Chapter 164
Atheromatous Embolization
Jeffrey W. Olin, John R. Bartholomew
Atheromatous embolization is a poorly recognized and underdiagnosed multisystem disorder that is associated with high risk of all-cause and cardiovascular mortality.1 There are a myriad of clinical manifestations that may occur across all specialties, making differential diagnoses broad and diagnosis difficult. In addition, atheromatous embolization is a confusing entity to many physicians because it is known by many different names: cholesterol embolization, cholesterol crystal embolization, blue toe syndrome, purple toe syndrome, atheroembolism, and pseudovasculitis. For the purposes of this chapter, these terms will be used interchangeably. Once atheroembolism occurs, therapy involves three major strategies: treat the end organ that is undergoing embolization, prevent further embolization from occurring, and prevent future cardiovascular morbidity and mortality. Therefore, it is critical for clinicians to have a high index of suspicion and to recognize the clinical manifestations of this syndrome.
Incidence
The incidence of cholesterol embolism syndrome varies based on population characteristics, diagnostic criteria, and study design. Among unselected series of autopsy studies, the incidence of cholesterol crystal embolism ranges from 0.18% to 2.4%.2 However, autopsy studies performed in selected populations with atherosclerosis and in those who have undergone aortic manipulation have reported a greater prevalence of cholesterol crystal embolism, ranging from 12% to 77%.3,4 In autopsy studies of patients with known advanced atherosclerosis who recently had an arteriogram or a cardiac or vascular surgical procedure, the incidence is also high.5 Blauth et al5 identified atheroemboli in 22% of their postcardiac surgery autopsy cases, whereas Ramirez et al6 reported a 27% incidence in patients who had arteriography performed before their deaths. In general, retrospective autopsy studies may overestimate the frequency of the disease because of the detection of subclinical cases and the selection bias inherent in obtaining information after necropsy. In contrast, clinically significant atheroembolic disease in clinical studies may be missed because of short-term follow-up. The prevalence of atheroembolic disease in clinical studies has been estimated to be between 1% and 4%.7–11 There are two factors that may be associated with either an increased prevalence of atheromatous embolization (the continuing increasing age of the population, and thus, more advanced atherosclerosis) or a decreased prevalence (better guide wires, catheters, and endovascular and surgical techniques). However, there have been no recent studies on current prevalence rates.
Pathogenesis
The first description of atheroembolism was published more than a century ago by the German pathologist, Panum.12 However, Flory13 is credited for accurately describing the syndrome in 1945. Among 267 consecutive autopsies, he observed 9 instances of cholesterol crystal embolism: none in 63 cases in which aortic plaque ulceration was absent; 2 instances in 147 (1.4%) cases with moderate aortic plaque erosion; and 7 instances in 57 (12.8%) cases with severe aortic plaque ulceration. Since that seminal paper, it has become quite clear that the risk of atheroembolism is directly related to the severity of aortic atherosclerosis.
Atherosclerotic plaques consist of a fibrous cap, under which are macrophages, necrotic debris, and cholesterol crystals. The vulnerable plaque, or the plaque at the highest risk of rupture, are those with a thin fibrous cap surrounding a large lipid-rich core.14 Kronzon and Saric15 have stated that there are six key elements required for the development of “cholesterol embolization syndrome”: (1) plaque in large arteries, such as the aorta, iliac, or carotid arteries; (2) spontaneous, traumatic, or iatrogenic plaque rupture; (3) embolization of cholesterol crystals, platelets, fibrin, and other detritus; (4) lodging of emboli in small arteries with a diameter of 100 to 200 µm, leading to occlusion of vessels; (5) foreign body inflammatory response to the atheromatous emboli; and (6) end organ damage to physical and inflammatory occlusion of multiple small arteries. Cholesterol crystals are white and rhomboidal or rectangular in shape. They can also be elongated, biconvex, and needle-shaped, and range in size from 250 µm to less than 10 µm in diameter.8 The cholesterol crystals dissolve in paraffin-fixed sections, leaving needle-like clefts (Fig. 164-1). Frozen or wet formalin-fixed sections reveal doubly refractile cholesterol crystals; with the Schultz histochemical stain, these crystals stain blue-green.16
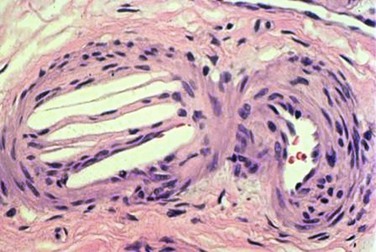
Figure 164-1 Typical appearance of the cholesterol clefts in a specimen from a kidney biopsy. The convex-shaped crystals within the small arterioles of the kidney dissolve during the fixation process leaving the ghosts (left side), which is what is seen in the histopathology (hematoxlyin & eosin stain, 200 times original magnification). Note the three red blood cells in the arteriole (right side).
Because they are light in weight and hydrophobic, they pass quickly through blood vessels until they are stopped by arterial bifurcations, a narrowing of the vessel lumen, or when they reach the end of the arterial circulation.8 Cholesterol emboli tend to be diffuse and lodge in arteries 100 to 200 µm in size,10 although small crystals have been observed in capillaries in the end-arterial circulation.
Cholesterol crystals that lodge in the arterioles immediately incite an inflammatory response characterized by varying degrees of polymorphonuclear and eosinophilic infiltration.8,13,17,18 By 2 to 4 weeks, a more chronic inflammatory infiltrate is seen. Cholesterol crystals become embedded in multinucleated giant cells and smooth muscle cells.17 Endothelial proliferation and fibrous tissue can be found surrounding the crystals, ultimately leading to luminal obliteration.17,18 At 1 to 2 months, crystals may extrude out of the vessel lumen and be buried in the adventitia, or remain in the lumen, embedded within organized thrombus that may re-canalize.17 The crystals are resistant to breakdown by macrophages and have been shown to persist in tissue for up to 9 months.19,20 Arterial lumina are eventually occluded by the accumulation of cells and fibrous material. These pathologic changes result in tissue effects distal to the cholesterol crystal emboli, including ischemia, and rarely, infarction, depending on the extent of organ involvement. This type of foreign body reaction is the reason it may take weeks to months for serum creatinine to rise in patients with atheroembolic renal disease and illustrates why renal function does not usually recover.19,21–23
Risk Factors and Simple Preventive Strategies
The most important risk factor for atheroembolism is established atherosclerosis. In 1945, Flory13 was the first person to hypothesize such a relationship between cholesterol crystal embolism and a diseased atherosclerotic aorta. Forty-seven years later, Blauth et al5 reported on 46 patient autopsies in which severe atherosclerosis of the ascending aorta was accompanied by evidence of atheroemboli in other vascular beds. Significant risk factors for atheroembolism included peripheral arterial disease, hypertension, older age, and coronary artery disease.5
There are several precipitating factors that have been implicated in the occurrence of plaque instability and consequent atheroembolism, including trauma, vascular surgery,24,25 angiographic and endovascular procedures,1,19,22,26 anticoagulation,7,27,28 and thrombolysis.29–32 Although spontaneous atheroembolism was once the most common presentation of atheromatous embolization, endovascular revascularization techniques are now the most frequent precipitating cause of the atheromatous embolization syndrome.21,22,33–35 In 354 patients who were followed for an average of 2 years, Scolari et al22 found that atheroembolic disease was spontaneous in only 23.5% of cases.
Coronary Interventions
Manipulation of the aorta with catheters or guide wires can cause mechanical trauma, consequently dislodging atheromatous material from the arterial wall.36 One study that evaluated the frequency of atherothrombotic material retrieved during placement of coronary catheters found 0.5% of 7621 patients had macroscopically visible atherothrombotic debris.37 None of these patients, however, had clinically apparent atheroembolic disease. In a review of 4587 cardiac catheterizations, Drost et al38 found 7 cases of clinical cholesterol embolization (0.002%). Colt et al39 found 8 cases after heart catheterization, percutaneous transluminal coronary angioplasty, and intra-aortic balloon pump insertion involving 3733 procedures (0.002%). Coronary angiography with angioplasty and stenting is considered the most common arteriographic procedure to incite atheroembolism.10,22 Saklayen et al,40 in a prospective analysis of 267 patients who underwent coronary angiography, found the incidence of cholesterol embolism to be less than 2%. Similar statistics were found in a more recent prospective analysis by Fukumoto et al,41 who reported the occurrence of clinically apparent cholesterol embolism (livedo pattern on the feet, blue toe syndrome, digital gangrene, or renal failure) in 1.4% of 1786 patients who underwent left heart catheterization.
Although it is impossible to predict the risk of atheroembolism in a given patient, the presence of severe peripheral artery disease, aortic aneurysm, and protruding mobile atheroma by transesophageal echocardiography (TEE),42 or aortic plaque more than 4 mm in thickness43 increase the risk of distal embolization and should therefore influence the vascular approach.40,44 Utilization of long guide wire (260 cm) exchanges is recommended, and back bleeding from guiding catheters (once the wire is removed) allows for removal of debris. Advancement and removal of catheters should occur over a guide wire to straighten the catheter and minimize contact with the aortic wall. Brachial and radial access may minimize embolization from the abdominal aorta, but not from the ascending aorta or arch. However, a prospective study of 1579 patients who underwent coronary angioplasty did not find significant differences between the brachial and femoral approaches.45 In contrast, in another study that involved 3733 procedures, there were no cases of cholesterol embolization after cardiac catheterization when the brachial artery was used.39
Aortography
Catheter manipulation of the aorta is frequent in the diagnosis and evaluation of patients with vascular disease before revascularization, and as with coronary angiography, the risk of atheroembolism is a serious concern. Ramirez et al,6 in a retrospective study of 71 autopsy cases, reported a 27% incidence of cholesterol embolization in patients who had arteriography performed compared with a 4.3% incidence of spontaneous cholesterol emboli in an age- and disease-matched control group who did not undergo arteriography.6 The rigidity of the catheter used and the force of the contrast injection appeared to contribute to the risk of embolization. Although some have advocated the use of a softer, more flexible catheter to avoid such a complication,6 the most important factor determining risk remains the severity of the atherosclerotic disease in the aorta. It should be understood, however, that the studies that reported a significant incidence of cholesterol embolization after angiography were conducted nearly 25 years ago. With the advent of better, smaller and more flexible catheters, guide wires and balloons, as well as superior operator technique and the use of the “no touch” technique,46 the incidence of atheromatous embolization following angiography is much less than it was 3 decades ago.
Endovascular Therapy
Endovascular therapy for patients with peripheral vascular disease has become widely utilized as an alternative to surgical revascularization. Clinically important atheroembolism appears to be a relatively infrequent, but not absent, complication of endovascular therapy. In a retrospective analysis of 493 patients who underwent a total of 565 aortoiliac stent placements, Lin et al47 found the incidence of atheroembolism to be 1.6%. This percentage is comparable to the findings of previous clinical studies that noted that atheroembolism ranged between 1.3% and 3.6%.48,49 In a study that utilized duplex ultrasound at the time of renal artery stenting, microembolic signals were detected in the renal parenchyma in every single case.1,50 In addition, when emboli protection devices were utilized in carotid stent procedures51 or renal artery stent procedures,52–58 visible atherosclerotic debris was frequently retrieved. Several studies showed that distal protection devices used at the time of renal artery stenting were associated with less deterioration in renal function compared with stenting without the use of these devices (Fig. 164-2).53–55 In a small prospective randomized trial, Cooper et al54 demonstrated that during renal artery stenting, the combination of distal embolic protection and the use of the glycoprotein IIb/IIIa inhibitor abciximab resulted in an improvement in renal function compared with the use of either of these modalities alone.54 Additionally, Paul et al59 showed that there is a much greater improvement in renal blood flow (as measured by the renal frame count) when a distal protection device was used during renal artery stent implantation compared with renal artery stenting without a distal protection device. Although distal protection devices are routinely used in carotid artery stenting, this is not the case in renal artery stenting. In the initial design of the CORAL trial, a distal protection device was used in every patient who was randomized to stenting. However, due to slow recruitment, this requirement was dropped from the protocol, and the decision was left up to the discretion of the interventionalist.60

Figure 164-2 A, Catheter-based angiogram demonstrating a severely atherosclerotic aorta with a severe stenosis of the left renal artery and an occluded right renal artery (left panel). A selective angiogram of the left renal artery shows the severity of stenosis. B, There was a 7-mm Spider embolic protection device (arrow) (ev3 Endovascular, Inc., Plymouth, Minn.) placed before renal artery stenting (right panel).
