Benign and Malignant Tumors of the Trachea
L. Penfield Faber
William H. Warren
Despite their histologic similarity to tumors of the mainstem bronchus and lung, tumors of the trachea are approximately 100 times less common than bronchial tumors and constitute only 2% of all upper respiratory tract tumors, as reported by Perelman and Koroleva.55 Tracheal cancer is responsible for <0.1% of all cancer deaths, as noted by Pearson.52 The most common malignant tumors are squamous cell carcinoma and adenoid cystic carcinoma.
Malignant tumors of the trachea are more common than benign tumors. Houston31 reviewed 30 years of experience at the Mayo Clinic, during which 53 of 90 tracheal tumors were found to be malignant. Hajdu29 reported a series of 41 primary malignancies of the trachea that were treated over a period of 33 years at a major cancer hospital. This number represents slightly more than one malignant tracheal tumor per year seen at a major referral center, which emphasizes the relative rarity of these tumors. In a center study of 208 patients with primary tracheal tumors reported by Regnard,59 181 were malignant and 27 were benign; however, in a review of 43 tracheal tumors occurring in infants and children, Gilbert20 noted that 93% were benign. Desai11 reviewed 36 reported tracheal tumors in infants and children from 1965 to 1995; 23 were benign and 13 were malignant. Malignant fibrous tumors and mucoepidermoid carcinoma were the more common malignant variants in children. The predominant benign tumors in children are hemangiomas, fibromas, and papillomas.
Secondary tumors also involve the trachea. Direct extension into the trachea occurs from cancers of the thyroid, larynx, lung, and esophagus. Mediastinal tumors may directly invade the trachea; the most common is lymphoma. Metastasis to the trachea is uncommon, but breast cancer, melanoma, and sarcomas have all been found in the trachea.
Symptoms and Findings
Dyspnea and shortness of breath on exertion are the most common presenting symptoms, according to Perelman,55 and occur when the tracheal lumen has been reduced to one-third of its normal cross-sectional area, with dyspnea in 80% of patients. Cough is a common symptom associated with tracheal neoplasms, but no particular salient features are associated with the cough to indicate that it is caused by a tracheal tumor. As the airway narrows, the classic symptom of wheezing becomes apparent. Stridor is a more prominent form of wheezing and indicates significant compromise of the airway. Often, a patient with a tracheal tumor is treated for asthma for a prolonged period.
Hemoptysis occurs in approximately 20% of patients with tracheal neoplasms and is most commonly seen in patients with squamous cell carcinoma. People with benign tumors rarely if ever present with hemoptysis. A change in voice quality can be related to paralysis of the vocal cord resulting from invasion of the recurrent laryngeal nerve or by direct extension of an upper tracheal tumor into the larynx. Recurrent pneumonitis, either unilateral or bilateral, can occur from obstruction of a main bronchus.
Perelman55 reported that the interval between the onset of early symptoms and diagnosis was approximately 25 months for benign tumors and 8 months for malignant tumors. Regnard59 noted that the mean duration of symptoms for patients with adenoid cystic carcinoma was 12 months, and for those with tracheal cancers, 4 months. The long duration of symptoms is emphasized by Perelman in finding that 23% of patients with tracheal tumor arrived at the Center for Surgery with life-threatening asphyxia. Regnard59 noted acute respiratory failure in 29% of patients.
Dysphagia is an uncommon symptom that indicates esophageal compression by a large bulky neoplasm. Auscultation of the chest reveals a coarse wheeze that is enhanced by rapid and deep inspiration. The wheeze is more prominent on inspiration than on expiration and is different from the wheezing commonly associated with bronchial asthma. Locations of tumors in the trachea, as reported by Perelman,56 were the thoracic trachea in 77, the cervical trachea in 26, and the carinal region in 41 patients.
Diagnosis
Radiographic Features
Careful inspection of the tracheal air column on posteroanterior and lateral chest radiographs sometimes reveals a tracheal tumor (Fig. 81-1). Oblique views of the trachea, lateral neck
radiographs, and hyperextension reveal the presence of the tumor but do not provide specific information necessary for a planned resection and reconstruction. Linear tomography, as described by Weber and Grillo,72 provides excellent visualization of the extent of the tumor (Fig. 81-2). Tracheal tomograms, however, are not effective for determining extraluminal extension of the tumor or lymph node invasion, and this technique is no longer available in most centers.
radiographs, and hyperextension reveal the presence of the tumor but do not provide specific information necessary for a planned resection and reconstruction. Linear tomography, as described by Weber and Grillo,72 provides excellent visualization of the extent of the tumor (Fig. 81-2). Tracheal tomograms, however, are not effective for determining extraluminal extension of the tumor or lymph node invasion, and this technique is no longer available in most centers.
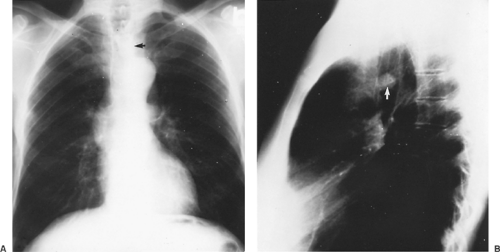 Figure 81-1. A: A chondroma is seen on this frontal chest radiograph (arrow). B: A tracheal hamartoma is clearly identified on this lateral chest radiograph. |
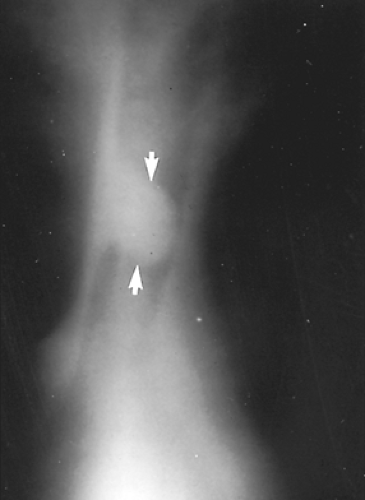 Figure 81-2. Linear tomogram clearly depicting the length of involvement of a carcinoid tumor of the trachea. |
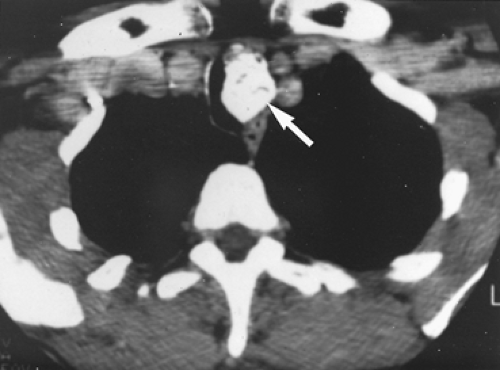
Computed tomography (CT) has replaced linear tomography as the primary method of radiologic evaluation of a tracheal tumor. Mediastinal extension, esophageal compression, and tracheal lumen size are all seen clearly on the CT (Fig. 81-3). Using thin-cut CT sections and knowing the distance between the cuts can permit a moderately accurate measurement of the length of
trachea involved by the tumor. Gross pathologic characteristics of the tumor are also identified on CT. Benign lesions are frequently round and smooth and approximately 2 cm in diameter. The tumor is generally inside the lumen of the trachea, and the well-circumscribed nature of the tumor is clearly evident. Calcification is a characteristic of benign lesions and is seen in tumors such as chondromas and hamartomas (Fig. 81-4). Calcification is also present, however, in a chondrosarcoma; malignant tumors extend up and down the trachea for several centimeters, while the surface of the tumor is irregular and possibly ulcerated. The tracheal wall is obviously invaded by the tumor at its base, and extraluminal growth may be present (Fig. 81-5). Enlarged lymph nodes usually indicate metastatic spread. The CT scan should always be done with infusion to clearly delineate the relationship of the tumor to the superior vena cava and other vascular structures in the mediastinum. No specific radiologic findings that differentiate malignant tumors of the trachea exist.
trachea involved by the tumor. Gross pathologic characteristics of the tumor are also identified on CT. Benign lesions are frequently round and smooth and approximately 2 cm in diameter. The tumor is generally inside the lumen of the trachea, and the well-circumscribed nature of the tumor is clearly evident. Calcification is a characteristic of benign lesions and is seen in tumors such as chondromas and hamartomas (Fig. 81-4). Calcification is also present, however, in a chondrosarcoma; malignant tumors extend up and down the trachea for several centimeters, while the surface of the tumor is irregular and possibly ulcerated. The tracheal wall is obviously invaded by the tumor at its base, and extraluminal growth may be present (Fig. 81-5). Enlarged lymph nodes usually indicate metastatic spread. The CT scan should always be done with infusion to clearly delineate the relationship of the tumor to the superior vena cava and other vascular structures in the mediastinum. No specific radiologic findings that differentiate malignant tumors of the trachea exist.
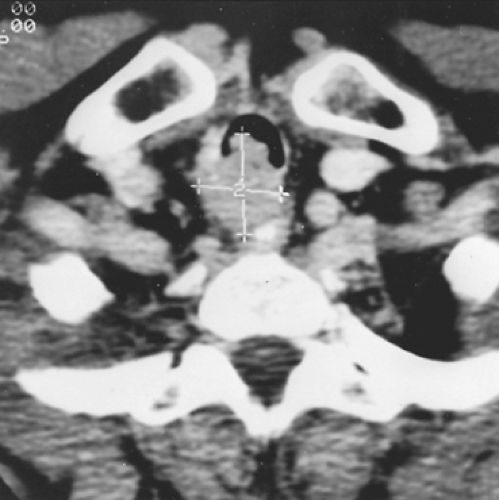 Figure 81-3. Computed tomogram identifying posterior mediastinal extension of an adenoid cystic carcinoma. |
Magnetic resonance imaging (MRI) can offer some advantages in the assessment of tracheal neoplasms. Coronal, oblique, and sagittal views can be obtained that demonstrate long lengths of the trachea and delineate a more precise length of tracheal involvement by the tumor. T1-weighted images characterize the anatomy of the trachea and adjacent soft tissues quite well. MRI also clearly depicts adjacent vascular structures and permits assessment of possible invasion of these structures. MR angiography can be used in place of conventional angiography when vena caval obstruction is evaluated. Three-dimensional helical CT of the central airway can provide precise anatomic information for the planning of endobronchial and surgical procedures. Kauczor36 diagnosed 36 patients with proven airway obstruction utilizing this technique, and the majority had bronchial carcinoma with mediastinal or hilar lymphadenopathy. The anatomy of the lesions was clearly depicted and closely correlated with the bronchoscopic findings. Three-dimensional helical CT provides additional information for assessing the distal airway when the bronchoscope cannot be passed through the obstructing lesion. This radiologic technique is most valuable in planning tracheal resections or in monitoring palliative efforts treating tracheal neoplasms. If the patient complains of dysphagia, a barium examination of the esophagus may demonstrate compression or possibly invasion and further define the extraluminal extent and size of the tracheal neoplasm.
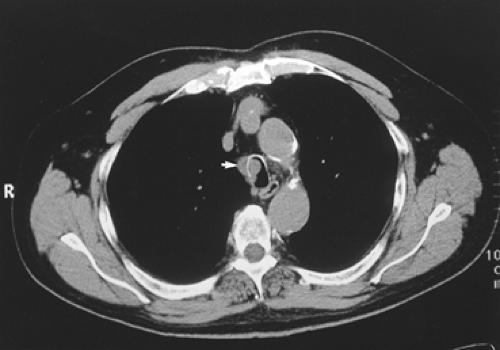 Figure 81-5. Computed tomographic scan showing adenoid cystic carcinoma extending through the tracheal cartilage. |
Pulmonary function studies reveal airway obstruction characterized by a reduced volume of air expired in 1 second, a significantly decreased peak flow rate, and a flattened expiratory flow-volume loop. Maximum voluntary ventilation is diminished. Pulmonary function tests may also delineate the presence or absence of parenchymal lung disease.
Bronchoscopy
Bronchoscopy is a necessary step in the diagnosis and clinical evaluation of a patient with a tracheal tumor. Biopsy and manipulation of a tracheal tumor is potentially hazardous because bleeding can cause complete tracheal obstruction. A sedated or anesthetized patient may be unable to maintain adequate ventilation, and the passage of an endotracheal tube may not be possible because of the obstructing tumor. The bronchoscopic examination should be carried out by an experienced endoscopist who can insert an open-tube bronchoscope through the tumor to establish an airway and manage any complications of hemorrhage.
A bronchoscopic examination is always conducted in the operating room, where ventilating bronchoscopes and biopsy forceps are available and a trained anesthesiologist is close at hand. Grillo23 believes that when the indications for primary tracheal resection are clear-cut, bronchoscopy can be deferred until the time of the operative procedure and frozen sections used to determine histology. With the flexible fiberoptic bronchoscope, however, a careful examination and biopsy can be accomplished in an awake patient. A preresection bronchoscopy offers several advantages:
Vocal cord function is evaluated, and the entire larynx and cricoid cartilage are seen clearly. This visualization is particularly important for upper tracheal lesions in which a partial resection of the cricoid or laryngectomy may be required.
The gross characteristics of the tumor should be noted, and an impression can be gained whether the tumor is benign or malignant.
The size of the tracheal lumen should be clearly noted. This assessment is extremely helpful in planning anesthetic management of the airway during the initial phase of tracheal resection.
A biopsy sample can be obtained with the small biopsy forceps through the flexible instrument, and knowing the histology is of benefit in planning the treatment program.
Frequently, the small, flexible fiberoptic bronchoscope can be inserted past the neoplasm and the distal airway carefully examined. The length of the tumor can be carefully measured and correlated with the radiologic measurements.
These findings are extremely helpful in planning the surgical approach and resection. However, the endoscopist must be prepared to insert an open-tube bronchoscope if airway obstruction does occur.
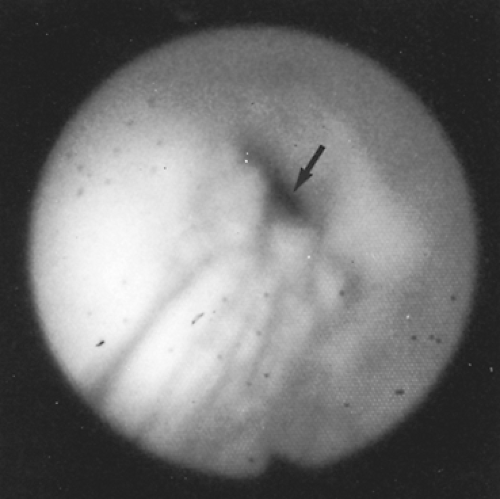
The decision for biopsy requires careful judgment, and the biopsy should not be done if there is any possibility of airway compromise (Fig. 81-6). Houston31 reported that of 53 primary cancers of the trachea, the diagnosis was established by bronchoscopic biopsy without complication in 47 patients (Fig. 81-7).
When life-threatening airway obstruction occurs from a tracheal tumor or bleeding from a biopsy obstructs the airway, an adequate tracheal lumen can be established by coring out the tumor with the rigid bronchoscope and biopsy forceps, as described by Mathisen.44 Regnard and colleagues59 recommend the relief of tracheal obstruction to better define location and size of the tumor and provide a more adequate airway. In their series of 208 tracheal tumors, airway obstruction was relieved by laser treatment in 62 of 71 patients, by bronchoscopic debridement in 5, and by cryotherapy in 2. Tracheostomy was done to provide an adequate airway in 2 patients. Daddi9 described several advantages associated with the endoscopic treatment of airway obstruction before attempted curative resection. They include the improvement of respiratory function, a better assessment of the exact location of the tumor by endoscopic means, more reliable CT scanning of the airway, and improvement of the patient’s performance status with associated pulmonary therapy and antibiotics. Endoscopic debridement was accomplished with ventilating rigid bronchoscopes and the neodymium:yttrium-aluminum-garnet (Nd:YAG) laser.
 Figure 81-6. An adenoid cystic carcinoma partially obstructing the tracheal lumen. The flexible bronchoscope passed easily and biopsy was done with evaluation of the distal trachea. |
Benign Tumors
Gilbert20 reported that the common benign tumors of the trachea are chondroma, papilloma, fibroma, and hemangioma. Benign tumors most often occur in the upper third of the trachea in children and are more common in the lower third in adults, frequently arising from the membranous portion of the trachea (Table 81-1).
Chondroma
According to Mark,42 the most common benign mesenchymal tumor of the trachea is a chondroma (Fig. 81-8). These tumors histologically duplicate normal cartilage and can exhibit vascular invasion. Endoscopically, a chondroma appears as a firm white nodule projecting into the lumen of the trachea. The tumor occurs in a 4:1 preponderance in men and is more common in adults than in children. No definite etiology for this lesion has been described. A chondroma occurs more frequently in the larynx than in the trachea. Biopsy of the lesion can be difficult because of its firm consistency; this characteristic can indicate the diagnosis. Vascularity is minimal, and the lesion can be removed easily through the bronchoscope. Recurrence after endoscopic removal has been observed, however, and Salminen62 reported malignant transformation to chondrosarcoma. Recommended treatment for recurrence is segmental tracheal resection.
Table 81-1 Benign Tracheal Tumors | ||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Papilloma
A solitary papilloma of the trachea is rare, but this lesion does occur in adults, as described by Maxwell.45 Papillomas are sessile growths lined by squamous epithelium covering fibrovascular cores. Cytologic atypia may be present. A solitary benign papilloma is easily removed through the open-tube bronchoscope, and the base of the tumor can be ablated with the Nd:YAG laser. Periodic endoscopic surveillance is indicated, and recurrence can be treated with laser ablation.
Juvenile laryngotracheal papillomatosis is common in children and is seen more frequently than is solitary papilloma of the trachea. It accounts for 60% of benign tracheal tumors in children, according to Beattie.2 It has been linked with human papillomavirus types 6 and 11. Papillomatosis more commonly involves the larynx, but it is found in the tracheobronchial tree in 20% of patients. It follows a relatively benign course, requiring repeated endoscopic removal, with recurrence rates as high as 90%. Complications include chronic cavitary respiratory papillomatosis resulting from proliferation of the virus in the distal bronchial tree, as noted by Karley.35 Malignant transformation of papillomatosis has been reported in patients with a history of radiation therapy or smoking, but it may also occur in nonsmokers, as noted by Guillou.28 The types of therapy for the more invasive form of the disease include photodynamic therapy with sensitization of the papilloma cells using hematoporphyrin diacetate, as described by Kavuru37 and Basheda.1 Leventhal39 reported successful treatment with the use of lymphoblastoid interferon-N1.
Fibroma
Fibroma accounts for approximately 20% of all benign tumors in adults.2 Mark42 reported that fibroma is more common than fibrosarcoma and can be difficult to distinguish from a fibrous histiocytoma. The tumor is well circumscribed and consists of fibroblasts embedded in intercellular collagen. A benign fibroma is easily removed through the bronchoscope, followed by careful laser ablation of the base of the tumor. Local recurrence would be unusual, but if it did occur, segmental tracheal resection would be indicated.
Hemangioma
Hemangioma of the trachea is similar to hemangioma of the skin in infants, with an increase in size at 1 month of age followed by a spontaneous decrease in size at 1 year. It may arise in the trachea or extend into the tracheal lumen from a hemangioma located in the mediastinum. Treatment may require tracheostomy to provide an adequate airway, followed by repeated small doses of radiation therapy to shrink the tumor. Weber73 used steroids to cause regression. Many lesions require no treatment, and natural regression frequently occurs. Larger hemangiomas of the lower trachea may require direct surgical intervention. In this instance, a careful plan must be developed for airway control during excision of the tumor.
Other Benign Tumors
Granular Cell Tumor
The granular cell tumor occurs less frequently in the trachea than it does in the tongue, neck, or larynx. Burton6 summarized the reported experience with this tumor in the trachea and identified 24 cases. The tumor is thought to be of neurogenic origin and derives from Schwann cells. Malignant transformation of the granular cell tumor does occur in other sites, but it has never been reported in the trachea. Both endoscopic and partial tracheal resections have been successful as treatment of this lesion. Local recurrence after endoscopic resection may require partial tracheal resection. Daniel and coworkers10 recommended removal of tumors >1 cm by a segmental tracheal resection because of the increased risk for full-thickness wall involvement with tumors of this size. Smaller lesions (<1 cm) are easily ablated by endoscopic Nd:YAG laser therapy. van der Maten43 identified 30 patients with granular cell tumors of the tracheobronchial tree, and 11 patients received no treatment other than confirmatory biopsy. They basically remained asymptomatic up to 6 years’ follow-up. Endoscopic therapy would certainly be applicable to both small and large tumors as well, with resection reserved for local recurrence, because malignant transformation of this tumor in the trachea has yet to be reported.
Fibrous Histiocytoma
Fibrous histiocytoma is a histologically benign tumor in the trachea, but it can be locally infiltrative (Fig. 81-9). An associated prominent inflammatory component can cause the tumor to be termed an inflammatory pseudotumor. The behavior of this tumor in the trachea appears to be benign, but because of its local infiltration, segmental resection is the treatment of choice. Resection of a malignant fibrous histiocytoma of the trachea was reported by Randleman,58 with identification of one other case in the literature.
Glomus Tumor
Glomus tumor is usually a benign neoplasm arising from specialized cells surrounding arteriovenous anastomoses. Garcia-Prats17 reviewed the literature and found six cases of tracheal origin. This tumor can be confused histologically with the carcinoid tumor; immunohistochemistry is recommended for confirmation. Menaissy48 reviewed nine cases of glomus tumor of the trachea and noted that the tumor can extend outside the tracheal wall. Segmental tracheal resection is recommended, with no expected recurrence. The World Health Organization states that a glomus tumor should be considered malignant if the tumor is >2 cm in size in a subfascial location, contains atypical mitotic figures, or exhibits marked nuclear atypia with any level of mitotic activity.
Lipoma
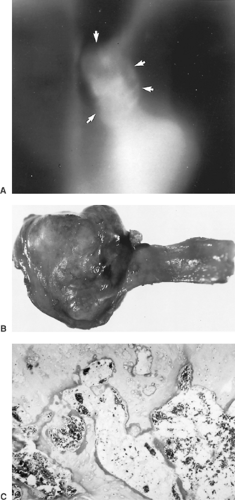
Tracheal lipoma is a rare lesion, with five cases reported (Fig. 81-10). Chen8 described a patient with a tracheal lipoma requiring major tracheal resection for complete removal. Other authors describe endoscopic removal. It is only logical to approach this tumor with endoscopic removal because it is a completely benign tumor, and any local recurrence can be treated successfully with laser therapy.
Leiomyoma
A leiomyoma may occur as a primary tracheal tumor, usually in the distal third of the trachea.42 Both tracheal resection and endoscopic removal have been described in rare case reports.
Neurogenic Tumors
The neurofibroma can occur in the trachea as a primary tumor, but it is not associated with generalized neurofibromatosis. This tumor can invade the wall of the trachea, and segmental resection would be the treatment of choice.
Pang51 presented two cases of primary neurilemoma (schwannoma) of the trachea. His review identified 14 other
reported cases. These tumors derive from the Schwann cell and are typically slow-growing. The tumor usually has a broad base, and complete removal by bronchoscopy would be difficult. These tumors can recur with malignant potential, and segmental tracheal resection is the treatment of choice. They can be malignant at initial diagnosis and segmental resection with adjuvant radiation would be the treatment of choice.63 Total positive margins were recorded as tumor involving or approaching within 1 mm either the radial or tracheal surgical margin.
reported cases. These tumors derive from the Schwann cell and are typically slow-growing. The tumor usually has a broad base, and complete removal by bronchoscopy would be difficult. These tumors can recur with malignant potential, and segmental tracheal resection is the treatment of choice. They can be malignant at initial diagnosis and segmental resection with adjuvant radiation would be the treatment of choice.63 Total positive margins were recorded as tumor involving or approaching within 1 mm either the radial or tracheal surgical margin.
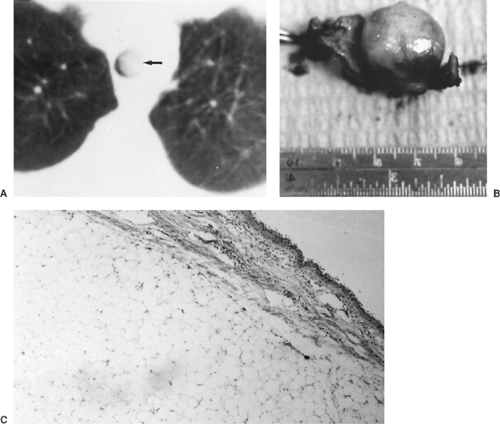 Figure 81-10. A: Computed tomogram showing almost total tracheal obstruction by a lipoma. B: Tracheal resection was required for the removal of the broad-based lesion. C: On microscopic examination, the fatty tumor was seen in the submucosa of the trachea.
Stay updated, free articles. Join our Telegram channel
Full access? Get Clinical Tree
 Get Clinical Tree app for offline access
Get Clinical Tree app for offline access

|