A 256-slice coronary computed tomography angiography (CCTA) is an accurate method for detection and exclusion of obstructive coronary artery disease (OBS-CAD). However, accurate image interpretation requires expertise and may not be available at all hours. The purpose of this study was to evaluate the usefulness of a fully automated computer-assisted diagnosis (COMP-DIAG) tool for exclusion of OBS-CAD in patients in the emergency department (ED) presenting with chest pain. Three hundred sixty-nine patients in ED without known coronary disease underwent 256-slice CCTA as part of the assessment of chest pain of uncertain origin. COMP-DIAG (CorAnalyzer II) automatically reported presence or exclusion of OBS-CAD (>50% stenosis, ≥1 vessel). Performance characteristics of COMP-DIAG for exclusion and detection of OBS-CAD were determined using expert reading as the reference standard. Seventeen (5%) studies were unassessable by COMP-DIAG software, and 352 patients (1,056 vessels) were therefore available for analysis. COMP-DIAG identified 33% of assessable studies as having OBS-CAD, but the prevalence of OBS-CAD on CCTA was only 18% (66 of 352 patients) by standard expert reading. However, COMP-DIAG correctly identified 61 of the 66 patients (93%) with OBS-CAD with 21 vessels (2%) with OBS-CAD misclassified as negative. In conclusion, compared to expert reading, automated computer-assisted diagnosis using the CorAnalyzer showed high sensitivity but only moderate specificity for detection of obstructive coronary disease in patients in ED who underwent 256-slice CCTA. The high negative predictive value of this computer-assisted algorithm may be useful in the ED setting.
New-generation computed tomography (CT) scanners now available have high accuracy for detection of obstructive coronary artery disease (OBS-CAD) and a low rate of unassessable segments allowing accurate diagnosis in most of the scanned patients and safe discharge when appropriate. However, even with new-generation CT scanners accurate image interpretation requires expertise and may not be available at all hours. To promote rapid and accurate diagnosis, automated computer-assisted diagnosis (COMP-DIAG) tools have become prevalent in general medicine and particularly in diagnostic radiology, for example, in diagnosis of breast imaging and lung nodules. Because accurate assessment of coronary computed tomography angiography (CCTA) is time consuming, requires expertise, and may not be available at all times, an automated tool has been developed and tested to identify potentially OBS-CAD from CCTA. This may be particularly useful in the ED setting. Hence, the purpose of our study was to evaluate the performance characteristics of a COMP-DIAG tool in patients in ED with acute chest pain.
Methods
This single-center, retrospective, observational study was approved by the institutional review board with waiver of informed consent. The cohort included consecutive adult patients, without previously known CAD, who presented to the ED with chest pain of uncertain origin and underwent a 256-slice CCTA during ED evaluation. Study exclusion criteria were known CAD and/or previous revascularization or CCTA exclusion criteria (pregnancy, contrast allergy, renal function impairment [estimated glomerular filtration rate <60 ml/min], and unable to cooperate).
CCTA was performed using a 256-row scanner (Brilliance iCT; Philips Healthcare, Cleveland, Ohio), which has a longitudinal coverage of 8 cm, rotation time of 0.27 seconds, and a 120-kW generator. CCTA was performed either as prospectively triggered “step-and-shoot” scans or with helical retrospective electrocardiographic (ECG) gating. Oral and/or intravenous β blockers were used to lower heart rate when >70 beats/min. Sublingual nitroglycerine (0.4 mg) was given before CCTA to all patients with systolic blood pressure of ≥110 mm Hg and no clinical contraindications (such as aortic stenosis or suspected pulmonary embolism). CCTA was performed using a bolus of iohexol (Omnipaque 350 mg I/ml, GE Healthcare, Princeton, New Jersey) injected into an antecubital vein at a flow rate of 5 to 6 ml/s, followed by a mixed 50% contrast or saline injection and then a 20- to 30-ml saline chaser bolus. Iohexol dose was calculated according to the following formula: (predicted scan time in seconds + 5) × intravenous contrast flow rate. Both modes of scans were performed at 120 kV with a slice collimation of 128 × 0.625 mm with a dynamic dual focal spot (therefore 256-slice acquisition) and a rotation time of 0.27 or 0.33 seconds. The helical scans (retrospective ECG gating) were performed with an effective tube current (rotation time product normalized by the pitch) in the range of 900 to 1500 mAs (eff) depending on body mass index and body habitus, and a pitch of 0.14 to 0.2. ECG-based tube-current modulation was used when appropriate. The prospectively triggered scans were performed in patients with stable heart rhythm and heart rate <65 beats/min with a tube current–x-ray ON time product of 160 to 300 mAs. Radiation exposure was assessed as dose–length product (product of scan length and CT dose index). Reconstruction was performed using a window centered at 75% of the R-R interval as default. For heart rates >70 beats/min an earlier reconstruction phase (usually ≤45%) was frequently used with retrospective gating.
Two expert readers (>10 years of experience each in CCTA; standard reading) blinded to COMP-DIAG results diagnosed and reported significant coronary stenosis (OBS-CAD) (>50% diameter stenosis, ≥1 vessel) by consensus.
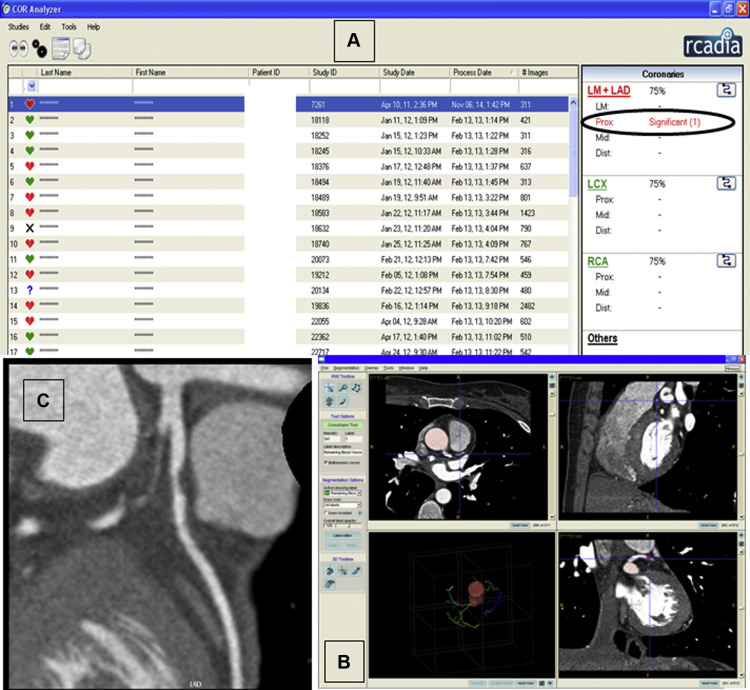
The CorAnalyzer II tool (Rcadia Medical Imaging, Haifa, Israel) was used for COMP-DIAG. This system installed in a standard workstation classifies the coronary artery system into 3 main arteries and 10 coronary segments: the left main coronary artery is presented together with the left anterior descending artery (the left anterior descending artery itself is divided to proximal, middle, and distal segments), the left circumflex, and the right coronary arteries are divided into 3 segments (proximal, middle and distal). Each artery is classified by the software to 1 of 3 categories: potentially stenotic (≥50% diameter stenosis), without significant stenosis (<50%), or indecisive (expert reading required). The latter would usually be reported by the system in the case of an unassessable segment.
Baseline characteristics and imaging and scanning parameters were recorded using descriptive statistics. Performance characteristics (patient-based and vessel-based) were calculated using CCTA expert reading results as the reference standard. A p value of <0.05 was considered significant. Statistical analysis was performed using Statistix 8 software package (Analytical Software, Tallahassee, Florida).
Results
Three hundred sixty-nine patients in ED with chest pain and without previously known CAD were originally included. However, 17 of 369 studies (5%) were unassessable by the automated COMP-DIAG and were excluded from analysis. Three hundred fifty-two patients (352 × 3 = 1,056 vessels) were therefore available for comparative analysis. Demographic data of the 352 patients are presented in Table 1 . CCTA imaging parameters are presented in Table 2 .
| Age (years) | ±SD | 55.5 ± 12.5 |
| Range | 17-89 | |
| Men | 208 (59%) | |
| Women | 41% | |
| Smoker | 33% | |
| Diabetes mellitus | 21% | |
| Hyperlipidemia ∗ | 50% | |
| Hypertension † | 54% | |
| Family history of coronary artery disease | 19% | |
∗ Total serum cholesterol level>5 mmol/l or treatment with lipid lowering drugs.
† Systemic blood pressure>140/90 or treatment with antihypertensive medication.
| Heart rate (BPM) (mean ± SD) | 63 ± 10 |
| Volume of IV contrast (ml) (mean ± SD) | 73.5 ± 10 |
| Dose length product (total) (mGy x cm) (mean ± SD) | 955 ± 695 |
| Dose length product of CTA (mGy x cm) (mean ± SD) | 713 ± 629 |
| Step & Shoot mode (percent) | 97/333 (29%) |
Expert reading of CCTA, which served as the reference standard diagnosed OBS-CAD in 107 of 1,056 vessels (10%) among 66 of 352 (18%) of the patients.
By COMP-DIAG, OBS-CAD was diagnosed in 301 of 1,056 vessels (28%) in 116 of 352 patients (33%).
Using expert reading as the reference standard, the sensitivity of COMP-DIAG to diagnose OBS-CAD was 93% (95% confidence interval [CI] 87 to 99) as 5 patients were incorrectly classified by the software as not having obstructive lesions. One hundred twenty-three patients were misclassified as having OBS-CAD by COMP-DIAG (false positive). Therefore, specificity was 56% (95% CI 50 to 62; Table 3 ).
| Analysis | N | Obstructive coronary disease by COMP-DIAG | Obstructive coronary disease by expert reading | Sensitivity (%, 95% CI) | Specificity (%, 95% CI) | PPV (%, 95% CI) | NPV (%, 95% CI) |
|---|---|---|---|---|---|---|---|
| Patient based | 352 | 116 (33%) | 66 (18%) | 93% (87-99) 66/71 | 56% (50-62) 158/281 | 35% (28-42) 66/189 | 97% (94-100) 158/163 |
| Vessel based | 1056 | 301 (28%) | 107 (10%) | 80% (73-88) 86/107 | 77% (75-80) 734/949 | 29% (24-34) 86/301 | 97% (96-98) 734/755 |
As reported previously, expert reading diagnosed OBS-CAD in 107 of 1,056 (10%) vessels, but COMP-DIAG diagnosed 301 of 1,056 (28%) vessels as having OBS-CAD. Thus, 194 vessels were misclassified as having OBS-CAD (false positive), in addition to 21 vessels with OBS-CAD misclassified as nonobstructive (false negative). Therefore, on a vessel-based analysis, the sensitivity of COMP-DIAG to diagnose OBS-CAD was 80% (73% to 88%) and specificity was 77% (75% to 80%; Table 3 ). An example of a true-positive case is presented in Figure 1 . Of note, no significant differences in terms of diagnostic accuracy were apparent among the 3 coronary vessels reported by the system (LM-LAD/LCX/RCA).