Approximately 121,000 bariatric surgical procedures are performed annually, and salutary effects include a reduction in cardiovascular morbidity and mortality, risk factor modification, and improvement in sympathovagal tone. There are anecdotal accounts of unexplained sinus bradycardia (SB) after significant weight loss but no systematic studies have been conducted. The purpose of this study was to determine the frequency of incident SB, its timing, and association with weight loss, clinical characteristics, and predictors. We evaluated various clinical characteristics including resting heart rate, blood pressure, body mass index (BMI), heart rate reserve (HRR), basal metabolic rate, and exercise regimen in 151 consecutive patients who underwent bariatric surgery. Multiple logistic regression analysis was performed to determine predictors of SB. Twenty-five of 137 patients (18%) experienced postoperative SB. Patients with SB had significantly greater reduction in BMI than those without bradycardia (35 ± 9.6% and 25.7 ± 13%, respectively, p = 0.002). HRR was significantly greater in patients with SB (116 ± 14 beats/min) compared with those without bradycardia (105 ± 14 beats/min, p = 0.007). Multiple logistic regression analysis revealed that the odds of developing SB were 1.96 and 1.91 and associated with the percent decrease in BMI (95% confidence interval 1.3 to 3.0, p = 0.002) or increase in HRR (95% confidence interval 1.28 to 2.85, p = 0.002), respectively. In conclusion, SB occurred 14 ± 11 months postoperatively and its predictors were the percent reduction in BMI or increase in HRR.
No systematic studies have been conducted to determine the frequency and cause of sinus bradycardia (SB) after bariatric surgery. Thus, the objective of this investigation was to undertake a pilot study by reviewing records of 151 patients who underwent bariatric surgery at our institution, to determine the frequency of incident SB, its timing, the magnitude of weight loss associated with SB, baseline clinical characteristics, and the clinical predictors.
Methods
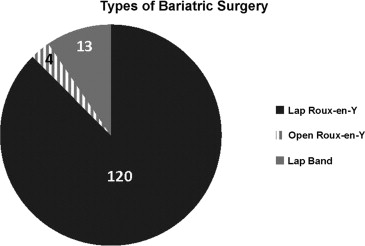
We reviewed data collected prospectively from 151 consecutive patients who underwent bariatric surgery at Hahnemann University Hospital from 2009 to 2010 to determine the frequency of incident SB and clinical variables predictive of postoperative SB. Patient characteristics (age, gender, co-morbidities, and medications), anthropometric measurements (height and weight), body mass index (BMI), basal metabolic rate (BMR), digital heart rate measurements, and heart rate reserve (HRR) were recorded at each quarterly outpatient visit over a follow-up period of 24 months. Fourteen patients were excluded: 6 because of limited data, 6 required surgical revision, and 2 had medication-induced SB. None of the patients had atrial fibrillation. A total of 137 patients were included in this study. There were 120 laparoscopic Roux-en-Y gastric bypass, 13 laparoscopic banding, and 4 open Roux-en-Y procedures ( Figure 1 ).
The co-morbidities specifically evaluated were diabetes mellitus, hypertension, dyslipidemia, obstructive sleep apnea, and hypothyroidism. Hypothyroid patients were further evaluated to determine if they were appropriately medically treated by confirming their thyroid function test results and that presurgical SB was not present. SB was defined as a rate of <60 beats/min at rest. Transient SB was defined as 1 episode of SB recorded at rest in the sitting position a few minutes after disrobing in the exam room. Patients with ≥2 episodes of SB recorded on consecutive office visits and throughout the follow-up period under similar resting state were defined as having persistent bradycardia. BMI was calculated using the height and weight recorded at each visit and reported as kilogram per square meter. Additionally, BMR was calculated as calories/day for every visit using an on-line calculator, which requires inputting the patient’s age, height, weight and gender ( www.BMI-calculator.net/BMR-calculator ).
HRR was defined as the difference between a patient’s maximum predicted heart rate (220−age) and heart rate at rest. This index has been shown to correlate with oxygen consumption and serves as a marker of autonomic balance. We calculated the HRR for all patients both at baseline and at the time of peak reduction in their BMI. Blood pressure (BP) was recorded along with other vital signs at baseline and at all postoperative visits.
All patients were recommended exercise of a minimum of 30 minutes with a suggested frequency of 3 to 5 times/week. Patients reported the duration and frequency of exercise at each visit. Patients who exercised as recommended were considered to be compliant, whereas those who reported less than the minimum or no exercise were considered noncompliant. Those patients whose medical records did not report any data on exercise were excluded from analysis of that variable. The study protocol was approved by the Institutional Review Board of Drexel University College of Medicine.
All values are reported as mean ± SD. Continuous variables were compared using Student t test and the Mann-Whitney U test, and Kruskal-Wallis rank tests were used for nonparametric data. Multiple comparisons of continuous data were analyzed using analysis of variance. Pearson’s chi-square and Fisher’s exact tests were used to analyze categorical data. Multiple logistic regression analysis was employed to determine predictors of SB and appropriate odds ratios. To correlate SB with the reduction in BMI, we calculated the mean heart rate at rest for all patients with bradycardia, its relation and timing to BMI reduction, and relation to the peak reduction in BMI; and determined the heart rate at rest for patients without bradycardia at the time of their peak reduction in BMI. This approach was deemed necessary because not all patients were expected to develop bradycardia at the time of peak reduction in BMI, but all patients were expected to experience a maximum decrease in BMI over the study period. A p value of <0.05 was considered significant. Statistical analysis was performed using the SPSS Statistics software package, version 20 (IBM, Chicago, Illinois).
