ATLAS OF PERCUTANEOUS REVASCULARIZATION
Percutaneous coronary intervention (PCI) is the most widely employed coronary revascularization procedure worldwide (Chap. 36). It is now applied to patients with stable angina, acute coronary syndromes, including unstable angina and non-ST-segment elevation myocardial infarction (NSTEMI), and as a primary treatment strategy in patients with ST-segment elevation myocardial infarction (STEMI). PCI is also applicable to patients with either single- or multivessel disease.
In this chapter, the use of PCI will be illustrated in a variety of commonly encountered clinical and anatomic situations such as chronic total occlusion of a coronary artery, bifurcation disease, acute STEMI, saphenous vein graft disease, left main coronary artery disease, multivessel disease, and stent thrombosis. In addition, the use of interventional techniques to treat structural heart disease will be shown, including closure of an atrial septal defect (ASD) and percutaneous aortic valve implantation; the latter is approved in Europe but is under active investigation in clinical trials in the United States and not yet approved for use.
CASE 1: CHRONIC TOTAL OCCLUSION
(Videos 44-1 to 44-7 can be accessed at the following link: http://www.mhprofessional.com/mediacenter/)
• An 81-year-old man with angina, NYHA class IV congestive heart failure and inferior-apical-posterior ischemia on an exercise technetium-99m scan.
• Diagnostic cardiac catheterization revealed a left dominant system with a totally occluded left circumflex (LCx) artery. The distal LCx filled via collaterals from the left anterior descending (LAD) artery, indicating chronicity of the total occlusion.
Video 44-1 Baseline left coronary angiogram shows an occluded LCx with left-to-left collaterals originating from LAD septal vessels.
Video 44-2 Attempts to cross the total occlusion in the LCx using a hydrophilic wire and an antegrade approach were not successful, with the wire tracking to the right of the trajectory.
Video 44-3 The LAD septal collateral is accessed with a guidewire and directed toward the distal LCx to cross the total occlusion retrograde.
Video 44-4 The total occlusion is crossed retrograde. The wire is snared in the guide, exteriorized, and used to provide antegrade access to the LCx.
Video 44-5 Antegrade flow in the LCx is restored after balloon inflation.
Video 44-6 Following stenting of the total occlusion, blood flow in the distal vessel is improved and a second significant stenosis is seen.
Video 44-7 Final result after LCx stenting.
SUMMARY
• Approximately 15–30% of all patients referred for cardiac catheterization will have a chronic total occlusion (CTO) of a coronary artery.
• CTO often leads to a surgical referral for complete revascularization.
• Incomplete revascularization due to an untreated CTO is associated with an increased mortality rate (Hazard Ratio = 1.36, 95% CI = 1.12–1.66, p < 0.05).
• Successful PCI of a CTO leads to a 3.8–8.4% absolute reduction in mortality, symptom relief, and improved left ventricular function.
• Newer techniques, such as the retrograde approach to crossing total occlusions, are useful when the antegrade approach fails, or is not feasible, and there are well-developed collateral vessels.
(Case contributed with permission by Dr. Frederick G. P. Welt.)
CASE 2: BIFURCATION STENTING
(Fig. 44-1; Videos 44-8 to 44-16 can be accessed at the following link: http://www.mhprofessional.com/mediacenter/)
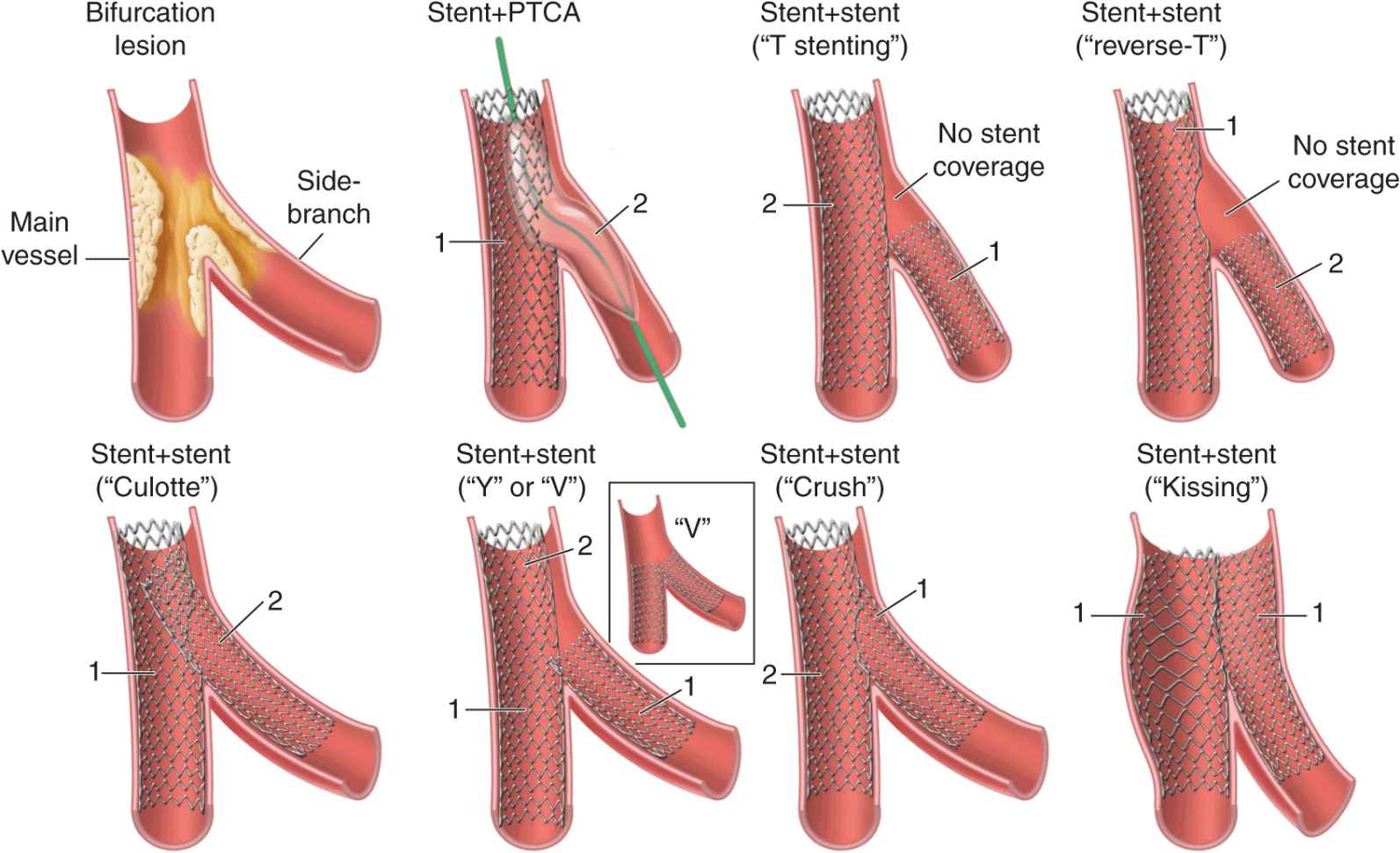
FIGURE 44-1
Schematic representation of 1-stent and 2-stent techniques to treat bifurcation lesions. PTCA, Percutaneous transluminal coronary angioplasty. (Reprinted with permission from SK Sharma, A Kini: Cardiol Clin 24:233, 2006.)
• A 52-year-old man with an acute coronary syndrome and a troponin I = 0.18 (upper limit normal ≥ 0.04).
• Diagnostic cardiac catheterization showed single-vessel coronary artery disease with a significant stenosis in the mid-LAD and a bifurcation lesion involving a large diagonal branch.
Video 44-8 Baseline angiogram of the left coronary circulation shows the significant stenosis in the mid-LAD and the bifurcation lesion involving a large diagonal branch.
Video 44-9 Both vessels are accessed with guidewires and pretreated with balloon angioplasty.
Video 44-10 Result after balloon angioplasty.
Video 44-11 Stent being positioned in the LAD.
Video 44-12 LAD post-stent result.
Video 44-13 Stent deployed in diagonal branch through the stent struts in the LAD using the “culotte” technique.
Video 44-14 Diagonal branch post-stent result.
Video 44-15 Simultaneous inflation of two 2.5-mm “kissing” balloons.
Video 44-16 Final postbifurcation stenting result.
SUMMARY
• Approximately 15–20% of PCIs will involve the treatment of bifurcation lesions.
• Bifurcation lesions require consideration of PCI strategies that protect side-branch patency.
• There are both one-stent and two-stent techniques to treat bifurcation lesions; the selection of technique depends upon anatomic considerations, including plaque burden, angle of side-branch take-off, plaque shift during angioplasty, and side-branch distribution.
• Rates of target lesion revascularization and stent thrombosis are similar between one-stent and two-stent procedures.
CASE 3: INFERIOR MYOCARDIAL INFARCTION—THROMBUS AND MANUAL THROMBECTOMY
(Figs. 44-2 to 44-4; Videos 44-17 to 44-22 can be accessed at the following link: http://www.mhprofessional.com/mediacenter/)
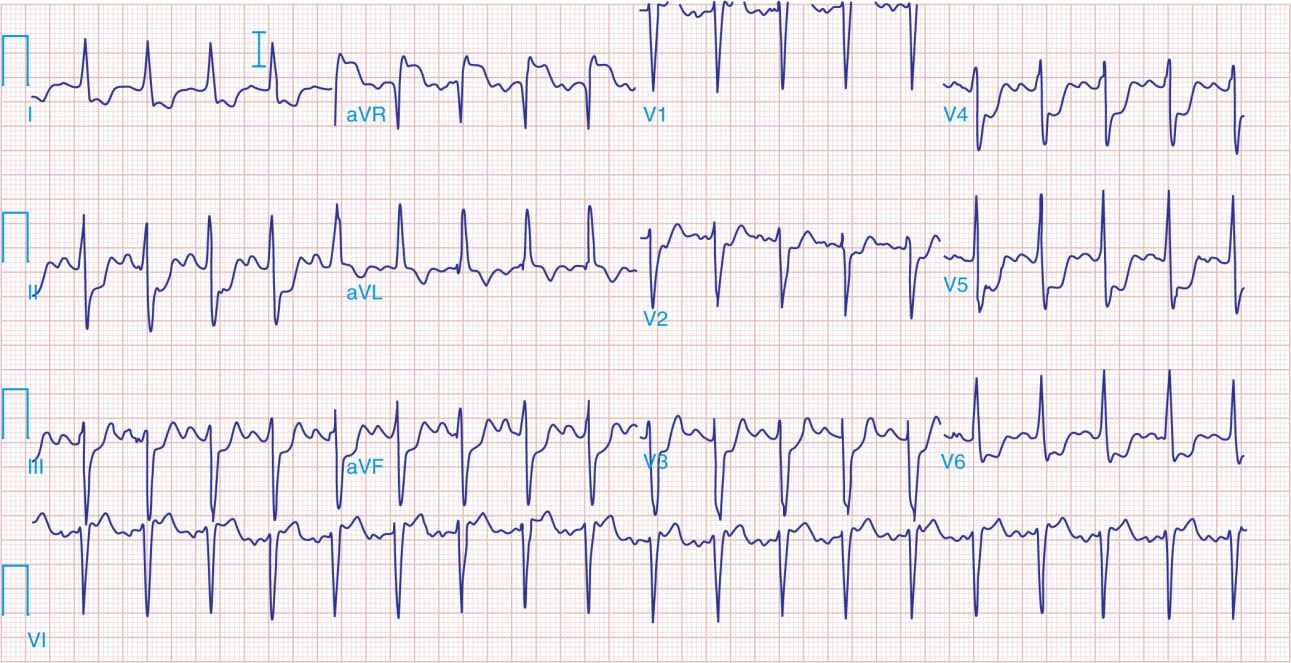
FIGURE 44-2
Preprocedure ECG showing inferior ST-segment elevations and lateral ST-segment depressions.
FIGURE 44-3
Example of an organized red thrombus retrieved by manual thrombectomy. (Reprinted with permission from C Trani et al: J Invasive Cardiol 19:E317, 2007.)
FIGURE 44-4
Postprocedure ECG showing resolution of ST-segment elevations.
• A 59-year-old man presented to the emergency room with 2 h of severe midsternal chest pressure.
• His systolic blood pressure was 100 mmHg and he was tachycardic in sinus rhythm with a heart rate of 90–100 bpm.
• His initial ECG showed inferior ST-segment elevations with lateral ST-segment depressions.
• He was referred emergently to the cardiac catheterization laboratory for primary PCI.
Video 44-17 The right coronary artery (RCA) is totally occluded with filling defects in the vessel after contrast injection, indicating thrombus is present in the vessel.
Video 44-18 An angioplasty wire is threaded through the thrombotic lesion, but this does not restore blood flow to the distal vessel.
Video 44-19 Result after manual thrombectomy and thrombus extraction. The “culprit” ruptured plaque and residual thrombus are now apparent in the vessel.
Video 44-20 After balloon angioplasty and stenting, thrombus is still present.
Video 44-21 After repeat manual thrombectomy and expansion of the stent, the thrombus is no longer present.
Video 44-22 Final result.
SUMMARY
• An acute STEMI occurs following plaque rupture that promotes thrombotic occlusion of a coronary artery.
• Despite successful revascularization of the epicardial coronary artery, microemboli liberated during balloon angioplasty and stenting may lead to persistent micro-vascular dysfunction. When present, microvascular dysfunction is associated with a larger infarct size, heart failure, malignant ventricular arrhythmias, and death.
• Manual thrombectomy is used to aspirate or remove thrombus in the vessel and limit distal embolization during angioplasty and stenting.
• Manual thrombectomy in primary PCI is associated with improved myocardial perfusion and a reduction in mortality.
• Adjunctive antiplatelet and antithrombin agents are important to aid in the resolution of intracoronary thrombus.
CASE 4: SAPHENOUS VEIN GRAFT INTERVENTION WITH DISTAL PROTECTION
(Fig. 44-5; Videos 44-23 to 44-26 can be accessed at the following link: http://www.mhprofessional.com/mediacenter/)
FIGURE 44-5
Distal protection device showing captured atherosclerotic debris liberated by initial balloon dilation. (Reprinted with permission from RA Aqel et al: J Invasive Cardiol 19:E104, 2007.)
• A 62-year-old man with a history of chronic stable angina.
• A four-vessel coronary artery bypass grafting (CABG) surgery was performed 17 years earlier with a left internal mammary artery graft to the LAD, a right internal mammary artery graft to the RCA, a saphenous vein graft to the first obtuse marginal branch, and a saphenous vein graft to the first diagonal branch.
• The patient had a recent increase in angina with exertion and was found to have lateral ischemia on an exercise technetium-99m scan.
• Diagnostic cardiac catheterization revealed a significant stenosis in the body of the saphenous vein graft to the first obtuse marginal branch.
Video 44-23 Saphenous vein graft to a first obtuse marginal branch with an 80% eccentric stenosis in the midgraft.
Video 44-24 A distal protection device is deployed past the lesion.
Video 44-25 Angioplasty balloon inflation with the distal protection device in place.
Video 44-26 Final result after stent placement.
SUMMARY
• Saphenous vein grafts have a failure rate of up to 20% after 1 year and as high as 50% by 5 years.
• Graft failure (>1 month) results from intimal hyperplasia and atherosclerosis.
• Saphenous vein graft PCI is associated with distal embolization of atherosclerotic debris and micro-thrombi, leading to microvascular occlusion, reduced antegrade blood flow (the “no-reflow” phenomenon), and myocardial infarction.
• Embolic distal protection devices decrease the risk of distal embolization, as well as the incidence of no-reflow and myocardial infarction associated with saphenous vein graft interventions.
CASE 5: UNPROTECTED LEFT MAIN PCI IN A HIGH-RISK PATIENT
(Figs. 44-6 and 44-7; Videos 44-27 to 44-34 can be accessed at the following link: http://www.mhprofessional.com/mediacenter/)
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree