Asymptomatic Internal Carotid Artery Stenosis
AMIT JAIN and GILBERT R. UPCHURCH Jr
Presentation
A 73-year-old man with a past medical history significant for hypertension, well-controlled diabetes, and hypercholesterolemia presents to your office after his family physician hears a right-sided neck bruit on routine physical examination. Social history is positive for tobacco use. His medications include a statin, a beta-blocker, an oral hypoglycemic agent, and an aspirin. On review of systems, the patient denies evidence of amaurosis fugax, motor or sensory deficits, difficulty with speech, or any previous history of a transient ischemic attack or stroke. On physical examination, the patient has a right-sided carotid bruit. His peripheral upper extremity pulses are all palpable. A duplex of the carotid arteries is recommended (Fig. 1).
Carotid Duplex Scan
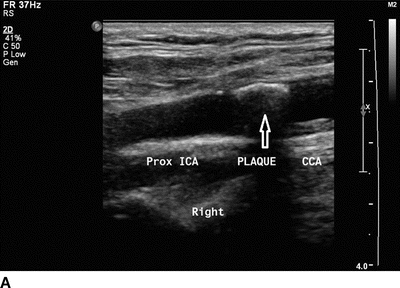
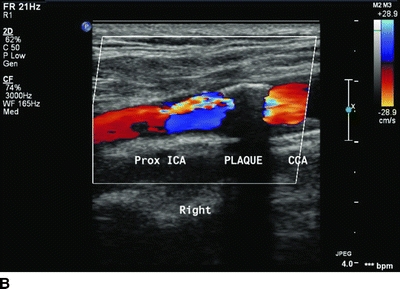
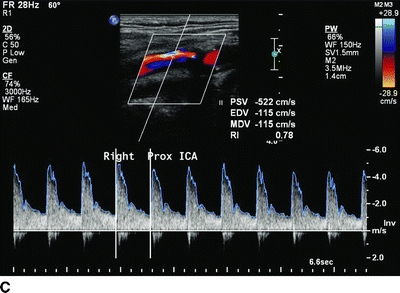
FIGURE 1 Carotid Doppler ultrasound showing carotid bulb and proximal ICA plaque on the gray-scale image (arrow in A) and color flow image (B). Note the high peak systolic and end-diastolic velocities suggestive of high-grade stenosis of the proximal ICA (C).
Carotid Duplex Scan Report
RIGHT CAROTID SCAN: The report suggests that the carotid bulb and internal carotid artery (ICA) show evidence of heterogeneous plaque by both gray-scale and color flow imaging (Fig. 1A and B, arrow denotes extent of plaque on Fig. A).
RIGHT CAROTID DOPPLER:
CCA velocity: 110 cm/s, normal
ICA systolic velocity/end-diastolic velocity: 522/115 cm/s, 80% to 99% diameter stenosis (Fig. 1C)
ICA/CCA ratio: 4.74
ECA: normal, vertebral: antegrade
RIGHT CAROTID IMPRESSION: The right carotid study reveals an 80% to 99% diameter stenosis in the BULB/ proximal ICA. The distal end of the plaque was seen.
LEFT CAROTID IMPRESSION: The left carotid study reveals no significant disease by image. Velocities are suggestive of a less than 39% diameter stenosis in the BULB/ICA.
Differential Diagnosis
This patient has an asymptomatic high-grade right ICA stenosis. Other pathology may be noted on duplex including a carotid body tumor, a carotid artery dissection or aneurysm, or reversal of flow in the vertebral artery (secondary to “subclavian steal”). However, given the patient’s smoking history, physical examination, and duplex results, the diagnosis is an asymptomatic high-grade right ICA stenosis.
Discussion
Stroke is the third leading cause of death in the United States with more than 700,000 strokes and 160,000 deaths annually. It was estimated that in 2007, nationwide stroke expenditure reached $62.7 billion with mean lifetime healthcare expenditure for each stroke patient of about $140,000. Carotid stenois occurs with a prevalence of about 2% to 9% in the general population, 5% to 9% in patients older than 65 years of age, 11% to 26% in those with coronary artery disease and as high as 25% to 49% of those with peripheral arterial disease. At present, approximately 2 million Americans are harboring asymptomatic carotid artery occlusive disease of at least 50% stenosis. About 87% of the strokes are ischemic and remaining 13% hemorrhagic in etiology. Arteriosclerosis of the brachiocephalic trunk, including the carotid arteries, causes greater than 50% of ischemic strokes. Initial plaque size, degree of stenosis, and the composition of the plaque along with some poorly understood events, including timing of plaque rupture, all play an important role in initiating the transformation of a benign carotid bifurcation lesion into a stroke-producing plaque.
The workup for a patient who presents with an asymptomatic or incidental carotid artery stenosis should be systematic. History should be directed at identifying risk factors and prior ischemic events. Physical examination should note signs of cardiac and systemic vascular disease, including assessment of peripheral pulses, examination for bruits, and careful assessment for signs of prior clinical stroke on neurologic examination. It should be noted that neither will all patients with a clinically significant lesion have a carotid bruit, nor will all the patients with a bruit have a hemodynamically significant carotid stenosis. A clinically important stenosis is present in only approximately a third of all patients with a carotid bruit. Also, every effort should also be made when taking a history to review any studies done to assess the carotid arteries in the past.
Carotid duplex ultrasonography is the recommended first screening study in patients who are suspected of having carotid artery stenosis. Duplex is widely available, is rapidly performed, is cost-effective, and carries minimal to no risk. The severity of the ICA lesion can be reliably measured based on the peak systolic flow velocity, the end-diastolic flow velocity, and the internal carotid to common carotid artery (CCA) flow velocity ratio. A good ultrasonographer can establish antegrade flow in the vertebral arteries and can also suggest diseased subclavian arteries if present. Both CT angiography (CTA) and 3D-magnetic resonance angiography (3D-MRA) with 2D-time-of-flight (2D-TOF) are useful in cases where duplex yields contradictory results or in the elucidation of concomitant proximal brachiocephalic or distal intracranial lesions. Other benefits of cross-sectional imaging include that it identifies the extent of the disease, the relationship of the carotid bifurcation to the angle of the mandible, and the tortuous course of the arteries. It is also helpful in assessing the atherosclerotic plaque burden of the aortic arch along with any ostial disease of the innominate or the left CCA, as well as the extent of collateral intracranial circulation. The traditional “gold standard” diagnostic study for carotid artery stenosis has been angiography, but it is rarely used now. Carotid angiography, however, was used in most of the randomized studies examining surgery versus medical therapy, justifying the use of carotid endarterectomy (CEA), and therefore serves as the reference standard against which other modalities are compared. In the ACAS study, confirmatory carotid angiography performed in patients with high-grade carotid stenosis on duplex criteria was associated with a 1.2% risk of stroke. It is useful in its ability to identify coexisting lesions of the great vessels and intracerebral arteries. Following a duplex scan, indications for a CTA, MRA, or carotid angiography include cases where symptoms do not correlate with the extent of carotid disease, the top of the plaque is not visualized, the vessel is extremely tortuous, the ipsilateral carotid artery is occluded, or if there is a high carotid bifurcation.
Recommendations
A right CEA is recommended given the patient’s age (less than 80 years) and gender (male). A combined 3% risk of ipsilateral stroke, myocardial infarction, and death is quoted. A 5% to 10%, usually transient, cranial nerve injury risk is described. Given the patient’s age (less than 80 years), lack of EKG abnormalities, no history of heart failure, and a good overall activity status (he is able to walk up a flight of stairs without shortness of breath), no further preoperative cardiac testing is performed. The patient is continued on his statin, beta-blocker, and aspirin preoperatively.
Surgical Approach
The patient undergoes appropriate monitoring including a radial arterial line and continuous percutaneous cerebral oximetry. General anesthesia is used (some surgeons prefer using cervical plexus block). The patient is placed supine in a beach chair position with neck extended and a shoulder roll underneath the scapulae. The neck is prepped including the ipsilateral ear lobe, the lower border of mandible and the sternal notch. An incision is made parallel to the anterior border of the sternocleidomastoid muscle, trying to incorporate skin lines. The platysma is divided, and the sternocleidomastoid muscle is retracted posteriorly. The carotid sheath is entered, and from this point on in the operation, sharp dissection is utilized. The facial vein is identified, ligated, and divided. Carotid artery dissection is performed with as little manipulation of the artery as possible. The vagus and the hypoglossal nerves are identified and protected. The CCA and the external carotid artery (ECA) are encircled. The patient is systemically heparinized (100 units/kg), and the ICA is encircled distal to the bulb plaque. The blood pressure is kept at around a systolic of 150s to 160s during the time of carotid artery cross clamping. After 3 minutes of heparinization, the ICA, ECA, and the CCA are clamped. An anterior longitudinal arteriotomy is made in the CCA below the bulb and extended up the ICA until the top of the plaque is reached. A drop of >20% in the cerebral oxygen saturation from the baseline is used as an indicator to use inline shunt. (In an awake patient with cervical block, a test clamp is placed on the ICA and ECA first, and if there is no change in the neurologic exam, the CCA is then clamped). Back bleeding from the ICA is also assessed. Others use EEG monitoring or back pressure measurements of the ICA. Still others just shunt everyone. While the literature is full of multiple large case series about how to manage clamping the carotid, most would acknowledge that this is operator dependent and that most of the techniques are acceptable. The endarterectomy is begun in the CCA where the plaque is cut flush. An eversion endarterectomy of the ECA is then performed with good back bleeding. A nicely feathering plaque is removed from the distal ICA. All debris is removed. A synthetic patch is sewn in with fine monofilament suture. A bovine pericardial patch or autologous saphenous vein patch is also a viable option. Prior to completing the patch, the ECA and ICA are back bled and the CCA is bled forward. The patch is completed. Following patch closure, an intraoperative duplex scan shows normal velocities (Fig. 2A and B) with no evidence of debris. The incision is closed over a drain, and the drapes are removed. The patient is neurologically intact and is transferred to the postanesthesia care unit where he received an aspirin. The patient is discharged to home the next morning on antiplatelet and antihypertensive medications with a follow-up appointment in 4 weeks.
Intraoperative Carotid Duplex Scan
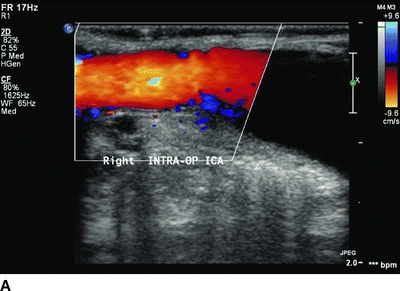
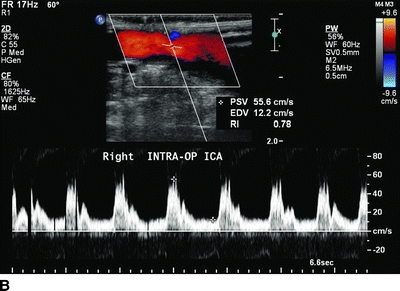
FIGURE 2 Intraoperative carotid Doppler after patch repair showing resolution of the stenosis of the carotid bulb and proximal ICA (A) and return of flow velocities within normal range (B).