Results
The mean age of study patients was 39 ± 11 years, which was not significantly different among patients with no bradycardia, with transient, and persistent bradycardia. There were 116 women (85%) and 21 men (15%) with no statistical difference in gender distribution among patients. The mean postoperative follow-up period was 17 ± 11.6 months. Preoperatively, all patients were morbidly obese with a BMI of 48.1 ± 7.8 kg/m 2 with similar preoperative BMI noted in those who did not develop bradycardia and those with transient or persistent bradycardia ( Table 1 ). The preoperative BMR for all patients was 2,123 ± 416 calories/day, and this variable was similar preoperatively among patients who were subsequently classified into the no bradycardia, transient, and persistent bradycardia subgroups postoperatively (p = 0.631). Preoperatively, the HRR for all patients was 99.4 ± 13.2 beats/min and this variable was not significantly different preoperatively among patients who were subsequently classified into the no bradycardia, transient, and persistent bradycardia subgroups postoperatively (p = 0.48). No significant difference in preoperative or postoperative BP was noted irrespective of heart rate.
| Variable | All Patients (n = 137) | SB | p Value | ||
|---|---|---|---|---|---|
| None (n = 112) | Transient (n = 20) | Persistent (n = 5) | |||
| Age (yrs) | 38.8 ± 10.9 | 38.3 ± 11.0 | 40.1 ± 11.1 | 43.2 ± 9.1 | 0.315 |
| Men/Women | 21/116 | 17/95 | 2/18 | 2/3 | 0.140 |
| BMI (kg/m 2 ) | 48.1 ± 7.8 | 48.0 ± 7.5 | 48.8 ± 9.6 | 48.0 ± 7.5 | 0.759 |
| Heart rate (beats/min) | 81.8 ± 10.0 | 82.6 ± 9.9 | 79.5 ± 10.6 | 73.4 ± 3.7 | 0.002 |
| HRR (beats/min) | 99.4 ± 13.2 | 99.1 ± 13.5 | 100.4 ± 12.0 | 103.4 ± 12.7 | 0.481 |
| Reduction in BMI (%) | −27.4 ± 13 | −25.7 ± 13.1 | −34.4 ± 8.5 | −37.4 ± 14.1 | 0.0002 |
| BMR (calories/day) | 2,123 ± 416 | 2,123 ± 416 | 2,040 ± 328 | 2,247 ± 602 | 0.631 |
| Presence of OSA | 69 | 69 | 70 | 80 | 0.590 |
| Hypertension | 61 | 53 | 40 | 80 | 0.230 |
| Diabetes mellitus | 39 | 29 | 40 | 40 | 0.610 |
| Dyslipidemia | 25 | 20 | 25 | 20 | 0.980 |
| Hypothyroidism | 7 | 5 | 10 | 0 | 0.600 |
Baseline clinical characteristics were not significantly different in all patients ( Table 1 ). The preoperative heart rate at rest for all patients was 81.8 ± 10 beats/min. Twenty-five of 137 patients (18.2%) had postoperative SB at rest with transient SB in 20 (14.6%) and persistent SB in 5 patients (3.6%). For the 112 patients who did not develop SB, the mean preoperative sinus rate was 82.6 ± 9.9 compared with a preoperative value of 78.3 ± 9.8 in those patients who eventually developed any bradycardia (p = 0.055). SB was asymptomatic in all patients and resolved in 20 of 25 patients despite continued but tapering weight loss. The mean bradycardic heart rate postoperatively for all patients who had any resting SB was 56.7 ± 3.9 beats/min (range 46 to 59) irrespective of the reduction in BMI and significantly different from the preoperative value (p = 0.0001). However, when correlating the bradycardia rate to the peak reduction in BMI, the mean heart rate at rest was 63 ± 8.9 beats/min. A difference existed between the mean bradycardic heart rate postoperatively and the heart rate at rest at peak reduction in BMI, because transient bradycardia resolved in a few patients whereas study patients still continued to lose weight but at a slower rate thus achieving further decrement in BMI. SB was observed in 24 of 124 patients who underwent Roux-en-Y procedures as opposed to 1 of 13 who had laparoscopic banding. There was no significant difference in observed bradycardia between those patients who had Roux-en-Y procedures compared with laparoscopic banding (p = 0.300).
After bariatric surgery, the average reduction in BMI was 27.4 ± 13% for all patients. Laparoscopic banding was associated with less reduction in BMI (15.2 ± 8.9) than combined open and laparoscopic Roux-en-Y procedures (29.6 ± 11.9% and 29.1 ± 10.9%, respectively, p = 0.0001). Patients without SB had significantly less reduction in BMI than the composite of both groups of patients with SB (25.7 ± 13.1% and 35 ± 9.6%, respectively, p = 0.0002; Figure 2 ). On subgroup analysis, the average percent reduction in BMI was significantly more in patients with transient bradycardia (34.4 ± 8.5) compared with patients without bradycardia (25.7 ± 13.1, p = 0.0005). However, the average percent reduction in BMI in patients with persistent SB (37.4 ± 14.1) was not significantly different from those with transient bradycardia (p = 0.14). Multiple logistic regression analysis revealed that the odds of developing SB postoperatively, when controlling for the percent reduction in BMI, was 1.96 (95% confidence interval [CI] 1.3 to 3.0, p = 0.002), given the difference in mean percent reduction in BMI of 9% in the bradycardia group compared with those without bradycardia. When the HRR at peak decrease in BMI was similarly analyzed, the likelihood of developing SB was 1.91 (95% CI 1.28 to 2.85, p = 0.002).





