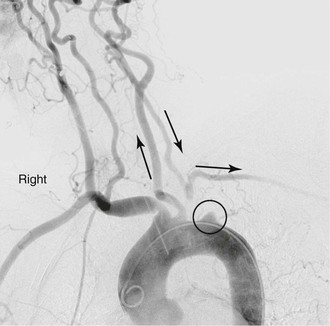
Figure 105-5 Subclavian steal in a patient with an occluded proximal left subclavian artery. Late filling of subclavian artery via retrograde flow in left vertebral artery.
Overall, symptomatic disease from stenosis of the brachiocephalic artery is uncommon because of the numerous collateral vessels present and the relatively low incidence of atherosclerotic disease affecting the upper extremity. Pain and fatigue from repeated use of the upper extremity can be a sign of subclavian or brachiocephalic artery compromise. In more severe cases, rest pain may be present, eventually leading to digital gangrene. Some patients may also present with findings consistent with Raynaud’s syndrome.11 In addition, stenotic and/or ulcerative lesions can be a source of microembolic phenomena to either the brain or hand.
Infectious processes (including syphilis and tuberculosis) can lead to aneurysmal degeneration of the brachiocephalic arteries (Fig. 105-6) and, in particular, the subclavian artery.12 These are rare causes of proximal (intrathoracic) aneurysm. Blunt traumatic injuries can also lead to proximal aneurysm formation, usually involving the origin of the innominate artery.13 Penetrating trauma may affect the brachiocephalic vessels in any location (Fig. 105-7) (see Chapters 156 and 157). Distal (extrathoracic) subclavian artery aneurysms are commonly related to a cervical rib, causing arterial thoracic outlet syndrome (Fig. 105-8) (see Chapter 124). The pathogenesis of the aneurysm is thought to be related to repetitive trauma to the artery at the level of the thoracic outlet.14,15 The clinical consequences of aneurysmal degeneration are usually related to the distal embolisms causing arm claudication, pain at rest, and digital ulcerations. Compressive symptoms, involving the recurrent laryngeal nerve (hoarseness), brachial plexus (upper extremity weakness, pain) and rupture can also occur.16 The more proximal aneurysms affecting the ascending aorta and arch are commonly dealt with by cardiothoracic surgeons and involve cardiopulmonary bypass.

Figure 105-6 A, CT scan of a syphilitic aneurysm. B, CT scan of a syphilitic aneurysm with left carotid artery occlusion.
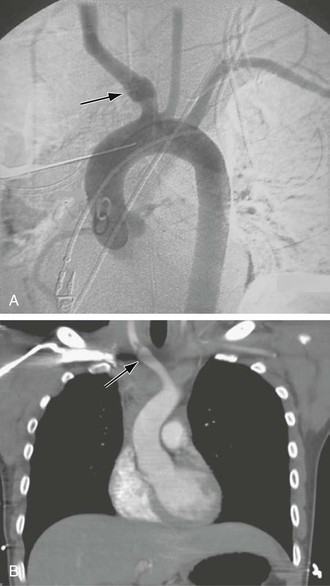
Figure 105-7 A, Aortogram demonstrating blunt traumatic injury (arrow) to the innominate artery. B, CT scan demonstrating an intimal flap in the innominate artery after blunt traumatic injury (arrow).
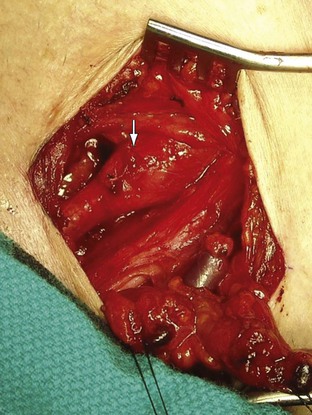
Figure 105-8 Distal right subclavian artery aneurysm in a patient with arterial thoracic outlet syndrome exposed via an infraclavicular incision. The patient’s head is at the top, left corner, and feet to the bottom, right corner.
Takayasu’s disease frequently involves all the proximal portion of the aortic arch branches (Fig. 105-9) (see Chapter 80). The disease is characterized by an acute inflammatory phase and a “burned-out” sclerotic phase. The inflammatory process leads to fibrosis and thickening of the arterial wall, whereas sclerosis leads to stenosis. Symptoms are typically related to vertebrobasilar insufficiency once the disease has progressed to multivessel occlusion. Chronic disease can also manifest as aneurysmal degeneration with embolic potential.17
Diagnostic Evaluation
In addition to a comprehensive physical examination, careful assessment of the upper extremity pulses, bilateral upper extremity blood pressure measurements, and auscultation of the carotid and subclavian arteries for bruit are effective tools for the diagnosis of brachiocephalic vascular disease. Duplex ultrasound examination of the aortic arch may be of some utility in identifying flow reversal in the vertebral arteries and excluding significant disease in the extracranial carotid arteries (see Chapter 98).18,19
Noninvasive imaging modalities, such as magnetic resonance imaging (MRI) and computed tomography (CT) scan, provide excellent imaging of the aorta and great vessels (see Chapter 93). Body habitus, claustrophobia, and metallic implants may limit the use of these imaging techniques. CT or MRI of the brain should also be performed before any planned revascularization to identify lesions susceptible to bleeding or areas of prior stroke, as reperfusion injury may develop in recent areas of stroke as a result of a transient ischemic state during surgery.20
The “gold standard” imaging modality is aortography. However, disadvantages of this invasive study include iatrogenic arterial injury, risk of stroke, and nephrotoxicity from iodinated contrast material. Because the incidence of concomitant coronary atherosclerosis approaches 40%, cardiac evaluation should also be performed, especially if transthoracic revascularization is planned.21 We routinely obtain a transthoracic echocardiogram and 12-lead electrocardiogram. Patients with a low ejection fraction (<50%) or ischemic electrocardiographic changes are referred for additional evaluation with a stress test or coronary angiography.22
Transesophageal echocardiography (TEE) is another important diagnostic tool because of its ability to accurately identify atherosclerotic disease in the proximal ascending and descending portions of the thoracic aorta.23 Disadvantages of TEE are that accurate evaluation requires an experienced sonographer and that the patient usually needs conscious sedation during the procedure. If transthoracic revascularization is planned, the proximal ascending aorta should be devoid of any atheromatous plaque or dissection. If accurate preoperative or intraoperative TEE is not available, a hand-held ultrasound probe (epiaortic ultrasound) can be used intraoperatively, once the aorta is exposed, to rule out atheromatous plaque in the ascending aorta.24
Revascularization
Indications
General indications for brachiocephalic revascularization include stroke or transient ischemic attacks due to atheroembolism; low-flow states, leading to vertebrobasilar insufficiency or, less commonly, cortical symptoms; and steal syndrome from proximal innominate or subclavian artery occlusion, leading to vertebrobasilar insufficiency, myocardial ischemia after internal mammary artery bypass or anterior cerebral TIA, or stroke. Upper extremity pain with exertion and/or digital ischemia is a common indication for intervention.25,26 A significant number of patients with proximal subclavian stenosis may demonstrate reversal of flow in the vertebral artery without displaying symptoms of vertebrobasilar insufficiency. Such patients can be safely observed until symptoms develop.27 There are few natural history data to guide decision making for patients with asymptomatic brachiocephalic disease. Some authorities suggest that asymptomatic patients with severe (>75%) stenosis of the innominate or common carotid artery should undergo revascularization if they have reasonable surgical risk,27a but this is controversial and data are inadequate for resolution. There is agreement, however, that revascularization of severe (>75%) asymptomatic stenosis of the subclavian artery should be performed if coronary artery bypass with the ipsilateral internal mammary artery is planned.27b
Options for Revascularization
Anatomic (transthoracic) revascularization is preferred for patients with multivessel disease and low surgical risk. Proximal innominate and subclavian aneurysms and traumatic injuries are also best treated with a bypass from the ascending aorta to the involved brachiocephalic arteries (Fig. 105-10).
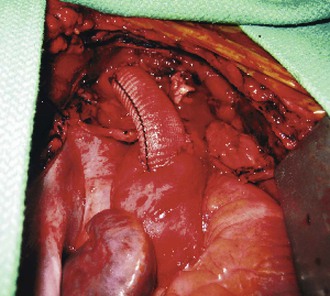
Figure 105-10 Completed aorto-innominate bypass in a patient (see also Fig. 105-7) with blunt traumatic injury to the proximal innominate artery.
Extraanatomic cervical revascularization is ideal for single-vessel subclavian disease or in patients for whom median sternotomy presents prohibitive risk. This approach is often combined with endovascular treatment of thoracic aortic aneurysms. Transposition of the left subclavian artery or carotid-subclavian bypass can extend the proximal “landing zone” to the left carotid artery. A right-to-left carotid bypass can further extend the proximal landing zone to the level of the innominate artery (see Chapters 136 and 137).
Anatomic Revascularization
The ascending aorta and transverse aortic arch are approached through a median sternotomy. The procedure is initiated with a skin incision from just below the sternal notch to the xiphoid process. Electrocautery is used to divide the soft tissues down to the sternum. A sternal saw is then used to divide the sternum from superior to inferior, and a sternal retractor to gently free the mediastinal structures from the undersurface of the sternum. Incision of the pericardium exposes the heart, aorta, innominate vein, and brachiocephalic arteries. Anatomic revascularization of the brachiocephalic arteries can be accomplished by either endarterectomy or bypass.
Endarterectomy
Endarterectomy is an effective strategy for focal lesions involving the midsection of the proximal innominate or common carotid artery. When the atherosclerotic lesion is located at the orifice of the brachiocephalic trunk, the transverse arch is usually involved in this process. However, in this setting, endarterectomy can be fraught with the dangers of embolization, incomplete endarterectomy, and aortic dissection. Also, endarterectomy is unsuitable for patients with disease involving a bovine arch variant (left common carotid artery arising from the innominate artery) because clamping of the innominate artery would cause ischemia in both cerebral hemispheres.
Bypass Grafts
Bypasses can be constructed from the ascending aorta to the brachiocephalic arteries if the ascending aorta is free of atherosclerotic disease (Fig. 105-11). The presence of atheroma can be confirmed by intraoperative TEE or epiaortic ultrasound.23 The patient undergoes heparinization with 1 mg/kg (body weight) (90 units/kg) of intravenous heparin. A partial-occlusion clamp is applied after heparinization (see Fig. 105-11) and a 12- to 14-mm woven Dacron tube graft impregnated with collagen or gelatin is sewn to the ascending aorta in end-to-side fashion with 4-0 polypropylene suture. The partial-occlusion clamp is released with the patient in the Trendelenburg position, and a clamp is placed distally on the graft. The innominate artery is then transected distal to the diseased portion and the proximal stump is oversewn with 4-0 polypropylene suture. The distal anastomosis is completed in an end-to-end fashion with 4-0 or 5-0 polypropylene suture.
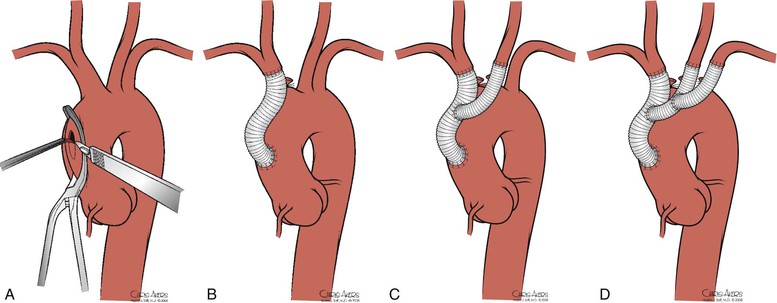
Figure 105-11 A, Partial-occlusion clamp placed on the ascending aorta with creation of a punch arteriotomy. B, Creation of an aorto-innominate bypass. C, Sidearm graft to the left carotid artery. D, Sidearm graft to the left subclavian artery.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree