ANOMALOUS PULMONARY VENOUS CONNECTIONS
Introduction, Nomenclature, and Embryogenesis
Abnormalities associated with connections of the pulmonary veins are rare and comprise 0.5–1.5% of cases of congenital heart disease (CHD). These abnormalities traditionally have been divided into two major subgroups. Total anomalous pulmonary venous connection (TAPVC) occurs when all of the pulmonary veins from both lungs do not connect normally to the left atrium (LA) but instead connect to systemic veins in the chest or abdomen or directly to the right atrium (RA). With rare exception, it is obligatory for patients with TAPVC to have an atrial septal defect (ASD) or patent foramen ovale (PFO) to sustain life. Partial anomalous pulmonary venous connection (PAPVC) constitutes the abnormal connection of one or several pulmonary veins. But, in PAPVC at least one pulmonary vein connects normally to the LA. PAPVCs can have a large variety of connections to systemic veins or the RA. Most patients with PAPVC have an ASD.
There are important clinical differences between the two subgroups. Patients with a TAPVC will usually present early in life with cyanosis and severe pulmonary hypertension secondary to pulmonary venous obstruction, whereas patients with a PAPVC will usually be asymptomatic in childhood. Patients with PAPVC may be discovered incidentally in adulthood or present with signs and symptoms similar to an ASD. Meticulous echocardiographic assessment from multiple imaging planes is essential to confidently establish that the pulmonary venous connections are normal. If one cannot identify all of the pulmonary veins, then an exhaustive search for the pulmonary venous connections must ensue. If transthoracic echocardiography (TTE) is non-diagnostic, then other imaging modalities must be utilized, such as transesophageal echocardiography (TEE), computed tomography (CT), magnetic resonance imaging (MRI), or, rarely, cardiac catheterization.
Normally, there are two right-sided and two left-sided pulmonary veins. Although the normal right lung has three lobes, the right middle and upper veins usually join before entering the LA. The most common variation in normal pulmonary venous anatomy is to have a single pulmonary vein from either lung (a single left vein is more common). Healey reported in 1952 that this occurs in as many as 24% of anatomic specimens. During early embryogenesis, part of the splanchnic plexus forms the pulmonary vascular bed. The pulmonary vascular bed is connected to the umbilicovitelline and cardinal venous systems. The pulmonary vascular bed is not connected to the heart during early development. Eventually, an evagination from the LA joins the interparenchymal pulmonary veins to form the “common pulmonary vein.” The common pulmonary vein, also termed a pulmonary venous confluence, becomes incorporated completely into the LA during the first month of gestation. Once this connection to the heart is established, the original pulmonary venous attachments to the splanchnic plexus involute. All abnormalities of pulmonary venous connections can be understood based on the original development of the pulmonary veins from the splanchnic plexus (Fig. 5.1). In 2001, Tal Geva and Stella van Praagh provided an excellent review of pulmonary venous embryology and anomalies (Moss and Adams: Heart disease in infants, children and adolescents). This chapter is recommended reading for those interested in further description of the embryogenesis of pulmonary venous anomalies.
A distinction should also be made between the exact anatomic “connection” of a pulmonary vein to the LA or other vessel/chamber and the “drainage” of a pulmonary vein. Although a pulmonary vein may “connect” normally to the LA, if malposition of the atrial septum (Fig. 5.2) or an ASD is present, pulmonary venous flow may actually “drain” across the interatrial defect into the RA. Therefore, the echocardiographer should use this terminology carefully when communicating with a surgeon.
Features of Transthoracic (TTE) Imaging of Pulmonary Venous Connections
Accurate delineation of the pulmonary venous connections to the LA requires clear two-dimensional imaging from multiple imaging windows. Color and spectral Doppler imaging is required to demonstrate flow from each pulmonary vein into the LA. Suspicion of APVC should be raised if right-sided volume is demonstrated, especially if no interatrial communication is observed. In newborns, suspect TAPVC if the left atrial size is reduced.
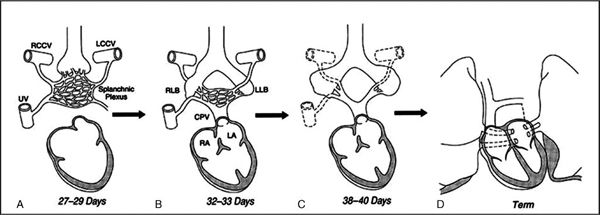
Figure 5.1. Embryologic development of the pulmonary veins from the splanchnic plexus during the first month of embryogenesis. A: Lung buds connected to the splanchnic plexus. No connection to heart exists at this point. LCCV, left common cardinal vein; RCCV, right common cardinal vein; UV, umbilicovitelline vein. B: Later in development, the common pulmonary vein (CPV) has evaginated from the left atrium (LA) and connected to the pulmonary venous plexus. The pulmonary veins are connected to the splanchnic plexus and the heart at this point in development. LLB, left lung bud; RLB, right lung bud. C: The connections to the splanchnic plexus involute. D: By term, the common pulmonary vein has become completely incorporated into the LA and the individual veins connect to the LA. (From Geva T, Van Praagh S. Anomalies of the pulmonary veins. In: Allen HD, Gutgesell HP, Clark EB, Driscoll DJ, eds. Moss and Adams’ Heart Disease in Infants, Children and Adolescents. 6th ed. Philadelphia, PA: Lippincott Williams & Wilkins; 2001:736–772. Originally adapted from work by R. C. Anderson, with permission.)
Subcostal Frontal (Four-Chamber) and Sagittal Views
The subcostal frontal and sagittal views offer precise imaging of the connections of the pulmonary veins, especially in infants. Likewise, these views are useful in the assessment of the atrial septum since the plane of sound is perpendicular to the plane of the septum. Frequently, a sinus venosus defect can be adequately assessed from the subcostal sagittal plane, obviating the need for alternative imaging. The subcostal sagittal view with rightward angulation offers a unique view of the right upper pulmonary vein as it travels between the superior vena cava (SVC) (anterior) and the right pulmonary artery (posterior) (Fig. 5.3A). When one rotates the transducer 90 degrees back to the frontal view, the SVC will no longer be visualized, but assessment of the right lower pulmonary vein (Fig. 5.3B) can occur. The os of the coronary sinus can also be evaluated from the subcostal frontal plane image; dilation of the coronary sinus may suggest APVC.
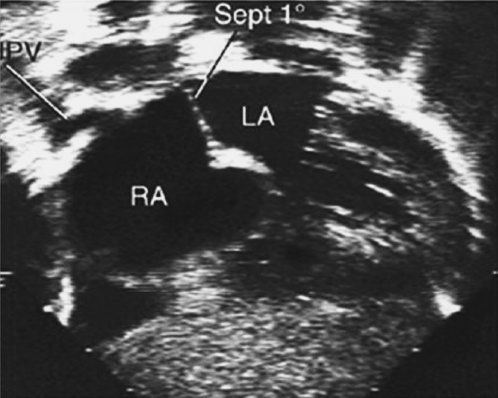
Figure 5.2. Subcostal frontal plane view (four-chamber) demonstrating normal “connection” of the right upper pulmonary vein (PV) to the left atrium (LA). However, due to malposition of the primum atrial septum (Sept 1°), the “drainage” from this vein is directed to the right atrial (RA) side of the septum.
