Brachiocephalic or subclavian artery obstruction accounts for about 15% of symptomatic, extracranial, cerebrovascular disease. Rapid advances in technology and evolution in technique over the last decade have resulted in percutaneous revascularization techniques supplanting surgery as the therapy of choice for the treatment of these lesions. Owing to the predilection of atherosclerosis for these sites, and the relative sparing of more distal upper extremity vessels, brachiocephalic and subclavian artery intervention comprise the majority of upper extremity endovascular procedures and will form the major focus of this chapter. Additional, less common vascular pathologies encountered during angiography of the upper extremity arterial circulation will also be highlighted.
ANATOMY
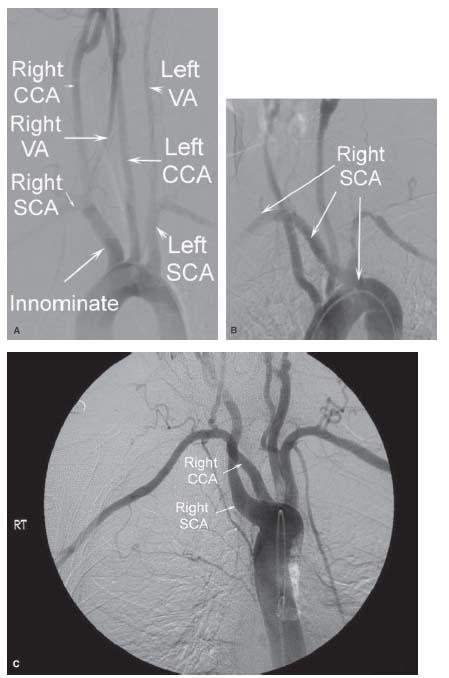
The subclavian arteries originate from the bifurcation of the brachiocephalic artery on the right, and directly from the aortic arch as the third, and final, of the great vessels on the left (Fig. 24.1A).
In approximately 0.5% of patients, the right subclavian artery arises anomalously, as the terminal vessel from the descending thoracic aorta, and courses toward its normal distribution to the right upper extremity (Fig. 24.1B).
Rarely, the right subclavian artery and right common carotid arteries have a separate origin as the first and second of the great vessels, respectively, from the arch (Fig. 24.1C).
Additional variations in arch anatomy that are important during upper extremity angiography include common origin of the innominate and left common carotid artery (CCA) from the arch (about 15%) (Fig. 24.1D), and bovine origin of the left CCA from the innominate artery (about 10%) (Fig. 24.1E).
In healthy young individuals, the great vessels arise from the horizontal portion of the arch. With increasing age and atherosclerotic disease, this portion of the arch descends into the thoracic cavity together with the origin of the great vessels, such that they appear to arise from the ascending portion of the arch (Fig. 24.1F,G).
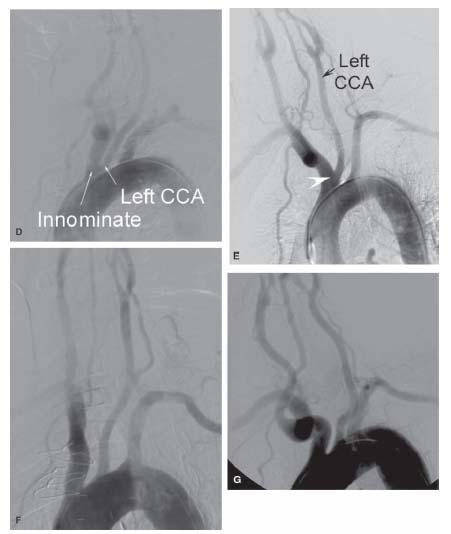
The most important branches of the subclavian artery arise from the first segment of the artery (i.e., medial to the scalenus anterior muscle) (Fig. 24.2A). The vertebral and internal mammary artery branches of the subclavian artery are remarkably constant in their origin and course, arising as the first and second branches, respectively. These branches supply the posterior cerebral circulation and the anterior chest wall, respectively. In 1% to 5% of patients, the left vertebral artery had a direct origin from the aortic arch, typically between the origins of the left CCA and the left subclavian artery (Fig. 24.2B).
In contrast, the thyrocervical trunk, which arises as the third branch, demonstrates significant variation in both the pattern and size of its various branches (i.e., inferior thyroid, suprascapular, ascending cervical, transverse cervical).
At the lateral margin of the first rib, the subclavian artery becomes the axillary artery. At the anatomic neck of the humerus, the axillary artery changes name to become the brachial artery (Fig. 24.2C).
In the arm, the brachial artery supplies the deep brachial branch that runs posteriorly (and is relatively small in caliber compared with its counterpart in the thigh), and the superior and inferior ulnar collateral arteries that supply collateral flow to the elbow region. Opposite the neck of the radius, the brachial artery typically divides into the radial and ulnar arteries (Fig. 24.2D).
The ulnar artery is usually the larger of the terminal branches of the brachial artery. Just distal to its origin, it gives off the anterior and posterior ulnar recurrent arteries that supply collateral flow to the elbow, and then gives off its major branch, the common interosseous. Thereafter, the ulnar artery descends on the medial side of the forearm. The radial artery supplies a radial recurrent branch to the elbow, and descends on the lateral side of the forearm. In some cases, the radial artery may originate high from the axillary or upper brachial artery. This is an important anatomic variant, as it may cause significant confusion during diagnostic angiography if its presence is not appreciated.
The arterial anatomy of the hand is extremely variable, and deviations from the classic patterns are common (Fig. 24.2E,F).
The ulnar artery supplies the superficial palmar arch and the radial artery supplies the deep palmar arch. In 10% of the population, the anterior interosseous or median artery persists and supplies the deep palmar arch. Typically, the superficial arch is dominant and lies distal to the deep arch. The princeps pollicis and radialis indicis arteries arise from the radial artery and supply the thumb and index finger. The superficial palmar arch gives off three or four common palmar digital arteries, and the deep arch gives off the palmar metacarpal arteries. At the bases of the proximal phalanges, adjacent metacarpal vessels from each arch join and then immediately divide into proper digital arteries, which supply the fingers (1,2).
Figure 24.1 • Normal and variant anatomy of the aortic arch. A: Arch aortogram in LAO projection demonstrating normal angiographic anatomy. B: Anomalous origin of right SCA as terminal great vessel off aortic arch. C: Separate origin of right SCA and CCA from aortic arch demonstrated in aortogram in RAO projection. D: Common origin of innominate and left CCA from aortic arch. E: Bovine origin of left CCA from innominate artery (arrowhead). F: Type II aortic arch. G: Type III aortic arch. CCA, common carotid artery; VA, vertebral artery; SCA, subclavian artery.
BRACHIOCEPHALIC AND SUBCLAVIAN ARTERY INTERVENTION
Patient Selection
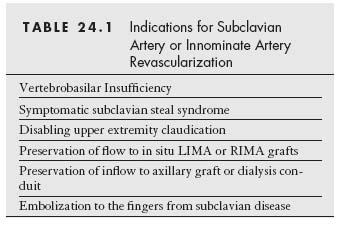
As in all endovascular procedures, careful patient selection is absolutely crucial to the success of the intervention (Table 24.1).
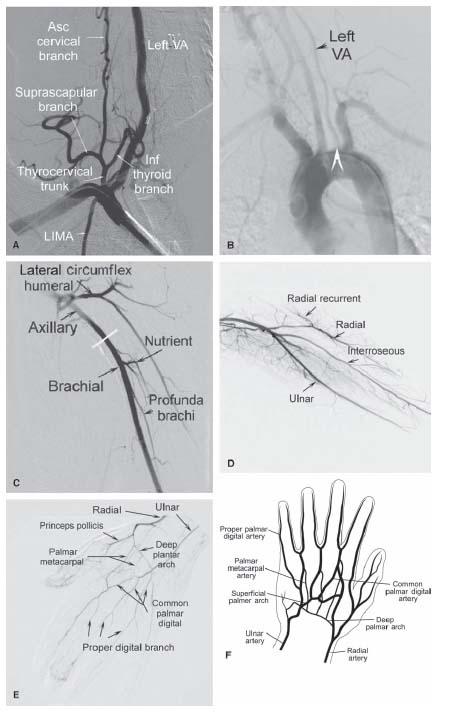
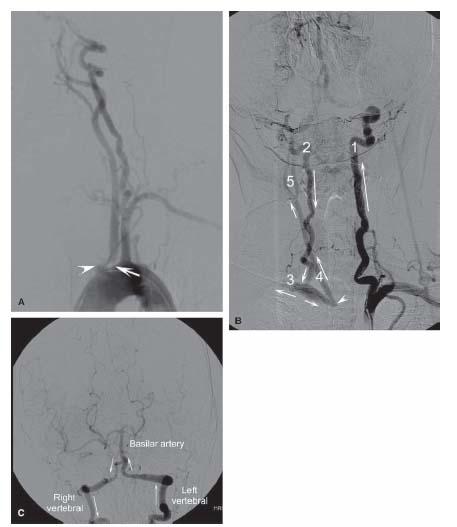
With some exceptions, intervention is generally reserved for patients with symptomatic subclavian or brachiocephalic disease. It is worth emphasizing that most patients with angiographic evidence of subclavian or brachiocephalic artery stenosis are asymptomatic. When symptoms are present, they may be attributable to ischemia of the upper extremity muscle groups that is precipitated by upper extremity activity. Alternatively, symptoms may be attributable to “steal” of blood flow from the posterior cerebral circulation toward the upper extremity, via retrograde flow along the ipsilateral vertebral artery, caused by significant proximal brachiocephalic/subclavian stenosis or obstruction (Fig. 24.3) (3,4). When symptomatic (i.e., subclavian steal syndrome), patients present with symptoms of posterior circulation ischemia including dizziness, diplopia, nystagmus, ataxia, and visual symptoms associated with upper extremity activity. Again, it is worth emphasizing that the presence of retrograde flow along the vertebral artery is most commonly asymptomatic, and is referred to as the “subclavian steal phenomenon.”
Figure 24.2 • Angiographic anatomy of upper extremity. A: Angiography of right subclavian artery demonstrating origin and course of the major branches from the first segment of the vessel. B: Arch aortogram demonstrating anomalous origin of left vertebral artery from typical location on aortic arch (arrowhead). C: Angiography of left axillary and brachial artery. D: Angiography of distal left brachial artery and ulnar and radial branches. E: Angiography of right hand of a patient with small-vessel vasculitis involving the proper digital branches. F: Schematic illustration of typical arterial anatomy in the hand. VA, vertebral artery; Inf, inferior; Asc, ascending; LIMA, left internal mammary artery.
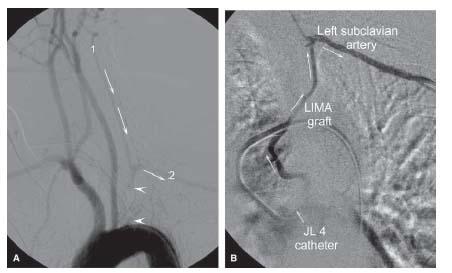
In patients with prior bypass surgery involving “in situ” right internal mammary artery (RIMA) or left internal mammary artery (LIMA) grafts, coronary “steal” may also occur as a result of retrograde flow along the graft from the coronary circulation toward the distal subclavian artery, precipitating coronary ischemia (Fig. 24.4) (5).
Typically, these “steal” syndromes are worsened by upper extremity activity. Specific to brachiocephalic artery lesions, ischemia in the distribution of the right internal carotid artery (ICA) may be the presenting symptom, on the basis of atherothrombotic embolization from the lesion, or hemodynamic compromise of flow. In asymptomatic patients, subclavian or brachiocephalic artery intervention may be performed to protect the inflow to a variety of surgical grafts including axilloaxillary, axillofemoral, subclavian–carotid, and IMA–coronary.
The dominant contraindication to subclavian/brachiocephalic percutaneous intervention is the presence of fresh thrombus. Embolization to the vertebral artery or right ICA during subclavian and brachiocephalic artery intervention is an important complication in this circumstance. There are significant technical challenges to the use of embolic protection devices (EPDs) for these procedures that further add to the risk in this setting. Therefore, with thrombotic lesions, the authors recommend either thrombolysis, or 2 to 4 weeks of anticoagulation, prior to proceeding with intervention. If the lesion must be dealt with immediately, use of a glycoprotein IIb/IIIa inhibitor, in addition to the use of embolic protection devices, is recommended.
Upper Extremity Angiography
AORTOGRAM
The major indications for upper extremity angiography are listed in Table 24.2
Prior to selective angiography of the upper extremity, it is prudent to always perform an arch aortogram (40° LAO projection). Our practice is to use a multisidehole pigtail catheter (Fig. 24.5A) for this purpose.
The arch aortogram facilitates the detection of important anomalies, as outlined earlier, and anatomic features (e.g., tortuosity of brachiocephalic or proximal subclavian artery, type III aortic arch) that influence the choice of equipment used to perform angiography and intervention, and increase the technical complexity of these procedures. An RAO view is rarely helpful, except in circumstances where there is significant overlap of vessels in the LAO view. Ideally, rotational angiography would be the gold standard, allowing a complete 3D assessment of the arch and the origins of the great vessels.
When selective angiography of the entire upper extremity is required, it is advisable to adopt a systematic, stepwise approach, starting proximally and working distally. This approach facilitates the prompt detection of anomalies, such as the high origin of either the radial or ulnar artery from the brachial artery, or the origin of the radial artery from the axillary artery. Failure to adopt this approach may result in an erroneous diagnosis of vessel occlusion. Iodixanol, an iso–osmolar nonionic contrast agent, is the preferred contrast medium for use in upper extremity angiography because of its excellent tolerability. By using hand injections of 5 to 10 mL of contrast agent with digital subtraction angiography (DSA), adequate visualization of all major vessels is achieved (2,6).
SUBCLAVIAN AND BRACHIOCEPHALIC ARTERY ANGIOGRAPHY
Selective engagement of the brachiocephalic artery and left subclavian artery may generally be achieved using a JR4 diagnostic of Berenstein catheter (Fig. 24.5B). For patients with unfolding of the aortic arch (i.e., type III arches), alternative catheters may be required (e.g., Vitek, Simmons, Headhunter-1) (Fig. 24.5C-E). The appropriate use of these catheters is important. In the case of the Vitek catheter, the practice is to advance the catheter to the descending thoracic aorta, where advancement of the catheter will usually allow the catheter to form its preformed shape. Further advancing the catheter over the arch will usually result in the tip of the catheter engaging the origin of the great vessels sequentially.
Safe removal of the Vitek catheter is accomplished by advancing the catheter into the ascending aorta, passing a long wire through the catheter beyond the tip to straighten the curve, and then removing the catheter and wire in unison. This technique minimizes trauma to the arch from the catheter tip. Owing to the larger primary curve of the Simmons catheter, it is more challenging to use because of the difficulty in reshaping the catheter in the aortic arch. The author’s preferred method for reshaping a Simmons catheter is to use a diagnostic catheter to engage the left subclavian artery and advance an exchange length wire (i.e., 260–300 cm) into the left subclavian artery. The diagnostic catheter is removed and the Simmons catheter is advanced over the wire and its tip is positioned in the proximal segment of the left subclavian artery. The wire is then withdrawn close to the tip of the catheter and the Simmons catheter is advanced forward resulting in prolapse of the catheter into the arch assuming its preformed shape. A similar removal technique for the Simmons catheter is employed, as described, for the Vitek catheter.
Following selective engagement of the left subclavian artery and brachiocephalic artery, angiography is performed in orthogonal oblique projections. The bifurcation of the brachiocephalic artery and origin of the right subclavian artery is well delineated in the RAO projection. The origins of the right vertebral artery and RIMA are usually best visualized in the LAO projection. For the left subclavian artery, the origins of the left vertebral artery and LIMA are usually best visualized in the RAO projection. Subclavian artery angiography is performed with the patient’s arm adducted at the patient’s side (i.e., neutral position). In the specific circumstance when thoracic-outlet syndrome causing arterial compression is suspected, angiography is performed in the posteroanterior (PA) projection with the arm in neutral position, and repeated with the shoulder in full abduction, external rotation, and retroversion (i.e., the throwing position).
Figure 24.3 • Demonstration of subclavian artery steal from vertebrobasilar circulation in a patient with innominate artery occlusion. A: Arch aortogram demonstrating innominate artery occlusion (arrowhead) and ostial left common carotid artery (CCA) stenosis (arrow). B: Left subclavian artery angiography demonstrating antegrade flow along left vertebral artery (1), and retrograde flow along right vertebral artery (2), toward the right subclavian artery (3), and right CCA (4). Arrows indicate the direction of flow. (5) Right CCA bifurcation. C: Selective angiography of left vertebral artery showing that flow from the left to right vertebral artery occurs at the level of the vertebrobasilar junction. Arrows indicate the direction of flow.
AXILLARY AND BRACHIAL ARTERY ANGIOGRAPHY
Selective angiography of the axillary or brachial arteries requires delivery of the diagnostic catheter into the distal subclavian artery, beyond the brachiocephalic/left subclavian artery ostium. Following the initial engagement of the respective ostia with the diagnostic catheter, a long (i.e., 300 cm) soft-tipped, 0.035″ wire (e.g., Wholey/Magic Torque®) is advanced into the brachial artery, using the DSA road-mapping function, and then the diagnostic catheter is advanced over this wire. This is a straightforward maneuver when the diagnostic catheter is a JR4, Berenstein, or angled glide catheter. When a Vitek or Simmons catheter is required to engage the respective ostia, an alternative strategy is usually required. In this circumstance, a soft-tipped wire, or stiff-angled glide wire, is advanced into the brachial artery, and the Vitek or Simmons catheter is then exchanged for a “friendly” diagnostic catheter (e.g., angled glide catheter or multipurpose catheter) (Fig. 24.5F,G). The angled glide wire is very steerable but care is required so as not to cause vessel dissection. Additionally, catheter exchanges over this wire are difficult and must be performed with great care so as not to loose wire position. Axillary artery angiography is performed with the arm in the neutral position or slightly abducted, whereas brachial artery angiography is performed with the arm abducted, and the forearm placed supine on an arm board.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree