Blunt and Penetrating Injuries of the Chest Wall, Pleura, and Lungs
Julian Guitron
Lynn C. Huffman
John A. Howington
Joseph LoCicero III
A systematic primary and secondary survey, as adopted from the Advanced Trauma Life Support (ATLS) guidelines by the American College of Surgeons,1 allows prioritization of injuries and prompt treatment to be instituted. It is imperative to keep these general trauma guidelines in perspective in approaching patients with thoracic injuries. Most commonly, the thoracic surgeon will be consulted by the trauma surgeon to address specific chest injuries. Even by an expert specialist, the general condition of the patient must be considered first, particularly in the face of obvious thoracic trauma that can easily distract from the well-established and lifesaving ATLS algorithms.
Incidence
Trauma kills 150,000 Americans every year. It is the most common cause of death in the population <40 years of age. One-fourth of deaths are specifically related to chest trauma,65 many of them occurring in the prehospital setting.93
The reported survival in adults after cardiopulmonary resuscitation (CPR) in the trauma center ranges from 0% to 23%, as recorded by several authors.9,69,80,99 The survival range in the pediatric population is similarly varied from 1.5% to 25%.16,64,101 It is important to note, however, that there is great disparity in the selection of patients as well as in the actual situations surrounding the CPR events. Under any circumstances, the survival following CPR on “dead” patients is dismal. This led to the publication, in 2003, of specific guidelines regarding the withholding or termination of CPR in traumatic cardiac arrests in the prehospital setting.51 In that latter report, it was suggested that such resuscitative efforts are no longer required or even indicated in adults ≥18 years of age who are victims of blunt trauma and are apneic and pulseless when the emergency medical services (EMS) arrive on the scene. Further evidence supporting such recommendations were made at Tulane University in 2004 by Stockinger and colleagues, who reviewed >16,000 trauma patients over 6 years. They found only 0.9% survivability in penetrating CPR and 6.2% in blunt trauma CPR.98 The final decision to stop CPR remains the prerogative of the physician in charge at the trauma center based on the information supplied by the EMS.
Disposition of patients who deteriorate en route and are “dead on arrival” (DOA) has been clarified. Demetriades and colleagues28 from the University of Southern California reported their experience from 1993 to 2002 involving a total of 34,120 trauma patients over 9 years. In their overall series, 65% sustained blunt trauma, while 35% had penetrating trauma. Their overall in-hospital mortality was 7.8%. Of these deaths, 3.7% resulted from blunt trauma and 4% from penetrating trauma. The most common body areas with critical injuries were the head (43%), chest (28%), and abdomen (19%). Table 73-1 shows the results in patients considered DOA.
The American College of Surgeons (ACS) recently presented the latest version of the National Trauma Data Bank (NTDB), which included 1,485,098 trauma records, the largest trauma
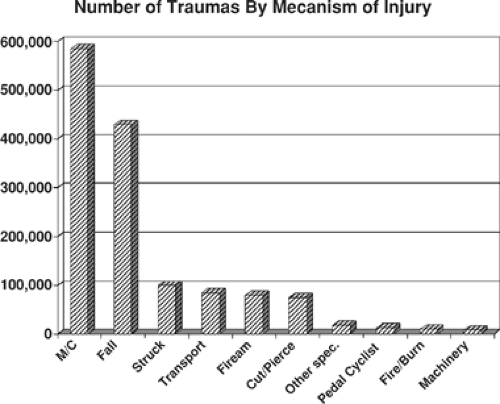
database to date.125 Version 7.0 of the NTDB used a rolling 5-year time frame for the yearly analysis, ensuring the latest high-quality information from 712 participating hospitals nationwide. Figure 73-1 shows the trauma distribution by age and Figure 73-2 by mechanism, further enhancing our understanding of the trauma situation in our population and allowing a more effective focus on improving prevention strategies.
database to date.125 Version 7.0 of the NTDB used a rolling 5-year time frame for the yearly analysis, ensuring the latest high-quality information from 712 participating hospitals nationwide. Figure 73-1 shows the trauma distribution by age and Figure 73-2 by mechanism, further enhancing our understanding of the trauma situation in our population and allowing a more effective focus on improving prevention strategies.
Table 73-1 USC Trauma Experience in 34,120 Trauma Patients Over 9 Yearsa | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||
Even though many patients presenting with thoracic injuries sustain multiple types and levels of injuries, the following text discusses each type separately for better understanding of its pathophysiology and optimal management.
Initial Evaluation
It is imperative to identify and correct life-threatening injuries immediately upon encountering the patient. The primary survey, as described by the Advanced Trauma Life Support (ATLS) course, ensures proper assessment and stabilization of the airway, breathing, and circulation. During the first few minutes of the patient’s arrival to the trauma bay, the possibility of endotracheal intubation, needle decompressions, and pericardioscentesis must be considered, occasionally without the luxury of radiographic evaluations in the most critical circumstances. The secondary survey will meticulously record every injury from head to toe in a systematic manner. Significant physical examination findings are shown in Table 73-2. Special attention should be directed to the neck veins, the motion of the chest wall, palpation, chest percussion, and breath sounds.
Imaging modalities have become an integral part of the trauma evaluation. Chest radiography is the most common initial study, usually obtained while the trauma team completes the physical evaluation. Bedside ultrasonography now is routine. It aids in the diagnosis of pericardial effusion, pneumothorax, and intra-abdominal fluid. In most instances it replaces the diagnostic peritoneal lavage. Computed tomography (CT) allows more detailed assessment of injuries. Advancement of technology is spawning new investigational algorithms that include fast, multislice CT scanners that could potentially incorporate bedside tomography to the secondary survey.48 Magnetic resonance imaging (MRI) may further characterize injuries, particularly in the brain and spine. However, since the patient is inaccessible during the study, it is recommended only when the patient is hemodynamically stable.
Specific Injuries
Traumatic Asphyxia
Traumatic asphyxia results from severe blunt thoracic trauma. The manifestation is excessive venous pressures. Characteristic signs include facial and upper chest petechiae, subconjunctival
hemorrhages, cervical cyanosis, and temporary loss of vision due to retinal edema. Thoracoabdominal compression during deep inspiration against a closed glottis causes venous hypertension in the valveless cervicofacial system, which results in the myriad of striking findings. Among survivors, traumatic asphyxia is self-limited. Supportive treatment is recommended.63,101
hemorrhages, cervical cyanosis, and temporary loss of vision due to retinal edema. Thoracoabdominal compression during deep inspiration against a closed glottis causes venous hypertension in the valveless cervicofacial system, which results in the myriad of striking findings. Among survivors, traumatic asphyxia is self-limited. Supportive treatment is recommended.63,101
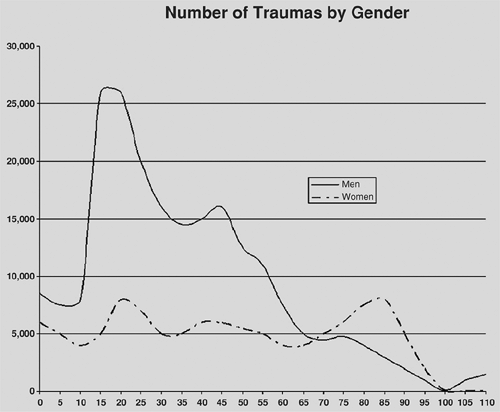 Figure 73-1. Trauma distribution by age from 2002 to 2006. (From the National Trauma Data Bank (NTDB). With permission.) |
Mediastinal and Subcutaneous Emphysema
Injuries to the upper airway, tracheobronchial tree, esophagus, or lung parenchyma can lead to mediastinal and subcutaneous emphysema. Physical exam, chest radiography, or CT usually demonstrates these injuries. Typically, the more distal the injury, the more likely it is to cause decompensation. The severity of the emphysema is directly related to the severity of the trauma. Air dissects along the bronchi and pulmonary vessels into the mediastinum and may migrate into the subcutaneous space of the neck and face, sometimes reaching from the torso down to the inguinal ligament and external genitalia.8
Table 73-2 Specific Physical Findings in Chest Trauma | |
|---|---|
|
Goudy and colleagues40 reported their experience at the University of Louisville. Cervical emphysema without pulmonary injuries was related to motor vehicle crash (43%), gunshot wound (37%), assault (10%), blunt injury (5%), and penetrating injury (5%). The source of the emphysema was glottic injury in 37%, hypopharyngeal injury in 27%, oropharyngeal injury in 16%, esophageal injury in 5%, and undetermined in 15%. Judicious use of bronchoscopy and esophagoscopy is recommended should there be any sign of worsening by clinical or radiographic criteria. Decompression incisions in the skin are rarely if ever indicated.
Rib Fractures
Rib fractures are the most common major thoracic injuries. Up to 40% of all thoracic trauma patients present with rib fractures.24,56 In cases of isolated rib fractures, the diagnosis is primarily clinical. The most prominent symptom is exquisite focal pain exacerbated by deep breathing. Palpation may produce tenderness or crepitus of the rib fragments. In multiple trauma patients, the diagnosis is often made radiographically. Simple fractures should alert the surgeon to the potential of underlying injury to the lung and other intrathoracic structures. Bone scans may be helpful to detect occult fractures in athletes.42
Fractures of One or Two Ribs Unilaterally
Management of one or a few rib fractures is directed at pain control to facilitate adequate pulmonary hygiene and identifying associated injuries. Uncontrolled pain may result in chest wall
splinting and chronic hypoventilation. Adequate pain control is mandatory to allow early mobilization, deep inspiratory efforts, and coughing in order to avoid secondary complications. Pulmonary physiotherapy, nasotracheal suctioning, and prompt bronchoscopy should be instituted in patients unable to clear secretions.
splinting and chronic hypoventilation. Adequate pain control is mandatory to allow early mobilization, deep inspiratory efforts, and coughing in order to avoid secondary complications. Pulmonary physiotherapy, nasotracheal suctioning, and prompt bronchoscopy should be instituted in patients unable to clear secretions.
Alternative methods for controlling pain due to thoracic injury include epidural analgesia, intercostal nerve blocks, intrapleural catheter analgesia, and transcutaneous electrical nerve stimulation. Each of these modalities has disadvantages.8 Epidural analgesia has been shown to improve outcomes compared with parenteral narcotics, particularly in the elderly population.120 However, hypotension may occur. Also, hospital policies or guidelines may limit the patient’s mobilization because of the need for monitoring. Intercostal nerve blocks require repeated administration with the risk for pneumo- thorax on each injection. Intrapleural regional analgesia with a catheter obviates the need for sedation or respiratory depression. However, catheter placement carries a risk for pneumothorax and may be less effective than epidural analgesia.66 Transcutaneous electrical nerve stimulation is of no benefit immediately after trauma. This method should be limited to controlling pain in a chronic setting. Catheters that can be placed in the subcutaneous space with a constant infusion of anesthetic, as with the On-Q device (I-Flow Corporation, Lake Forest, CA), may be beneficial, but no studies are available at this time.
Fractures of the First and Second Ribs
The main priority for first- or second-rib fractures should be to evaluate for associated intrathoracic injuries. Fractures of the upper ribs (including the scapula) are associated with a 36% mortality rate.86 Associated injuries include brain in 53%, intra-abdominal organs in 33%, and other thoracic structures in 64% of the patients. Some surgeons have suggested routine aortography on any patient with such fractures. Others recommend reserving this invasive investigation to cases with additional evidence of aortic or great vessel injuries.82 CT angiography likely will replace aortography as the scanners become more precise.
Multiple or Bilateral Rib Fractures
Factors that have the most impact on outcome after rib fractures include the number of ribs fractured, age of the patient, and underlying pulmonary status.37,119 There is considerable evidence supporting the use of continuous epidural analgesia in severe chest wall injuries to improve outcome.67,120,124 One should always keep in mind that mortality from isolated rib fractures can be as high as 5% in children and 20% in the elderly population. Once pain is under control, a transition to transdermal analgesia supplemented by oral analgesics and anti-inflammatory agents may be possible.
Flail Chest
Instability of the chest wall results from unilateral or bilateral multiple rib fractures and/or disruption of costochondral junctions. The force needed to create a flail segment depends on the compliance of the ribs (i.e. elderly persons may need only a low-energy impact, whereas less than 1% of children develop flail chest even after severe thoracic trauma).76 LoCicero and Mattox65 determined the incidence of flail chest in patients with thoracic injuries to be as high as 5%.
Because of underlying pulmonary contusion, the clinical appearance of patients with flail chest may be misleading. This associated pulmonary injury may cause a decrease in oxygen diffusion to a variable portion of the ipsilateral lung. The traumatic chest wall segment floating unattached to any bony structure results in paradoxical chest wall motion. This leads to a reduction in vital capacity and to ineffective ventilation, which, along with the associated pulmonary contusion, may lead to the development of acute respiratory distress syndrome (ARDS).
Current treatment recommendations stress the importance of prophylaxis and early intervention.8,22,35 These interventions include pain control, humidification of air, aggressive pulmonary physiotherapy with incentive spirometry, deep breathing and coughing several times each hour, deep suctioning in patients unable to clear secretions, and judicious use of bronchoscopy to remove any retained secretions promptly. Early documentation of respiratory compromise by frequent monitoring of respiratory rate, oxygen saturation, and arterial blood gases (ABG) is crucial. Therapy is then guided by blood gas results. Unless there is evidence of rapid improvement after a short period of observation, pain management, and aggressive pulmonary therapy, noninvasive ventilation or endotracheal intubation and ventilator assistance is indicated. Suggested parameters for instituting ventilatory support are respiratory rate >30 breaths per minute, PaO2<60 mm Hg, or PaCO2>45 mm Hg.
Treatment of the unstable chest wall has been controversial, shifting from stabilization of the flail segment to aggressive pain management, pulmonary hygiene, and supportive measures. Historically, external stabilization, including sandbags and towel clips, was recommended. However, this approach is considered obsolete.
Operative fixation of flail segments has not gained widespread acceptance, although several techniques have been described.44,62,79 Balci and colleagues compared the outcomes of open fixation of flail chest in 27 patients with that of mechanical ventilatory support using intermittent positive-pressure ventilation in 19 patients and synchronized intermittent mandatory ventilation in 18 patients.6 They found that only three-quarters of the patients who underwent open fixation required short-term ventilatory support postoperatively for a mean of 3.1 days compared with the other two groups, who required an average of 7.2 days. The mortality rate in the surgical group was 11.1%, compared with 27% for the ventilated patients. Selection of patients for either mode of treatment as well as other factors must be considered in evaluating the results. In 2007, Richardson and colleagues88 published a series of 35 patients with sternal fractures and 7 with multiple rib fractures. All were treated with open reduction and internal fixation, using titanium plates and screws, with excellent results.88 The communication of these authors suffers from no randomization and few hard variables to be useful in decision making concerning rib fixation.
Mortality from flail chest has improved from the 30% to 40% reported in the mid-1970s94,105 to 11% to 16% reported in the 1980s.22,35 However, flail chest injuries may have long-term consequences. In 1984, Landercasper and associates61 documented impaired pulmonary function in long-term survivors. Only 6% of their patients had severe enough pulmonary compromise to
require mechanical ventilation. Yet the long-term changes included dyspnea in 63%, abnormal exercise tests in 70%, abnormal spirometry in 57%, and persistent disabling pain in 49%. The etiology of these persistent pulmonary abnormalities is unclear, and whether internal stabilization of the chest wall would reduce the incidence of unsatisfactory long-term outcomes is unknown.
require mechanical ventilation. Yet the long-term changes included dyspnea in 63%, abnormal exercise tests in 70%, abnormal spirometry in 57%, and persistent disabling pain in 49%. The etiology of these persistent pulmonary abnormalities is unclear, and whether internal stabilization of the chest wall would reduce the incidence of unsatisfactory long-term outcomes is unknown.
Other Bony Fractures of the Chest Wall
Sternal Fractures
Up to 4% of major motor vehicle crash victims present with sternal fractures.82 Older patients and front-seat vehicle occupants involved in frontal collisions are at greatest risk. The fracture is typically transverse and is located in the upper and midportions of the body of the sternum. The features that help establish the diagnosis of sternal fracture are physical exam demonstrating point tenderness, swelling, and deformity; chest radiograph showing sternal fracture on lateral view (Fig. 73-3); CT scan delineating fracture23; and MRI.5 The last of these tests is useful particularly for evaluation of the sternoclavicular joint.
Sternal fractures are frequently associated with other severe intrathoracic injuries.15 Specific injury to the myocardium is common; however, its clinical significance and that of abnormal test results in hemodynamically stable patients is questionable and has been challenged.20,121
Age and mechanism of injury play a key role in associated injuries. A 1993 prospective review by Hill and associates49 of over 12,000 patients showed that vehicle occupants with isolated sternal fractures had less injury overall compared with those who had no such fractures.49 In their series, patients with sternal fractures included a greater proportion of patients >50 years of age (56% versus 11%), more females (55% versus 34%), and more seat belt wearers (70% versus 40%). There was no association with serious visceral chest injury (including cardiac contusion). Motor vehicle occupants with sternal fractures had less injury overall compared with those without sternal fractures. However, multiple organ injuries were associated with fractures of the thoracic spine.
Treatment of sternal fractures is similar to that for rib fractures. It consists of good pain control and appropriate pulmonary hygiene.91 Surgical intervention, on the other hand, is indicated in severely displaced fractures. Internal fixation with plating systems or cross wires is done through a midline incision and is the favored procedure. In the uncommon situation of a flail sternum due to disruption of the costochondral junctions, external fixation as recommended by Henley47 as a viable alternative, minimizing the need for positive-pressure ventilation.
Scapular and Clavicular Fractures
Fractures of the scapula result from a severe force of impact. These fractures, which are uncommon, have an 80% to 90% incidence of accompanying injuries,68,106 with a mortality as high as 10%.3 Because of the high incidence of concurrent brachial plexus injuries, a detailed neurovascular examination should be performed. Treatment consists of shoulder immobilization with subsequent early range-of-motion exercises. Surgical repair may be indicated when the function of the glenohumeral joint is impaired.43
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree