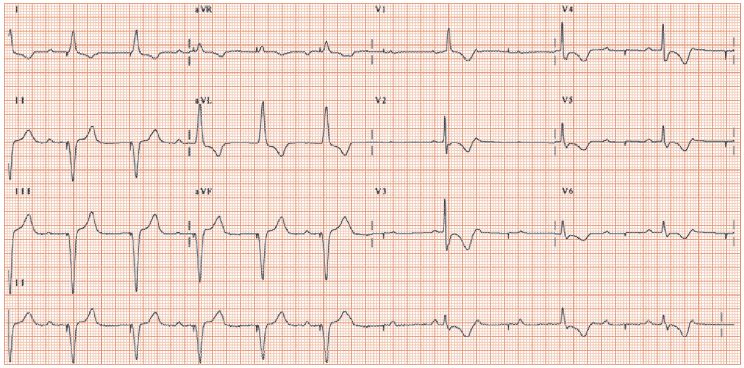
Fig. 59.2 Failure to pace. The first six beats show a pacing spike followed by a paced QRS complex (VVI pacemaker), then the pacing spike occurs (arrowed) but no paced beats follow, ‘failure-to-pace’. Fortunately, the underlying heart rhythm, complete heart block, rapidly emerged. The pacemaker output was set too low; the problem resolved when it was increased.
Anti-bradycardia pacemakers comprise the majority of pacemakers (88% of the 35 000 pacemaker device implanted in the UK in 2004). They determine whether normal cardiac electrical activity has occurred; if so, they are silent, if not, then they stimulate the heart to beat. The common indications are: third degree atrioventricular (AV) block (30% of implants), sick sinus syndrome (25%), atrial fibrillation with bradycardia (20%), second degree heart block (15%), others (10%). Except in rare circumstances (see Chapter 60) they do not prevent tachycardias (e.g. in atrial fibrillation [AF] with pauses antitachycardic medication is still needed post-pacemaker implantation).
Pacemaker implantation
Pacemakers are implanted under local anaesthetic, in the left upper chest of right-handed individuals. The skin is cut, the cephalic vein identified and opened, the electrode introduced and pushed into the relevant heart chamber, guided into position under X-ray imaging, tested (see below), stitched so it cannot withdraw from the heart, and connected to the generator. The generator is inserted into a pocket made medially in the chest, over pectoral major and under the dermis/subcutaneous fat. The skin wound is sewn up. The procedure takes 30–60 min. The complication rate is low (pneumothorax, haemothorax, pacemaker infection, arrhythmias).
The paced ECG
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


