In patients with heart failure (HF) with chronic obstructive pulmonary disease (COPD), concerns exist regarding β blockers, particularly noncardioselective β blockers, precipitating bronchospasm or attenuating the benefit of inhaled β 2 agonists. The aim of this study was to test the hypothesis that noncardioselective β blockers would not be associated with worse outcomes compared with cardioselective β blockers in patients with concomitant COPD in a large HF registry. A retrospective analysis of patients from the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF) who had systolic dysfunction, documentation of β-blocker status, and follow-up information available after index hospitalization (n = 2,670) was performed. The associations between cardioselective and noncardioselective β blockers and the end points of 60- to 90-day mortality and mortality or rehospitalization in patients with (n = 722) and without (n = 1,948) COPD were analyzed using regression modeling. The models were adjusted for covariate predictors of β-blocker use at discharge and clinical predictors of outcomes. Noncardioselective and cardioselective β blockers were associated with lower risk-adjusted mortality in patients with and without COPD. There was no evidence that β-blocker selectivity was associated with a difference in outcomes between patients with and those without COPD (p for interaction >0.10 for both outcomes). In conclusion, despite concerns regarding β blockers in patients with HF with COPD, there was no evidence that β-blocker selectivity was associated with differences in outcomes for patients with HF with COPD versus those without.
Chronic obstructive pulmonary disease (COPD) is a common co-morbidity in patients with heart failure (HF) (approximately 30%). Data suggest that COPD independently increases HF hospitalizations, length of stay, costs, and mortality, although data have been conflicting. Clinicians underuse evidence-based HF therapies in these patients. Concerns exist regarding β blockers, particularly noncardioselective β blockers, precipitating bronchospasm. However, patients with COPD have largely been excluded from HF trials. Thus, the impact of β-blocker selectivity in patients with concomitant HF and COPD has not been well characterized. We explored the interaction between β-blocker selectivity and outcomes in patients with COPD after admission for HF in patients with systolic dysfunction in the Organized Program to Initiate Lifesaving Treatment in Hospitalized Patients With Heart Failure (OPTIMIZE-HF). We hypothesized that noncardioselective β blockers would not be associated with worse outcomes compared to cardioselective β blockers in patients with HF with concomitant COPD.
Methods
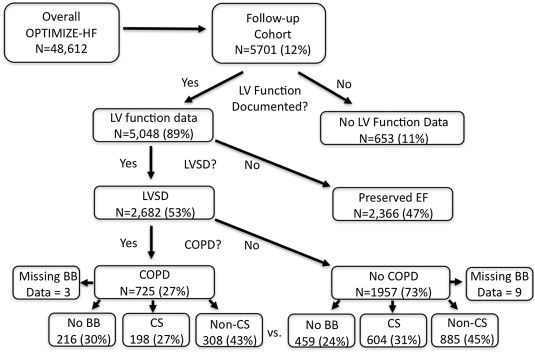
OPTIMIZE-HF consisted of a registry and quality-of-care intervention. Briefly, OPTIMIZE-HF enrolled 48,612 patients from 2003 to 2004 from 259 hospitals across the United States. Eligible patients were enrolled if they were hospitalized with new-onset or worsening HF and had primary discharge diagnoses of HF. A prespecified subset of approximately 12% (n = 5,701) of the cohort was followed for 60 to 90 days after discharge. The follow-up cohort was demographically similar to the patients in the overall cohort. The investigation conformed with the principles outlined in the Declaration of Helsinki. The OPTIMIZE-HF registry was approved by the appropriate regulatory authorities and ethics committees before patient enrollment, and written informed consent was obtained from each patient before entry.
A hierarchical definition of left ventricular systolic dysfunction (LVSD) was used as previously described. In brief, LVSD was defined first by a left ventricular ejection fraction <40%. If the left ventricular ejection fraction was unavailable, then the description of left ventricular dysfunction was used (i.e., moderate or severe). In the registry, 20,118 patients had LVSD at index hospitalization, and 2,682 of them had 60- to 90-day follow-up. Beta-blocker use was unavailable for 9 patients in the no-COPD group and 3 patients in the COPD group. Our analysis was restricted to 2,670 patients with complete data.
COPD status at admission was prospectively recorded by the clinician-investigator on the basis of available clinical data and/or medical history of COPD before the HF hospitalization, including chronic productive cough, chronic wheezing, emphysema, or chronic bronchitis, as previously described.
Cardioselective β blockers that primarily antagonize the β 1 receptor include metoprolol, bisoprolol, atenolol, and nebivolol. Noncardioselective β blockers that antagonize the β 1 and β 2 receptors include carvedilol, labetalol, pindolol, propranolol, nadolol, and timolol.
Clinical characteristics as a function of baseline COPD status were evaluated in those with LVSD (n = 2,682; Figure 1 ). For the 2 groups defined by COPD status, continuous variables are summarized with medians and 25th and 75th percentiles and compared using Wilcoxon’s test. Categorical variables are presented as frequencies and percentages and were compared using chi-square tests. The associations between cardioselective and noncardioselective β blockers and the end points of 60-day mortality and 60- to 90-day mortality or rehospitalization in patients with and without COPD were analyzed through regression modeling. The interaction between type of β blocker (no β blocker, cardioselective, or noncardioselective) by COPD status was tested. For the mortality end point, event rates were estimated using the Kaplan-Meier method. For the mortality or rehospitalization end point, rates were estimated as the percentage of patients with the composite event during the follow-up. Time to rehospitalization was not available to allow estimation of the Kaplan-Meier rates for the mortality or rehospitalization end point. The models were adjusted by covariate predictors of β-blocker use at discharge and clinical predictors of outcome on the basis of the OPTIMIZE-HF risk models. Statistical significance was assessed using 2-sided statistical tests. A p value <0.05 was considered statistically significant. All statistical analyses were performed at the Duke Clinical Research Institute (Durham, North Carolina) using SAS version 9.2 (SAS Institute Inc. Cary, North Carolina).
Results
COPD was present in 725 patients (27%) in the follow-up cohort with LVSD. Baseline characteristics are listed in Table 1 . Multiple co-morbidities were more common in patients with COPD compared to those without COPD, including hyperlipidemia, renal insufficiency, vascular disease, and arrhythmias. Admission systolic blood pressure and basic laboratory values, including serum sodium, creatinine, and natriuretic peptide, were similar between groups. Patients with COPD demonstrated similar use of angiotensin-converting enzyme inhibitors or angiotensin receptor blockers but lower use of aldosterone antagonists at discharge compared to those without COPD. Patients with COPD were less likely to receive β blockers at discharge compared to those without COPD ( Table 2 ). Of patients receiving β blockers at discharge, the breakdown between those receiving cardioselective (about 40%) versus noncardioselective (about 60%) agents was similar in those with and without COPD. Metoprolol succinate was the most common cardioselective agent in patients with and those without COPD (about 20% of β-blocker use). Metoprolol tartrate and atenolol were the second and third most common cardioselective agents at about 12% and 5%, respectively. Carvedilol accounted for most noncardioselective β blockade, at about 58% of all β blockers used. The median β-blocker dose (i.e., carvedilol dose equivalent; see Appendix ) was similar between the COPD and non-COPD groups ( Table 2 ).
| Characteristic | COPD | p Value | |
|---|---|---|---|
| No (n = 1,957) | Yes (n = 725) | ||
| Age (yrs) | 71 (59–80) | 73 (63–80) | 0.05 |
| Men | 63% | 63% | 0.86 |
| African Americans | 22% | 18% | 0.01 |
| Ischemic cause of HF | 52% | 52% | 0.71 |
| Ejection fraction (%) | 25 (20–30) | 25 (20–30) | 0.04 |
| Hypertension ∗ | 67% | 69% | 0.16 |
| Diabetes mellitus † | 41% | 43% | 0.39 |
| Hyperlipidemia ‡ | 39% | 46% | 0.0001 |
| Renal insufficiency § | 18% | 22% | 0.01 |
| Peripheral vascular disease | 12% | 21% | <0.001 |
| Previous stroke or transient ischemic attack | 13% | 16% | 0.04 |
| Pulmonary hypertension | 6% | 10% | 0.001 |
| Atrial arrhythmia | 30% | 35% | 0.01 |
| Ventricular arrhythmia | 11% | 16% | 0.001 |
| Systolic blood pressure (mm Hg) | 130 (112–151) | 130 (113–149) | 0.73 |
| Serum sodium (mEq/L) | 138 (135–141) | 138 (135–140) | 0.14 |
| Serum creatinine (mg/dl) | 1.3 (1.0–1.8) | 1.3 (1.0–1.8) | 0.79 |
| Hemoglobin (g/dl) | 13 (11–14) | 13 (11–14) | 0.89 |
| N-terminal pro–brain natriuretic peptide (pg/ml) | 1,130 (601–2,320) | 1,150 (566–2,395) | 0.94 |
| Implantable cardioverter defibrillator | 11% | 13% | 0.29 |
| Angiotensin-converting enzyme inhibitor at discharge | 66% | 63% | 0.17 |
| Angiotensin receptor blocker at discharge | 11% | 12% | 0.86 |
| Aldosterone antagonist at discharge | 23% | 18% | 0.02 |
∗ History of high blood pressure, defined as systolic blood pressure >160 mm Hg and diastolic blood pressure >90 mm Hg, whether or not the patient is receiving prescribed medications.
† History of physician-diagnosed, insulin- or non-insulin-dependent diabetes, including the use of diet or oral hypoglycemic agents.
‡ Low-density lipoprotein >100 mg/dl in patients at high risk, >130 mg/dl in patients at moderate risk, and >160 mg/dl in patients at low risk on the basis of Adult Treatment Panel III clinical guidelines.
§ History of physician-diagnosed renal insufficiency or chronic renal failure or serum creatinine >2.0 mg/dl.
| Variable | COPD | p Value | |
|---|---|---|---|
| No (n = 1,948) | Yes (n = 722) | ||
| β-blocker use at discharge | 77% | 70% | 0.001 |
| Of those patients receiving β blockers at discharge | |||
| Cardioselective | 41% | 39% | 0.57 |
| Dose (mg) ∗ | 25 (13–50) | 25 (13–50) | 0.67 |
| Noncardioselective | 59% | 61% | 0.57 |
| Dose (mg) ∗ | 13 (6–25) | 13 (6–25) | 0.27 |
∗ Carvedilol dose equivalent (see Appendix ).
Table 3 lists the event rates for 60-day mortality and 60- to 90-day mortality or rehospitalization in patients with and those without COPD stratified by β-blocker use and selectivity. The overall Kaplan-Meier 60-day mortality estimates were 6.2% and 6.0% in those with and without COPD, respectively. Beta-blocker use, either cardioselective or noncardioselective, was associated with a similar mortality rate in patients with and without COPD. No β-blocker use, compared to β-blocker use, was associated with higher mortality in those with and without COPD (7.8% and 10.1%, respectively). With regard to mortality or rehospitalization, 34.3% of patients without COPD and 41.0% of those with COPD experienced the composite end point. In the non-COPD group, β-blocker use was associated with lower mortality or rehospitalization (about 32% with cardioselective and noncardioselective agents) compared to 42.6% in those not receiving β blockers. In the COPD group, patients receiving cardioselective β blockers had a similar mortality or rehospitalization event rate (43.6%) compared to those not receiving β blockers (44.1%). In contrast, the COPD group receiving noncardioselective β blockers had a lower event rate of 37.7%.
| Variable | COPD | |
|---|---|---|
| No (n = 1,948) | Yes (n = 722) | |
| 60-day mortality, events (Kaplan-Meier %) | ||
| No β blocker | 43 (10.1%) | 16 (7.8%) |
| Cardioselective β blocker | 28 (4.9%) | 12 (6.2%) |
| Noncardioselective β blocker | 38 (4.5%) | 15 (5.0%) |
| Total | 110 (6.0%) | 43 (6.2%) |
| 60- to 90-day mortality or rehospitalization, events (%) | ||
| No β blocker | 189 (42.6%) | 93 (44.1%) |
| Cardioselective β blocker | 184 (31.5%) | 85 (43.6%) |
| Noncardioselective β blocker | 281 (31.9%) | 114 (37.7%) |
| Total | 658 (34.3%) | 293 (41.0%) |
Table 4 lists the association between β-blocker use and selectivity and outcomes in patients with and without COPD, adjusted for potential confounders. Compared to no β-blocker use, cardioselective and noncardioselective agents were associated with lower 60-day mortality in those with and without COPD. There was no significant difference between cardioselective and noncardioselective β blockers for 60-day mortality in the 2 study arms; the β-blocker type by COPD interaction p value for the mortality analysis was 0.82. For the mortality or rehospitalization end point in patients without COPD, cardioselective and noncardioselective β blockers were associated with lower mortality or rehospitalization. In patients with COPD, β-blocker use was not associated with significantly lower mortality or rehospitalization. However, there was no evidence that β-blocker selectivity was associated with a difference in mortality or rehospitalization between patients with and those without COPD (p for interaction >0.10).
| Variable | COPD | |
|---|---|---|
| No (n = 1,948) | Yes (n = 722) | |
| Hazard ratio for 60-day mortality ∗ (95% confidence interval) | ||
| Cardioselective vs no β blocker | 0.56 (0.34–0.90) | 0.53 (0.25–1.13) |
| Noncardioselective vs no β blocker | 0.59 (0.38–0.92) | 0.47 (0.25–0.89) |
| Cardioselective vs noncardioselective β blocker | 0.94 (0.57–1.54) | 1.14 (0.57–1.56) |
| β blocker type by COPD interaction, p value | 0.82 | |
| Odds ratio for 60- to 90-day mortality or rehospitalization † (95% confidence interval) | ||
| Cardioselective vs no β blocker | 0.70 (0.52–0.95) | 1.19 (0.75–1.87) |
| Noncardioselective vs no β blocker | 0.74 (0.57–0.98) | 0.89 (0.59–1.35) |
| Cardioselective vs noncardioselective β blocker | 0.94 (0.73–1.22) | 1.33 (0.87–2.03) |
| β blocker type by COPD interaction, p value | 0.15 | |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


