Arterial Thoracic Outlet Syndrome
MARGARET CLARKE TRACCI
Presentation
A 47-year-old woman with a history of smoking presents to the emergency department with a cool, painful right hand and bluish discoloration of several fingertips. She has had several episodes of coolness and tingling of her fingertips with associated discoloration over the past several months, although these have previously resolved on their own. Physical examination reveals a cool hand with dusky color changes to several fingertips. Radial and ulnar pulses are not palpable. A proximal brachial pulse is palpable, as is the subclavian just above the clavicle.
Differential Diagnosis
The differential diagnosis for upper extremity ischemia includes atherosclerotic disease, embolic phenomena, and vasculitis. Atherosclerotic disease most commonly presents as chronically progressive fatigue with activity, typically related to a proximal lesion of the subclavian or innominate artery. Atherosclerotic lesions, which tend to be proximal in location, may also serve as a nidus for distal emboli.
Other proximal sources of emboli include the heart and aneurysms of the subclavian or innominate arteries. Aneurysms in this position may be associated with atherosclerosis, connective tissue disorders, anatomic anomalies such as an aberrant right subclavian artery, or represent poststenotic dilatation distal to extrinsic compression within the thoracic outlet. Larger emboli lodging in brachial, radial, and ulnar arteries may present more dramatically, with the sudden onset of ischemic symptoms, though the rich collateralization of the upper extremity often protects patients from critical ischemia even with complete occlusions of these vessels. Microemboli may present much more subtly, with recurrent episodes ranging from painful, markedly ischemic fingertips to an asymmetric Raynaud’s phenomenon.
Less frequently, ischemia of the upper extremity may be related to large (Takayasu’s), medium (thromboangiitis obliterans or Buerger’s disease), or small vessel (ANCA-associated) arteritides. Functional disorders resulting in very distal ischemia include Raynaud’s phenomenon or rarer vasomotor phenomena, such as erythromelalgia.
Workup
The patient undergoes CT angiography (CTA) for further evaluation of her upper extremity ischemia, which reveals a thrombus-lined aneurysm of the midsubclavian artery, occlusion of the brachial artery, and evidence of embolization to the digital arteries of the hand. A right cervical rib is noted with a prominent synostosis with the first rib (Figs. 1,2 to 3).
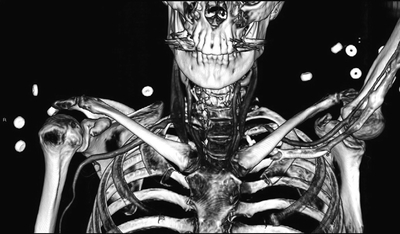
FIGURE 1 3D CT reconstruction demonstrating right cervical rib.
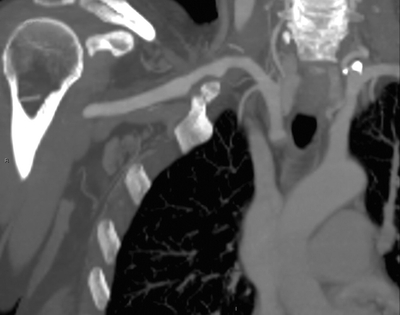
FIGURE 2 CT image demonstrating thrombus-lined subclavian artery aneurysm.
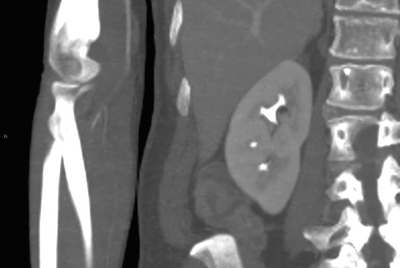
FIGURE 3 CT image demonstrating brachial artery occlusion.
CTA offers several advantages in the diagnosis of arterial thoracic outlet syndrome (aTOS). While catheter-based angiography remains the gold standard for fine resolution imaging of the distal arteries of the hand and digits, it may not fully demonstrate a thrombus-lined aneurysm. CT offers excellent 3D renderings of both the vascular system and of the surrounding musculoskeletal structures that create compressive syndromes of the thoracic outlet. MR angiography (MRA) does not yet offer sensitivity equal to CTA for arterial thoracic outlet syndrome. Plain chest radiographs may demonstrate bony abnormalities such as cervical rib, anomalous transverse process, or a callused fracture of the clavicle that are classically associated with aTOS.
Noninvasive vascular laboratory studies are of somewhat limited diagnostic utility. Traditionally, maneuvers intended to elicit compression of the subclavian artery have been performed, with examination for changes in flow velocity or diameter by duplex ultrasound or waveform with pulse volume recordings. However, there is a significant rate of false-positive results, with nearly 20% of asymptomatic patients demonstrating some degree of arterial compression with abduction maneuvers. Duplex may be useful in identifying aneurysm disease, intraluminal thrombus or injury, and patency of distal vessels. Pulse volume recordings with segmental pressure measurements are useful in the identification and quantification of digital embolization.
Laboratory evaluation is typically useful only to the extent that it may identify or rule out conditions, such as vasculitis or thrombophilia in the differential diagnosis of upper extremity ischemia.
Diagnosis and Treatment
The presentation, clinical examination, and imaging studies are consistent with arterial thoracic outlet syndrome with aneurysm degeneration of the artery distal to the site of extrinsic compression and presenting with distal embolization of aneurysm thrombus. These patients typically present with microembolization to the digits but may suffer from larger emboli resulting in brachial artery occlusion or present with exertional pain that is either subtle and positionally related or more severe and related to aneurysm thrombosis, compressive symptoms related to aneurysm growth, or asymmetric Raynaud’s phenomenon.
While arterial, venous, and neurogenic thoracic outlet syndrome all involve compression of structures passing through the confines of the thoracic outlet, presentation, the location of extrinsic compression, and management differ significantly. Arterial thoracic outlet syndrome is the least common of the three, representing 1% to 6% of patients in large series of thoracic outlet decompression. The source of compression in this syndrome is most frequently a cervical rib, which is present in this case, but may also be an anomalous first rib, fibrocartilaginous bands, prior clavicular fracture with associated bony callus, or an elongated C7 transverse process. Where a cervical rib is present, the artery is typically high riding and easily palpable well above the clavicle (Figs. 4 and 5).
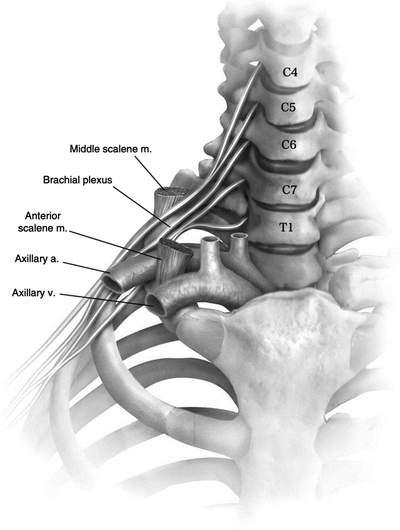
FIGURE 4 Anatomic relationships at the thoracic outlet. (From Tracci MC. Thoracic outlet syndrome: transaxillary approach. Op Tech Thorac Cardiovasc Surg. 2011;16(4):267–277, with permission.)



