Anticoagulants in NSTEACS
The ACC/AHA guidelines summarizing the recommendations for the use of anticoagulant therapy in NSTEACS patients separate anticoagulant management of these patients on the basis of whether treating physicians will pursue an invasive management strategy (early diagnostic catheterization to then triage patients for further medical therapy, PCI, or coronary artery bypass grafting [CABG]) or a conservative management strategy (medical therapy followed by noninvasive risk stratification) (
1). Once the diagnosis of ACS has been made, patients should be immediately started on anticoagulant therapy regardless of the management strategy—a Class I recommendation in the ACC/AHA guidelines (
Table 4-1). The notable exception to this is for those patients whose ACS is not a consequence of an atherothrombotic process, but is rather a secondary event (e.g., as a result of severe blood loss, trauma, or sepsis).
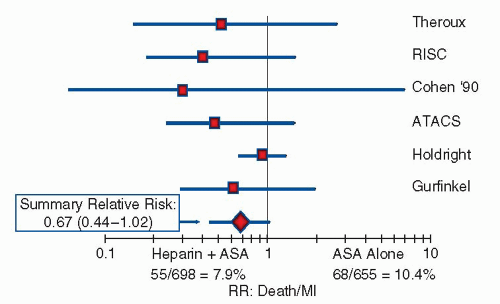
There are several classes of anticoagulants that have been shown to be effective in treating patients with ACS: unfractionated heparin (UFH), low-molecular-weight heparins, direct thrombin inhibitors, and Factor Xa inhibitors. The primary function of these agents is to inhibit the coagulation cascade, thereby preventing or minimizing thrombosis in order to alleviate the ischemic effects of ACS. A critical management issue related to the use of anticoagulant agents in ACS is the potential tradeoff of more potent anticoagulation (aimed at maximizing anti-ischemic efficacy) for an increase in bleeding complications. The association between ischemic events and late mortality has been recognized historically and well described in studies of ACS; in fact, this is one of the fundamental principles behind the use of anticoagulant therapy in ACS. More recently, a strong linkage between nonfatal bleeding events and subsequent mortality has also emerged in both randomized clinical trials and observational studies on ACS (
2,
3 and
4). Thus, the treating physician must be acutely aware of the joint importance of both ischemic and bleeding complications when selecting the optimal anticoagulant strategy for patients with NSTEACS.
Anticoagulant Use with an Invasive Management Strategy
Patients presenting with NSTEACS who are being treated with an invasive management strategy are usually started on anticoagulant therapy at the time of diagnosis, and typically taken to the catheterization lab within 48 hours of presentation. Anticoagulant agents that have been shown to be effective in this setting include intravenous bivalirudin, intravenous UFH, subcutaneously administered fondaparinux, or subcutaneously administered enoxaparin. As stated in the guidelines, there are limited comparative data among the various Class I agents in this setting, and across-study comparative assessments based upon historical data are often confounded by changes in adjunctive therapies (e.g., antiplatelet agents) over time. Thus, the specific choice of an anticoagulant agent may be a physician- or an institution-dependent decision, modified by patient-specific factors.
NSTEACS patients undergoing PCI frequently require uptitration of anticoagulant dosing at the time of PCI in order to minimize the additional thrombogenicity associated with the procedure (
Table 4-2). Consistency in anticoagulant choice should be maintained in most circumstances as several studies have demonstrated
an associated increased risk of bleeding when switching anticoagulant agents, particularly if enoxaparin is used as the initial anticoagulant (
5). In rare cases (for example in the treatment of intraprocedural thrombotic complications), patients may require the use of more than one anticoagulant agent during PCI. Additionally, because of an increased rate of catheter-related thrombotic complications observed during PCI performed with fondaparinux (
2), many operators have adopted a strategy of intraprocedural treatment with UFH in patients initially treated with this agent (
6).
Anticoagulant therapy is typically discontinued immediately following PCI because continued administration has demonstrated limited additional anti-ischemic benefits and an increased risk of bleeding.
Anticoagulant Use with a Conservative Management Strategy
The goal of anticoagulant therapy in patients with NSTEACS is first to placate the activated prothrombotic state. Appropriate patients can then be further risk-stratified with noninvasive testing, which may lead to a more selective use of angiography and/or revascularization. Conservatively managed patients with NSTEACS may be treated with various anticoagulants, including UFH, enoxaparin, or fondaparinux. According to the current ACC/AHA guidelines, bivalirudin is not considered part of the armamentarium for a conservative management strategy because of the limited data with this agent in conservatively managed patients. A Class IIa recommendation is given to the use of either fondaparinux or enoxaparin over UFH for the treatment of ACS in conservatively managed patients.
There are limited data regarding the exact duration of anticoagulant therapy in conservatively managed patients; however, it is generally accepted practice to continue these agents for at least 48 hours after initial presentation.
Anticoagulants during PCI
Anticoagulation is generally administered during PCI in order to suppress the thrombotic process that may be precipitated by the introduction of foreign objects into the coronary vasculature (i.e., catheters, wires, balloons, stents). Further, anticoagulants can help suppress activation of the thrombotic cascade following vessel injury during PCI. There are several classes of anticoagulants that have shown to be effective in treating patients undergoing PCI, including UFH; enoxaparin, a low-molecular-weight heparin; and direct thrombin inhibitors such as bivalirudin.
Anticoagulants are typically not administered during diagnostic catheterization procedures with the exception of radially performed diagnostic procedures. If the radial artery is chosen as the access site for angiography, it is recommended that parenteral
anticoagulation be started immediately after the arterial sheath is placed in order to reduce the risk of radial artery occlusion. Spaulding et al. demonstrated a correlation between the dose of UFH therapy used following radial access and the rate of radial artery occlusion post procedure in 415 patients; occlusion occurred in 71% of patients with no UFH therapy, 24% in patients treated with 2,000 to 3,000 U of UFH, and 4.3% in those treated with 5,000 U of UFH (
7). Whether the use of more modern hydrophilic sheaths, smaller catheter sizes, and shorter procedure times can completely mitigate this effect is unknown.
Once the decision is made to pursue PCI (irrespective of the access site), the ACC/AHA/SCAI guidelines give a Class I recommendation to administer parenteral anticoagulation at the time of the procedure (
Table 4-3) (
8). Specific recommendations regarding the choice of agent depend upon the clinical scenario. For elective PCI (or in patients not previously on parenteral anticoagulants), an anticoagulant agent is chosen and typically administered as a parenteral bolus, with an infusion lasting for the duration of the PCI. For patients with NSTEACS treated with upstream therapy, the dose of anticoagulation is typically higher during PCI than during maintenance upstream therapy, and several therapies used upstream are not indicated for PCI; thus, specific decisions regarding switching anticoagulants, further bolus dosing, and/or increasing the dose of infusion are required (
Table 4-2). Of the anticoagulants used during PCI, UFH is one agent for which intraprocedural monitoring of levels of anticoagulant activity is recommended.
In general, anticoagulant therapy is discontinued immediately following PCI. Decisions regarding management of the vascular access site depend upon several factors: the site of access (e.g., femoral vs. radial), whether use of a vascular closure device is planned, and the particular anticoagulant used. For femoral access, if use of a vascular closure device is planned, it is typically deployed immediately after PCI. For manual compression of a femoral access site, sheaths are usually removed when the activated clotting time (ACT) falls below 150 to 180 seconds in patients treated with UFH; for patients treated with bivalirudin, sheaths are typically removed 2 hours after termination of the infusion. For radial access, sheath removal is typically performed immediately after PCI by applying nonocclusive pressure, typically with a specialized pressure device (to achieve patent hemostasis).