Parasternal Long- and Short-Axis (PSLA and PSSA) Views
PSLA images with leftward angulation will demonstrate the connection of one or both left pulmonary veins to the LA. Color flow interrogation at the posterior aspect of the cardiac border can demonstrate these flows (Fig. 5.3C). PSSA images demonstrate the anterior and posterior aspects of the atrial septum. The connection of the right lower pulmonary vein to the LA can be demonstrated with rightward angulation when one focuses on the posterior edge of the atrial septum. PSSA at the level of the main pulmonary artery demonstrates the connection of the left pulmonary veins to the LA. A dilated coronary sinus may also be detected in the PSSA scans as well as the os of the coronary sinus between the tricuspid inlet and the inferior vena cava (IVC)-RA junction. The high right parasternal window offers a unique view of the relationship of the SVC and the right pulmonary veins. Figure 5.3D demonstrates three right-sided pulmonary veins connecting to the LA in a normal fashion.
Apical Four-Chamber View
The apical four-chamber image clearly demonstrates the connection of the right lower and left lower pulmonary veins (Fig. 5.3E). A common misconception is that the right upper pulmonary vein is demonstrated in this scanning plane. However, the true apical four-chamber image, which evaluates the crux of the heart and the hinge points of the atrioventricular (AV) valves, is not oriented in an anterior-to-posterior plane. Instead, the scan is entirely posterior from a superior-to-apical perspective, providing excellent imaging of the posteriorly positioned AV valves, the entrance of the IVC into the RA, and the respective lower pulmonary veins. From this view, with anterior angulation, the right upper vein connection to the dome of the LA can be visualized, but this requires one to move away from the plane of the AV valves.
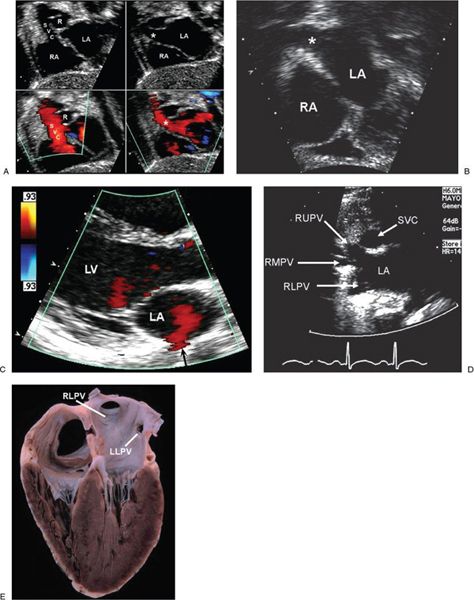
Figure 5.3. Two-dimensional imaging from multiple imaging windows. A: Quad-image from the subcostal sagittal window demonstrating the relationships of the superior vena cava (SVC), right pulmonary artery (R), atrial septum, and right upper pulmonary vein. Left: Normal connection of the SVC to the RA with color flow demonstrated toward the transducer. Right: With rightward angulation, the course of the right upper pulmonary vein (asterisk) can be demonstrated as it travels between the SVC and the RPA. B: Subcostal frontal plane view of the atrial septum and right lower pulmonary vein (asterisk). C: Parasternal long-axis image of flow from a left pulmonary vein (black arrow) entering the LA. D: High right parasternal image demonstrating the relationship of the right upper pulmonary vein (RUPV), right middle pulmonary vein (RMPV), and right lower pulmonary vein (RLPV) to the SVC as the right veins enter the LA. E: Pathologic specimen in an apical four-chamber projection demonstrating normal connection of the right lower pulmonary vein (RLPV) and left lower pulmonary vein (LLPV) to the left atrium.
Suprasternal Notch Short-Axis or “Crab View”
The “crab” view (Fig. 5.4A–C) permits the identification of all pulmonary veins connecting to the LA and should be part of all routine TTE assessments. This image usually provides excellent imaging of the normal pulmonary veins in small children. Adult echocardiography laboratories do not typically obtain this view. The Mayo Clinic congenital echocardiography laboratory demonstrated that the suprasternal notch short-axis view was obtained in 74% of 200 consecutive adult patients studied. But in this cohort, 2D and color Doppler imaging adequately demonstrated the connection of all pulmonary veins in only 46% of patients. Parameters of body habitus (body mass index, body surface area, height, and weight) did not correlate with ability to adequately evaluate the pulmonary venous connections (P. Katanyuwong, Mayo Clinic, unpublished data). In the crab view, avoid the pitfall of mistaking the LA appendage for the left upper pulmonary vein (Fig. 5.4D).
Total Anomalous Pulmonary Venous Connection
TAPVC is usually classified according to the position of the anomalous connection relative to the heart, and TAPVC is divided into four major subtypes (Fig. 5.5).
■Supracardiac
■Cardiac
■Infracardiac
■Mixed
In the supracardiac type of TAPVC, the pulmonary veins come together to form a confluence that does not enter the left side of the heart but instead enters a “vertical vein” (usually on the left side of the chest), which drains to the innominate vein (Fig. 5.6A). This is the most common type of TAPVC, accounting for 40–50% of cases in autopsy series. The anomalous vertical vein is an embryologic remnant of the splanchnic and cardinal systems. Children may come to medical attention due to an abnormal chest radiograph and enlargement of the right side of the heart. The chest radiograph is classically described as having a “snowman” appearance (Fig. 5.6B). These children generally have difficulty gaining weight and are tachypneic. In the more common form of supracardiac TAPVC, the left vertical vein originates from the pulmonary venous confluence and travels anterior to the left pulmonary artery (LPA), left mainstem bronchus, and aortic arch before it joins the innominate vein just proximal to where the left internal jugular and left subclavian veins join (Fig. 5.7). However, when the left vertical vein passes between the LPA and the left mainstem bronchus, it may become obstructed. This is referred to as a “vascular vise” (Fig. 5.8). The vertical vein is not referred to as a “left superior vena cava.” The term “left superior vena cava” should be used when a left-sided chest vessel connects the innominate vein to the coronary sinus or LA (Fig. 5.9). In cardiac TAPVC, all pulmonary veins connect to a vessel that directly enters the right atrium (usually the coronary sinus). These connections are usually unobstructed (Fig. 5.10). In infracardiac TAPVC, all of the pulmonary veins connect to a vertical vein that descends below the diaphragm (Fig. 5.11). This connection below the diaphragm occurs due to failed involution of the connection to the umbilicovitelline system. This form of TAPVC is associated with severe pulmonary hypertension and obstruction of the vertical vein as it crosses the diaphragm or enters the relatively smaller-caliber veins in or near the liver. Obstruction most commonly occurs as the infracardiac vertical vein enters the portal vein. Connection to the ductus venosus, hepatic veins, or IVC has also been observed. Infracardiac TAPVC usually requires emergent surgery in the first hours after birth. Angiography (Fig. 5.12A) or alternative imaging modalities rarely are needed to better delineate the course of the pulmonary veins before surgical repair. Infracardiac TAPVC should be suspected in newborns who present with respiratory distress and diffuse bilateral pulmonary venous congestion on chest radiography (Fig. 5.12B).
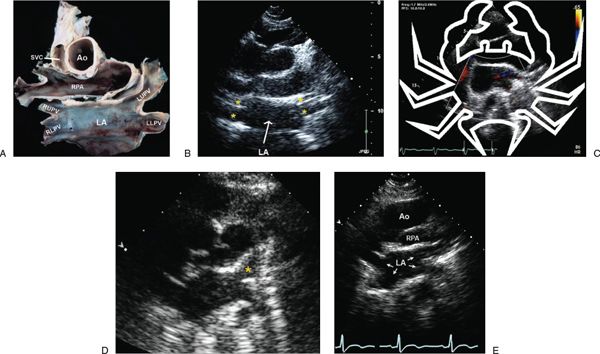
Figure 5.4. “Crab” views. A: Pathologic specimen similar to the suprasternal notch short-axis view demonstrating normal pulmonary venous connections. Coined the “crab view,” all four pulmonary veins can usually be identified from this scanning plane. This view is usually diagnostic in small children. This imaging window may not be as accessible in adults. