Benign Germ Cell Tumors of the Mediastinum
Mark S. Allen
Victor F. Trastek
Peter C. Pairolero
Incidence and Terminology
The incidence of mediastinal tumors, as noted by Cocks and Kamdar,6 is approximately 1 in 3,400 hospital admissions. Benign germ cell tumors are uncommon and account for 5% to 10% of all mediastinal tumors. Mullen and Richardson22 have proposed a useful classification system of mediastinal germ cell tumors. They divided them into three categories: benign germ cell tumors, seminomas, and nonseminomatous germ cell tumors, also called malignant teratomas. The germ cell tumors consist of choriocarcinoma, yolk sac carcinoma, embryonal carcinoma, and teratocarcinoma (see Chapters 193 and 194).
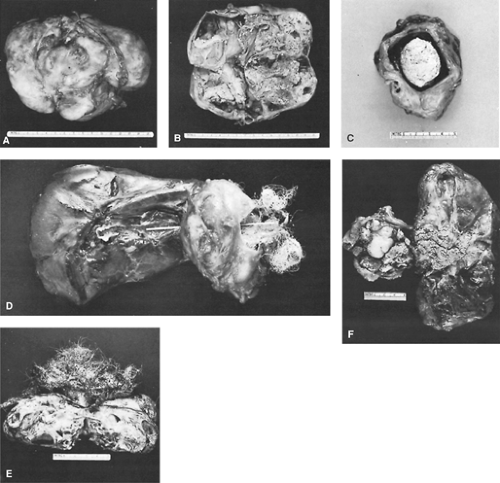
Benign germ cell tumors have also been referred to as epidermoid cysts, dermoids, benign teratomas, or simply teratomas. The term teratoma is derived from the Greek word teras, which means “monster,” an apt name for these often bizarre-appearing tumors (Fig. 192-1). The terms embryoma, teratoid tumor, and teratoblastoma imply malignancy and are therefore misleading and should not be used. Similarly, the terms bidermoma and tridermoma, which attempt to describe the number of germ cell layers in the tumor, are cumbersome and awkward and are rarely used. Dermoid cyst is used commonly and is a descriptive term for the often cystic nature of this tumor. Since these tumors are true neoplasms and contain multiple germ cell layers they are probably best termed benign teratomas.
Histologically, benign teratomas have been defined by Willis39 as tumors composed of tissue foreign to the organ or anatomic site in which they arise. Often included but not an absolute requirement is that tissue from all three primordial germ cell layers be present (i.e., ectoderm, mesoderm, and endoderm). With incomplete differentiation, one or two germ cell layers may be missing.
Incidence and Epidemiology
Only 5% to 10% of germ cell tumors are extragonadal, but the mediastinum is the most common extragonadal site, as noted in the publications of Hession and Simpson10 as well as Sohn33 and Greif8 and their associates. According to Hainsworth and Greco,9 the exact percentage depends on the age group studied. In a collective review of anterior mediastinal tumors, Mullen and Richardson22 found that germ cell tumors accounted for approximately 15% of the anterior mediastinal tumors in adults (85% of these were benign) and 25% in children, all of which were benign.
Typically, germ cell tumors occur in young adults in the second to fourth decades of life, with equal sex distribution. Wychulis and colleagues,40 in a review of 1,064 mediastinal tumors managed surgically between 1929 and 1968 at the Mayo Clinic, found that 99 (9.3%) were teratomas. Most occurred in young adults, with half occurring in individuals 11 to 30 years of age. Benign teratomas had a slight predominance in women as compared with men; however, most series found no sex ratio differentiation. The percentage of benign teratomas was higher in a series from Japan, where Suzuki and coworkers36 reported that 23% of mediastinal masses were teratomas. Although not the most common type of mediastinal mass, benign teratomas historically have constituted 80% to 85% of all mediastinal germ cell tumors. However, Davis and associates7 reported on 400 mediastinal masses seen at Duke University Medical Center from 1930 to 1986; 42 were germ cell tumors, and of these, only 21 were benign. Whether this reflects an increasing number of malignant germ cell tumors or is only the result of the patterns of referral is unknown.
Almost all benign teratomas occur in the anterior compartment of the mediastinum. Only 3% to 8% are located in either the posterior portion of the visceral compartment or the paravertebral regions, as illustrated by the review by Shirodkar and coworkers.31 The benign lesions in the anterior compartment may protrude to one side or the other. Shirodkar and associates31 found that 46 projected to the left, 34 toward the right, and 6 were midline.
Pathophysiology
Theories of origin of benign teratomas must account for their usual location and the presence of multiple germ cell layers. Three theories exist to describe the origin of mediastinal germ cell tumors. One theory, as espoused by Schlumberger,30 suggests that these tumors arise from cells adjacent to the third and fourth brachial clefts. Because this tissue is juxtaposed to the thymus gland, it is unclear whether the tumor arises from
thymic tissue or is just intimately adjacent to this organ. Another theory, as noted by Mullen and Richardson,22 suggests that benign teratomas arise from primordial germinal nests that did not complete the migration from the urogenital ridge to the gonads during development. Last, Wychulis and colleagues40 as well as Hession and Simpson10 believe these tumors may arise from pluripotent cells that have the capacity to form tissue from all three embryonic layers foreign to the area where they are located.
thymic tissue or is just intimately adjacent to this organ. Another theory, as noted by Mullen and Richardson,22 suggests that benign teratomas arise from primordial germinal nests that did not complete the migration from the urogenital ridge to the gonads during development. Last, Wychulis and colleagues40 as well as Hession and Simpson10 believe these tumors may arise from pluripotent cells that have the capacity to form tissue from all three embryonic layers foreign to the area where they are located.
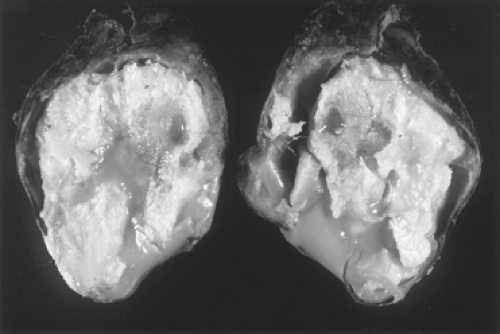 Figure 192-1. Gross photograph of a cross section of a benign teratoma. Note the hair and sebaceous material present. A well-formed capsule is present that is thin in several areas. |
Benign teratomas can be either cystic or solid or a combination of both. Lewis and associates18 reported that the size of the average germ cell tumor was 10.5 × 8.6 × 5.4 cm and that it had an average weight of 415 g (range 48 to 1,820 g). Wall thickness of the encapsulated benign teratoma ranged from 0.5 to 2.0 cm (Fig. 192-2).
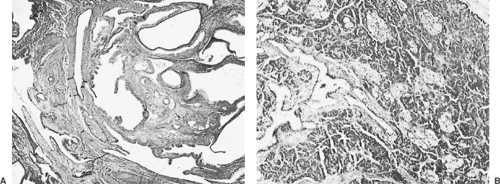
Rosado-de-Christenson and associates26 have rightly pointed out that, histologically, benign teratomas consist of all three primordial layers: ectoderm (skin and hair), mesoderm (bone, fat, and muscle),
and endoderm (respiratory epithelium and gastrointestinal tract) (Fig. 192-3). Therefore it is not surprising to find all types of histologic tissue in teratomas. Skin, pilosebaceous tissue, smooth muscle, fat, and respiratory epithelium occur in more than half of the tumors. Teeth, bone, cartilage, neural tissue, and pancreatic tissue have been reported in benign teratomas by Willis39 and Wychulis and colleagues40 as well as by many of the aforementioned researchers. These tumors, when mature, contain well-differentiated tissue components. When immature, they contain less well-differentiated tissue. In infants, immature teratomas behave similarly to mature teratomas, but in older patients, Sohn and coworkers33 have pointed out that the immature teratomas are more aggressive, resembling malignant teratomas.
and endoderm (respiratory epithelium and gastrointestinal tract) (Fig. 192-3). Therefore it is not surprising to find all types of histologic tissue in teratomas. Skin, pilosebaceous tissue, smooth muscle, fat, and respiratory epithelium occur in more than half of the tumors. Teeth, bone, cartilage, neural tissue, and pancreatic tissue have been reported in benign teratomas by Willis39 and Wychulis and colleagues40 as well as by many of the aforementioned researchers. These tumors, when mature, contain well-differentiated tissue components. When immature, they contain less well-differentiated tissue. In infants, immature teratomas behave similarly to mature teratomas, but in older patients, Sohn and coworkers33 have pointed out that the immature teratomas are more aggressive, resembling malignant teratomas.
Presentation
Benign teratomas present equally in men and women and can be found as early as the first month of life and as late as the eighth decade of life. The tumor tends to be slow-growing; thus many patients have no signs or symptoms when the mass is initially discovered. Le Roux16 reported that 62% of his patients were asymptomatic, although Lewis and associates18 found that only 36% of their patients were so.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree