106 On its way from the sinus node to the ventricles, an electrical impulse passes through the atrioventricular (AV) conduction system comprising atrial myocardium, the AV node, the penetrating AV bundle (bundle of His), and the network of Purkinje fibers. Regular cardiac function requires some AV conduction delay to allow the ventricles to relax before the next atrial contraction. AV block is defined as further delay or block of impulse transmission that occurs mostly in the AV node. The AV node forms a heterogeneous and highly complex three-dimensional lattice of distinct cell types with different molecular make-up and therefore different functional behavior (Figure 106-1). Large atrial cells connect to midsized transitional cells, which, in turn, contact the small, closely packed cells of the compact node. It must be emphasized that the compact part represents one component of the AV node, which comprises all the different cell groups that determine its functional properties. Figure 106-1 Diagram Illustrating Anatomical, Histo-molecular, and Electrical Complexity of the Human AV Node in Relation to AV Block Many morphologic and functional factors like action potential characteristics, cell-to-cell coupling, and autonomic innervation determine impulse transmission and control AV conduction (see the previous chapter in this textbook1). Numerous pathologic processes, congenital or acquired, can affect this delicate system. AV block can be defined anatomically—supra- (i.e., atrial or AV nodal), intra-, or infra-His (see Figure 106-1)2—or electrocardiographically—first-, second-, and third-degree (complete) AV block. Thorough analysis of the electrocardiogram (ECG) can provide an estimation of the anatomical site of the block. If ventricular depolarization is undisturbed and QRS complexes appear normal, the site of delay or block is usually supra-His (usually AV nodal). Variations of the PR interval point to the AV node as the source of delay and block. When abnormal ventricular depolarization with prolonged QRS duration or left or right bundle branch block is present, the AV node can still be the substrate, but involvement of the His-Purkinje system distal to the AV node is likely. The site of conduction delay can be determined more precisely by endocardial recordings of AH and HV intervals. If impulse transmission is impaired in the atrium or in the AV node, the AH interval will be prolonged (>125 ms) and the HV interval will be normal (see Figure 106-1). A prolonged HV interval (>55 ms) indicates conduction disturbances in the His-Purkinje system (see Figure 106-1). Supra-His AV conduction delay or block usually has a favorable prognosis, whereas intra- or infra-His AV conduction delay or block implies a more serious prognosis.2,3 In the next section, a description of each specific AV block will be combined with data concerning incidence, prognosis, and treatment. On the surface ECG, the PR interval is measured from the onset of atrial depolarization (P wave) to the beginning of ventricular depolarization (QRS complex) and ranges normally between 0.12 and 0.20 seconds. In first-degree AV block, every non-premature atrial impulse is conducted to the ventricles with a PR interval that exceeds 0.20 seconds. The incidence of first-degree AV block in asymptomatic subjects is low, ranging between 0.5% and 1.6%.4,5 The prognosis for PR prolongation in the presence of a normal QRS complex until recently was thought to be benign. However, an observation from the Framingham Heart Study showed increased risk of development of atrial fibrillation (hazard ratio [HR], 2.06) and of pacemaker implantation (HR, 2.89) and revealed a moderately increased risk of death with a hazard ratio of 1.4.5 Electrocardiographically, typical type 1 block is characterized by several features: (1) progressive prolongation of the PR intervals, (2) the greatest increase in PR interval noted in the second beat of a cycle, with the increment being progressively less in subsequent beats, (3) gradual shortening of RR intervals, (4) a P wave not followed by a QRS complex, (5) a pause with an RR interval less than the sum of two PP intervals, and (6) the first conducted atrial impulse after the pause showing a shorter or normal PR interval (Figure 106-2). Clinically, only a minor part of type 1 second-degree AV block complies with all criteria.3 Figure 106-2 ECG Recordings from type I and type II Second-Degree AV Block Progressive (beat-to-beat) slowing of conduction velocity during a fast atrial rate, referred to as decremental conduction, can be attributed to the AV node and its atrial nodal extensions.1 Therefore, in type 1 second-degree AV block with normal QRS complexes, conduction delay and block occur most often within the AV node proximal to the His bundle. Type 1 block can occur in 1% to 2% of healthy individuals as a result of enhanced efferent discharge of parasympathetic nerve fibers. This vagally mediated block, in combination with slowing of the sinus rate, can occur in normal persons, for instance, as a result of pain or during sleep, or in persons with high vagal tone, like endurance athletes at rest.6 It is functionally determined and usually benign and disappears with increased sympathetic tone. Syncope is rare, although it sometimes can lead to serious symptoms in athletes and can necessitate de-training. In asymptomatic individuals without evident infra-nodal conduction disturbances, permanent pacemaker implantation is not recommended (class III).2 Progression to so-called advanced second-degree AV block or third-degree AV block is uncommon. If patients develop symptomatic bradycardia, permanent pacemaker implantation is indicated.2 Implantation of a permanent pacemaker is recommended for patients with type 2 second-degree AV block and should be considered also in asymptomatic patients. An electrophysiological study can sometimes be useful for determining intra- or infra-His levels of block. Type 2 second-degree AV block during exercise in the absence of ischemia indicates a diseased His-Purkinje system and should lead to permanent pacemaker implantation.2
Atrioventricular Block
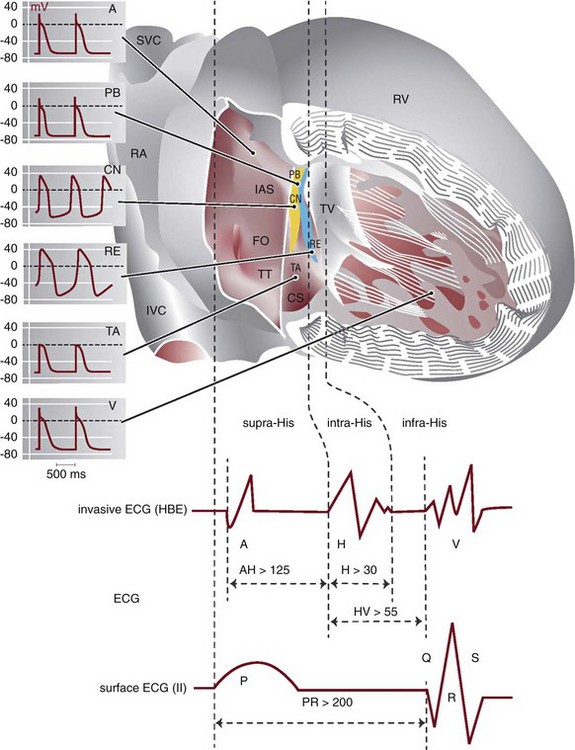
Anteriorly, the AV node is bordered by the tricuspid valve (TV), and posteriorly by the tendon of Todaro (TT). Histo-morphologically, the AV node is composed of a transitional area (TA), left inferior (LE) and right inferior extensions (RE), and the compact node (CN), which connects to the penetrating bundle of His (PB); yellow region, Cx43-negative; blue region, Cx43-positive. Calculated action potentials (APs) derived by mathematic modeling of mRNA expression data. Supra-His AV block if AH >125 ms; intra-His AV block if H >30 ms; infra-His block if HV >55 ms. CS, Coronary sinus; FO, foramen ovale; IAS, interatrial septum; IVC, inferior vena cava; RA, right atrium; RV, right ventricle; SVC, superior vena cava.
(Data from Kurian T, Ambrosi C, Hucker W, et al: Anatomy and electrophysiology of the human AV node. Pacing Clin Electrophysiol 33:754-762, 2010.)
(APs reproduced with permission of Dobrzynski H, Monfredi O, Greener ID, et al: Molecular basis of the electrical activity of the atrioventricular junction and Purkinje fibres. In Tripathi ON, Ravens U, Sanguinetti M [eds]: Heart Rate and Rhythm. Berlin, Heidelberg, Springer-Verlag, 2011.)
Electrocardiographic Characteristics and Definitions of AV Block
First-Degree AV Block
Second-Degree AV Block
Type 1 Second-Degree AV Block
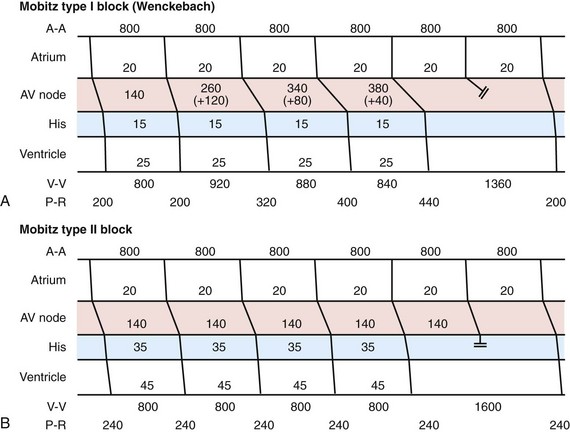
In Mobitz type I or Wenckebach block (panel A), progressive delay of the atrial impulse occurs in the AV node proximal to the His bundle. The greatest increment occurs in the second beat (+120 ms) and becomes less in subsequent beats (+80 ms, +40 ms), leading to gradual shortening of the RR interval (920 ms − 880 ms − 840 ms). The pause measures less than the sum of two PP intervals (1360 ms). Mobitz type II AV block (panel B) is not preceded by PR interval lengthening, and the pause equals two PP intervals. The site of block is usually distal to the AV node. Activation times in the diagrams are given in milliseconds (ms); double bars indicate conduction block. A, Atrium; V, ventricle.
Type 2 Second-Degree AV Block
Atrioventricular Block



