Our objective was to evaluate the implant and mid-term outcomes of transvenous pacemaker or internal cardioverter-defibrillator placement by alternative axillary approaches compared to the infraclavicular approach in a pediatric and congenital heart disease population. We conducted a retrospective review of all patients with new endocardial heart rhythm devices placed at 4 pediatric arrhythmia centers. A total of 317 patients were included, 63 had undergone a 2-incision axillary approach, 51 a retropectoral axillary approach, and 203 an infraclavicular approach. Congenital heart disease was present in 62% of the patients. The patients with the 2-incision axillary approach were younger and smaller. The patients with the retropectoral axillary approach were less likely to have undergone previous cardiac surgery and were more likely to have had an internal cardioverter-defibrillator placed. The duration of follow-up was 2.4 ± 1.9 years for the 2-incision axillary, 2.6 ± 2.6 years for retropectoral axillary, and 3.5 ± 1.4 years for the infraclavicular technique (p = 0.01). No differences were seen in implant characteristics, lead longevity, implant complications, lead fractures or dislodgements, inappropriate internal cardioverter-defibrillator discharges, or device infections among the 3 groups. In conclusion, our data support that the outcomes of axillary approaches are comparable to the infraclavicular approach for endocardial heart rhythm device placement and that axillary approaches should be considered a viable option in patients with pediatric and congenital heart disease.
Infraclavicular placement is the standard approach for endocardial heart rhythm devices, including pacemakers and internal cardioverter-defibrillators (ICDs). The surgical scar and imprint from the device placed in this location can be quite noticeable and unsightly. Straps, such as those on seatbelts, backpacks, purses, or golf bags can rub and cause discomfort at the site. Although seemingly minor, these considerations can be of particular importance to young patients. To address these concerns, placing transvenous devices using various axillary approaches has been proposed. Axillary approaches allow the primary incision to be hidden underneath the arm and thus provide an improved cosmetic result for patients. The purpose of the present study was to compare the clinical outcomes of patients who had undergone 2 different axillary approaches with the clinical outcomes of those who had undergone the infraclavicular approach for transvenous heart rhythm device implantation in a pediatric and congenital heart disease population.
Methods
This was a retrospective, multicenter, international study that included 4 pediatric arrhythmia centers: the Children’s Hospital in Denver, Colorado and its affiliates; Glenfield Hospital in Leicester, England; the University of Iowa Children’s Hospital in Iowa City, Iowa; and the CS Mott Children’s Hospital in Ann Arbor, Michigan. The study centers were chosen because both axillary and infraclavicular approaches were used for the placement of endocardial heart rhythm devices. Each center provided institutional review board approval. Electrophysiology databases at each center were reviewed for all new endocardial pacemaker or ICD implants from January 2000 to August 2008. All included patients were <18 years of age or had congenital heart disease.
The medical records were reviewed for patient demographics, device implantation technique, procedure times (typically recorded as the “procedure time” or “anesthesia time”), and fluoroscopy times. The following parameters were documented at the initial implantation and at follow-up: lead sensing parameters, lead pacing thresholds, defibrillation thresholds, appropriate and inappropriate shocks, and complications. ICD discharges were deemed appropriate if they had occurred secondary to the detection of ventricular arrhythmias faster than the programmed detection criteria. All other causes of discharge, including supraventricular tachycardias, were deemed inappropriate. Specific complications of interest included infection, lead dislodgement, lead fracture, and the need for surgical reintervention. Because of the known tendency of the Medtronic Sprint Fidelis (Medtronic Inc., Minneapolis, Minnesota) lead to fracture, resulting in a medical device recall, these lead fractures were considered separately from fractures of other lead types.
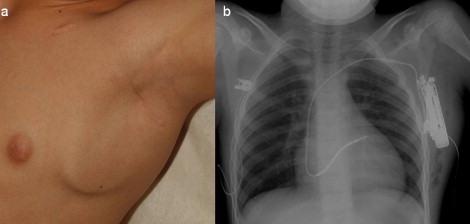
The patients were divided into 3 groups according to the technique used for placement of their device: 2-incision axillary, retropectoral axillary, and infraclavicular. The 2-incision axillary technique was performed at the Children’s Hospital in Denver and its affiliates and Glenfield Hospital in Leicester, England. This technique included a 1-cm incision in the infraclavicular region. From this incision, the subclavian vein was accessed, and the leads were placed and tied down at this location. A second incision was then made high in the axilla. The leads were tunneled from the infraclavicular pocket to the axillary pocket in a submuscular plane. The leads were attached to the generator that was then placed in the axillary pocket ( Figure 1 ).
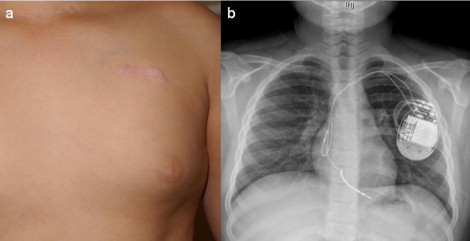
The retropectoral axillary technique was performed at the University of Iowa Children’s Hospital and CS Mott Children’s Hospital. This technique involves the creation of a 4-cm incision along the anterior axillary line. A pocket was created on the anterior chest, in a submuscular location. The leads were placed through this incision by accessing the subclavian or axillary vein. The leads were then placed into the generator, and the generator was placed into the retropectoral pocket ( Figure 2 ).

The infraclavicular approach includes the traditional location for device placement. Patients from all 4 study centers were included in this group. For the infraclavicular approach, a 4-cm incision was made in the infraclavicular region. Venous access and lead placement occurred through this incision and could be accomplished from the subclavian vein, axillary vein, or cephalic vein. A pocket was then created in either the premuscular or submuscular plane for device placement ( Figure 3 ).
Statistical analysis of the data used the mean ± standard deviation to summarize the continuous variables, and t tests were performed to compare the mean values among the groups. Percentages were used to summarize each of the dichotomous variables, and the chi-square test or Fisher’s exact test was performed to compare the proportions among the groups.
Results
A total of 317 patients with new endocardial heart rhythm devices were identified during the study period ( Table 1 ). The 2-incision axillary approach was used in 63 patients, the retropectoral axillary approach in 51, and the infraclavicular approach in 203. The presence of structural congenital heart disease was similar in all 3 groups. The 2-incision axillary population was younger and lighter in weight than the other 2 groups. The retropectoral axillary population was less likely to have a history of cardiac surgery.
| Variable | Two-Incision Axillary (n = 63) | Retropectoral Axillary (n = 51) | Infraclavicular (n = 203) | p Value |
|---|---|---|---|---|
| Age at implant (years) | 14 ± 6.6 | 17 ± 9.2 | 19 ± 10.7 | 0.01 ⁎ |
| Weight at implant (kg) | 46 ± 19.4 | 55 ± 19.6 | 60 ± 21.3 | 0.01 ⁎ |
| Female gender | 36 (57%) | 32 (63%) | 91 (45%) | 0.03 † |
| Congenital heart disease | 36 (57%) | 28 (55%) | 132 (65%) | 0.29 |
| Previous heart surgery | 29 (46%) | 14 (27%) | 103 (51%) | 0.01 ‡ |
⁎ Two-incision axillary group was significantly younger and lighter than other 2 groups.
† Retropectoral axillary group was more likely to be female than infraclavicular group; however, neither group was significantly different compared to the 2-incision axillary group.
‡ Retropectoral axillary group was significantly less likely to have undergone previous heart surgery.
All device placements were performed successfully using the planned implant technique ( Table 2 ). No difference was seen in implant procedure or fluoroscopy times. The proportion of patients with ICD placement versus pacemaker placement was greater in the retropectoral axillary group than in the other 2 groups. Of the patients receiving an ICD, the retropectoral group (25 of 38, 66%) and infraclavicular group (54 of 80, 67%) were more likely to have had devices placed for primary prevention than the 2-incision axillary group (5 of 20, 25%; p = 0.01).
| Variable | Two-Incision Axillary | Retropectoral Axillary | Infraclavicular | p Value |
|---|---|---|---|---|
| Pacemaker | 43 (68%) | 13 (25%) | 125 (62%) | <0.01 ⁎ |
| Internal cardioverter-defibrillator | 20 (32%) | 38 (75%) | 78 (38%) | |
| Total number of leads | 107 | 81 | 354 | |
| Procedure time (min) | 124 ± 50 | 144 ± 69 | 132 ± 66 | 0.33 |
| Fluoroscopy time (min) | 14.3 ± 13.8 | 17.2 ± 16.9 | 16 ± 13.9 | 0.65 |
| Leads | 0.11 | |||
| Single | 19 (30%) | 21 (41%) | 53 (26%) | |
| Dual | 44 (70%) | 30 (59%) | 149 (73%) | |
| Biventricular | 0 | 0 | 1 (1%) | |
| Lead position | 0.42 | |||
| Atrial | 49 (46%) | 31 (38%) | 164 (46%) | |
| Ventricular | 58 (54%) | 50 (62%) | 190 (54%) | |
| Atrial lead pacing thresholds | 0.9 | |||
| Implant | 0.79 ± 0.47 V @ | 0.79 ± 0.4 V @ | 0.8 ± 0.63 V @ | |
| 0.51 ± 0.06 ms | 0.53 ± 0.04 ms | 0.49 ± 0.06 ms | ||
| Follow-up | 1.3 ± 1 V @ | 1 ± 0.9 V @ | 1 ± 0.7 V @ | |
| 0.37 ± 0.15 ms | 0.48 ± 0.59 ms | 0.39 ± 0.13 ms | ||
| Atrial lead sensing (mV) | ||||
| Implant | 3.7 ± 1.7 | 3.7 ± 1.9 | 3.9 ± 2 | 0.7 |
| Follow-up | 2.5 ± 2 | 4.3 ± 2 | 3.7 ± 2 | <0.01 |
| Ventricular lead pacing thresholds | ||||
| Implant | 0.78 ± 0.86 V @ | 0.72 ± 0.27 V @ | 0.66 ± 0.53 V @ | 0.4 |
| 0.5 ± 0 ms | 0.49 ± 0.06 ms | 0.49 ± 0.1 ms | ||
| Follow-up | 1.6 ± 1.3 V @ | 1 ± 0.6 V @ | 1.3 ± 0.9 V @ | |
| Follow-up | 0.42 ± 0.22 ms | 0.44 ± 0.09 ms | 0.42 ± 0.2 ms | |
| Ventricular lead sensing (mV) | ||||
| Implant | 12.9 ± 6.5 | 11 ± 5.5 | 10.9 ± 5.5 | 0.07 |
| Follow-up | 7.8 ± 5.2 | 9.8 ± 5.7 | 8.9 ± 5.3 | 0.24 |
⁎ Retropectoral axillary group had significantly greater proportion of ICD.
The implant lead sensing and pacing parameters were similar among all 3 groups ( Table 2 ). The defibrillation threshold values were not available for all patients, and, in patients with available values, the device was frequently tested at a set output and not to threshold. The defibrillation threshold was 11.4 ± 3.8 J in 18 of 20 patients in the 2-incision axillary group, 9.7 ± 5 J in 16 of 38 patients in the retropectoral axillary group, and 15.8 ± 7.4 J in 34 of 80 patients in the infraclavicular group (p <0.01).
The patient follow-up duration was significantly longer for the infraclavicular population ( Table 3 ). No differences were seen among the 3 groups with respect to complications either <30 or >30 days after the procedure. Within the infraclavicular group, no difference was seen in complications with the use of a subcutaneous versus submuscular device placement. Of the reported complications, most were related to lead dislodgement (2% to 8%) or lead fracture (4% to 11%). The 2-incision axillary group had fewer lead dislodgements than the other 2 groups. All dislodged leads were removed and replaced. No differences were seen among the groups with respect to lead fractures. Atrial leads had more frequent complications (6% to 10%) than the non-Fidelis ventricular leads (2% to 4%), but the rate was not significantly different when stratified by placement technique (p = 0.58 and p = 0.66, respectively).
| Variable | Two-Incision Axillary (n = 63) | Retropectoral Axillary (n = 51) | Infraclavicular (n = 203) | p Value |
|---|---|---|---|---|
| Follow-up (years) | 2.4 ± 1.9 | 2.6 ± 2.6 | 3.5 ± 2.4 | 0.01 ⁎ |
| Complications <30 days | 4 (6%) | 3 (4%) | 12 (6%) | 0.83 |
| Complications >30 days | 10 (16%) | 5 (10%) | 24 (14%) | 0.56 |
| Reintervention at any point | 9 (14%) | 8 (16%) | 28 (14%) | 0.95 |
| Specific complications | ||||
| Lead dislodgement | 2 (3%) | 4 (8%) | 14 (7%) | 0.05 † |
| Lead fracture | ||||
| Fidelis | 4 (6%) | 1 (2%) | 8 (4%) | 0.5 |
| Non-Fidelis | 3 (5%) | 1 (2%) | 4 (2%) | 0.44 |
| Lead malfunction—other | 0 | 1 | 4 | |
| Infection | 0.16 | |||
| Superficial skin | 2 | 0 | 2 | |
| Pocket infection | 1 | 1 | 0 | |
| Endocarditis | 0 | 0 | 1 | |
| Pocket hematoma | 0 | 0 | 1 | |
| Pulmonary embolism | 1 | 0 | 0 | |
| New-onset arrhythmia | 1 | 0 | 0 | |
| Significant device site pain | 0 | 0 | 1 | |
| Pneumothorax | 0 | 0 | 1 |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