The presence of a shaggy aorta and diffuse soft ulcerative plaque on TEE studies clearly identify a high-risk population.43 Hence, heightened awareness, proper patient selection, utilization of the most advanced catheters, guide wires, and balloons, use of emboli protection devices, and greater operator expertise may have a favorable impact on the incidence of atheroembolism during endovascular interventions. There are times in which endovascular procedures using covered stent grafts may be quite effective in patients who experience embolization, as is discussed in the Treatment section.
Vascular Surgery
The effect of atheroembolism after major vascular surgery was first recognized by Thurlbeck et al in 1957.61 In their series, atheroembolism was present at autopsy in more than 75% of the patients who died after aortic aneurysm surgery. Atheromatous embolization was the cause of death or significantly contributed to mortality in nearly half of the patients in this series. Subsequently, numerous studies confirmed the importance of vascular surgery as a precipitator of atheroembolism. Vascular surgery procedures may disrupt plaque when the vessel is manipulated, cross-clamped, or incised during surgery. Other vascular surgery procedures known to precipitate cholesterol embolization include aortoiliac and aortofemoral bypass, carotid endarterectomy, and renal artery revascularization.10 In a retrospective series of 1011 patients who underwent infrarenal aortic surgery or infrainguinal surgery, the diagnosis of cholesterol embolization was 2.9%.62 Due to the advent of better surgical techniques and an awareness of the risk of surgery precipitating atheromatous embolization, this complication has become much less common than reported in the older literature.63
Cardiac Surgery
Atheroembolization is a recognized complication of cardiac surgery and has profound medical and economic consequences. Doty et al,25 in a retrospective analysis of 18,402 patients who underwent cardiac surgery, found evidence of atheroembolism in 0.2% of patients at autopsy. The clinical presentation of atheroembolism in this study was broad and included five distinct organ systems: heart, central nervous system, gastrointestinal (GI) tract, kidneys, and the lower extremities. In 21% of these cases, death was directly attributable to atheroembolism.25 Kolh et al64 documented a significant increase in intensive care unit stay, overall hospital stay, and total hospital cost in patients with documented atheroembolism after cardiac surgery. TEE can identify significant aortic plaque preoperatively with sensitivity and specificity in excess of 90%.65 Multidetector computed tomographic (CT) angiography may also be a valuable imaging tool to image the aorta and iliac arteries. Alteration of the cannulation site and avoidance of aortic manipulation for coronary artery bypass based on such findings may reduce the incidence of atheroembolism.
It is clear that the most effective strategy for the management of atheroemboli in vascular surgery is prevention. In high-risk surgical patients, noninvasive procedures, such as magnetic resonance imaging, TEE, or CT angiography are excellent techniques to screen for the presence of aortic atherosclerosis preoperatively. When a severely atherosclerotic aorta is visualized, alternative surgical procedures should be considered to minimize aortic manipulation. Appropriate surgical techniques to prevent atheroemboli during operation are now well recognized and documented.63
Anticoagulation
An increased risk of cholesterol embolization with anticoagulation and clinical improvement when anticoagulation was removed has been reported in case reports for nearly half a century.7,10,27 One hypothesis is that anticoagulation may prevent thrombus formation over unstable atherosclerotic plaque, thus allowing exposed cholesterol crystals to embolize. Another hypothesis is that these agents may initiate the disruption of a complex plaque by causing intraplaque hemorrhage.66–69 Based on these small case series and case reports, some investigators have recommended that warfarin be discontinued, when feasible, in patients who have had an episode of cholesterol embolization for which no other precipitant can be identified.
However, the data are not entirely clear in assessing anticoagulation safety in patients with a large amount of aortic plaque. The assumption that anticoagulation precipitates cholesterol emboli syndrome was not confirmed by the SPAF-3 trial, in which patients with documented aortic plaque identified by TEE and who were assigned to adjusted-dose warfarin therapy had a low annual rate of cholesterol embolization (0.7% per patient-year; 95% confidence interval, 0.1%-5.3%).70 Furthermore, cholesterol embolization was not seen in patients with documented aortic arch plaque of more than 1 mm in thickness treated with warfarin in The French Study of Aortic Plaques in Stroke Group.43 In a prospective evaluation of 25 patients with cholesterol emboli syndrome after cardiac catheterization, Fukumoto et al41 failed to show any association between the use of anticoagulants and cholesterol embolism. In addition, anticoagulation has been advocated for patients with crescendo transient ischemic attacks (TIAs), a syndrome caused by athermatous embolization to the eye or brain.
Whether the use of anticoagulation is associated with a higher incidence of atheroemboli remains controversial, but the current literature suggests that it is safe to continue anticoagulation therapy in patients with a compelling reason to do so, such as those with atrial fibrillation or venous thromboembolism.
Thrombolysis
Atheromatous emboli have also been associated with thrombolytic therapy in case reports and small series,30,32 but again this is controversial. Thrombolytic agents act by converting plasminogen to plasmin; plasmin directly degrades fibrin. Theoretically, any therapy that causes the thrombus to undergo lysis may leave atherosclerotic plaque uncovered, placing the patient at risk for embolization. In one small prospective study, no relationship between the administration of thrombolytic therapy and cholesterol emboli syndrome was found.71
Clinical Features
Epidemiology
The syndrome of atheroembolism usually affects elderly persons who have multiple risk factors for atherosclerosis, but may occur in younger individuals with advanced atheroscleosis.2 In a recent prospective study to identify risk factors for cholesterol embolism in patients who underwent cardiac catheterization, Fukumoto et al41 confirmed that cholesterol emboli syndrome occurred more frequently in patients with generalized atherosclerosis (e.g., multivessel coronary disease, cerebrovascular disease). In addition, the authors found a significant relationship between C-reactive protein and cholesterol embolism (odds ratio 4.6; P = .01, using multivariate analysis), indicating an important possible association between systemic inflammation and cholesterol emboli syndrome.41
The increased frequency of this disease in men72 may be explained by a difference in the prevalence of atherosclerosis between the sexes. In addition, atheroemboli occurs almost exclusively in patients older than 50 years of age.72 A race predilection has also been reported, because atheroemboli are less likely to occur in African American patients (32 : 1 ratio).72,73 However, because African Americans appear to have an increased prevalence of atherosclerosis, it has been suggested by some investigators that this may be a failure to recognize the classic features of this syndrome because of skin pigmentation and the propensity of African American patients to develop renal failure secondary to poorly controlled blood pressure.
Clinical Findings
Patients almost always have symptomatic atherosclerosis manifested clinically by angina, myocardial infarction, TIA, stroke, renal artery disease, mesenteric ischemia, or peripheral arterial disease and claudication.74 Atheroembolism can present with a myriad of symptoms (Box 164-1).75–77 In general, the organs affected by cholesterol embolism depend on the location of the embolic source. Atheroemboli from the ascending aorta and proximal aortic arch usually manifest with central nervous system or retinal pathology, whereas cholesterol crystal emboli originating from the descending thoracic or abdominal aortas affect the visceral organs and extremities. In general, bilateral lower extremity atheroembolism signifies a source proximal to the aortic bifurcation, whereas unilateral emboli may originate either proximally or in any artery distal to the aortic bifurcation. Patients with one or more large atheromatous plaques in the aorta may present with a catastrophic event, such as an acutely ischemic limb, or renal or mesenteric infarction.33,78 Conversely, patients with microemboli may have milder localized signs or a clinical picture that suggests a systemic illness. There may be a temporal delay in clinical findings (especially for renal failure) after the inciting event of up to 8 weeks.76
Cutaneous Manifestations
Skin manifestations are among the most common clinical manifestations of atheroembolism, and the common cutaneous features are livedo reticularis and blue toes.79,80 The appearance of cutaneous signs can be delayed, with 50% of patients in one series showing skin signs of atheroembolism more than 30 days after their procedure or other inciting event.79
Livedo Reticularis.
Livedo reticularis is a blue-red mottling or discoloration of the skin that occurs in a netlike pattern, most commonly seen on the buttocks, thighs, or legs (Fig. 164-3A). A detailed skin examination performed in both the supine and upright posture is necessary because livedo reticularis has been shown to be more readily demonstrable in the upright position.81 Livedo reticularis is caused by obstruction of small arteries, capillaries, or venules in the deep dermis.10,22 When the skin is biopsied in patients with atheromatous embolization, cholesterol crystals may be seen in the dermal blood vessels. Livedo reticularis, however, is not pathognomonic of atheroemboli and has an extensive differential diagnosis including, but not limited to, other causes of intravascular obstruction (i.e., antiphospholipid antibody syndrome, cryoglobulinemia, endocarditis, left atrial myxoma), vasculitis, or be drug-induced (i.e., quinidine, quinine, amantidine, catecholamines).82 Furthermore, there are also physiologic (Cutis marmorata) and idiopathic (livedoid vasculitis) forms of livedo reticularis. Livedo can occur in young healthy women and appears to be related to abnormal sensitivity of the dermal blood vessels to cold (primary livedo reticularis). This livedo reticularis pattern usually disappears on re-warming. Patients who exhibit this should be reassured that there is no serious circulatory abnormality present.


Figure 164-3 A, Characteristic appearance of the foot in a patient with atheromatous embolization. There is a patchy distribution of livedo reticularis on the lateral aspect, plantar surface, and heel of the right foot. Note the purple second toe. B, Typical appearance of blue or purple toes that may occur in atheromatous embolization. C, More severe cases may progress to gangrene.
Blue Toe Syndrome.
In its classic presentation, the blue toe syndrome presents as the sudden appearance of a cool, cyanotic, and painful toe in the presence of palpable distal pulses (Fig. 164-3B).66–68,79 Discoloration may also be seen on the sole of the foot. The discoloration may be patchy (see Fig. 164-3A), and comparison of both feet shows that the distribution is not symmetric. These lesions may progress to ulceration, necrosis, and frank gangrene (Fig. 164-3C).10 Accessory lesions may be present on the lateral and posterior aspects of the heels, which later develop into linear fissures with skin edge gangrene and a dark, necrotic base.
Other Skin Manifestations.
Other skin manifestations include splinter hemorrhages, petichiae, purpura, ulcers,83 and raised nodules that appear as the result of subepidermal inflammation surrounding cholesterol crystals,10,79 These nodules are painful, violaceous in appearance with a necrotic center, and may mimic a necrotizing vasculitits, such as polyarteritis nodosa or leukocytoclastic vasculitis. Ulceration of the penis and scrotum have also been described.84
Renal Involvement
The kidneys are a prime target for cholesterol crystal embolization due to the enormous amount of blood that flows through the kidney and the close proximity of the proximal renal arteries to the plaque-bearing abdominal aorta.21–23
Incidence.
Mayo et al,9 in a review of 402 nephrology consultation charts, found that the incidence of clinically detectable atheroembolism amounted to at least 4% of all inpatients examined, representing approximately 5% to 10% of the acute renal failure patients encountered. Scolari et al10 estimated encountering at least one case per month with atheroembolic renal disease. Since this report, these investigators have seen 354 patients who have been followed for an average of 2 years.22 Most investigators believe that this condition is significantly underdiagnosed.1,21,22
Pathology.
Pathologically, the classic lesion of atheroembolic renal disease is the occlusion of medium-sized arterioles (150-200 µm in diameter) and glomerular capillaries with cholesterol emboli.10 In addition to the ischemic obstructive mechanical phenomenon produced at the onset, this pathologic condition produces an inflammatory reaction within the arterioles. The initial stages, which occur several days to weeks after the inciting event, are characterized by an inflammatory infiltration consisting of polymorphonuclear leukocytes, macrophages, and multinucleated giant cells. Because the cellular infiltrate leads to thickening and fibrosis of the arterioles, later stages are characterized by glomerular sclerosis, tubular atrophy, and interstitial fibrosis.21,76,85 A kidney biopsy specimen from an individual patient may reveal different stages of histologic evolution because dislodged atheromatous debris may be showered into the circulation at different time intervals.85 Furthermore, the involvement tends to be patchy, and therefore, a renal biopsy may not always show the classic pathologic lesions of this disease.85
Clinical Features.
The net effects of this pathogenic process, when combined with varying amounts of cholesterol embolization, have several different clinical presentations (Fig. 164-4).10,21–23 It is important to recognize the differences in the patient with acute tubular necrosis (ATN) (Fig. 164-4A) from those with atheroembolic renal disease (Figs. 164-4B-D). Marked renal impairment with acute onset is the easiest form of atheroembolic renal disease to recognize. It has the closest temporal relationship to the inciting event and is generally considered the consequence of massive embolization, often resulting in catastrophic consequences. The subacute form of atheroembolic renal disease, the most frequently observed, is more insidious in onset, occurring a few weeks after the inciting event. Renal impairment may worsen over weeks to months due to an inflammatory response and foreign-body reaction, or the cyclic occurrence of cholesterol crystal embolic showers (Fig. 164-4B). Some patients with advanced renal failure come to the attention of physicians with few clues as to the exact onset of renal impairment. Under this circumstance, atheroembolic renal disease can only be diagnosed by performing a renal biopsy. Atheroembolic renal disease may also be present with chronic stable renal impairment (Fig. 164-4C) in an asymptomatic patient. Clinical features tend to be similar to those of ischemic nephropathy and nephrosclerosis. The role of cholesterol embolization in this setting is somewhat unclear. Many patients are misdiagnosed either because a renal biopsy is not performed or cholesterol embolization is missed on biopsy due the patchy distribution of the emboli. Recovery of dialysis-dependent renal failure (Fig. 164-4D) may occur in 21% to 39% of patients who initially require renal replacement therapy.23 Atheroembolic renal disease is often associated with severe and poorly controlled hypertension.68,76,86,87 When large segments of small arterioles are occluded, ischemic atrophy of substantial portions of the kidney occurs. As glomerular filtration declines, the renin-angiotensin-aldosterone system is activated, causing hypertension.76 Severe, accelerated, labile, and malignant hypertension have all been reported, and atheroembolic renal disease should be strongly considered in patients who present with resistant hypertension.87,88
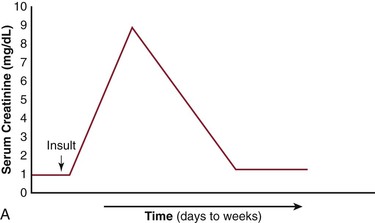
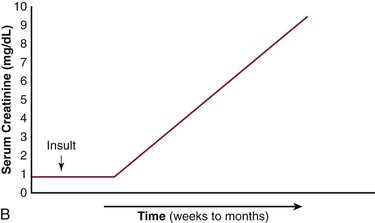
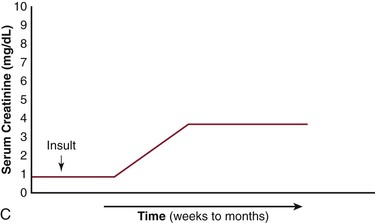
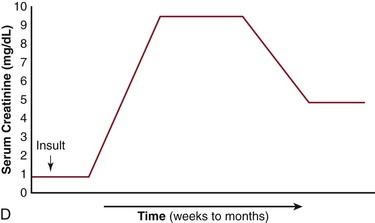
Figure 164-4 Patterns of renal failure in patients with acute tubular necrosis (ATN) and atheroembolic renal disease. A, ATN: the serum creatinine rises within 24 hours of the inciting event and progresses to a peak over a period of days to weeks. Under most circumstances, the creatinine slowly returns to normal or near normal. B, There is a delay of one to several weeks from the inciting event until the creatinine begins to rise. This may progress to end-stage renal disease over a period of weeks to months. C, Delay from the inciting event, followed by a rise in the serum creatinine over a period of weeks to months eventually leveling out and leaving the patient with chronic stable renal disease. D, There have been an increasing number of reports in which the patient requires renal replacement therapy and after a period of time, the renal function improves to the point where the patient no longer requires dialysis. (From Bartholomew JR, et al: Atheromatous embolization. In Young JR, et al, editors: Peripheral vascular diseases, ed 2, St. Louis, 1996, C.V. Mosby Co., pp 266).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


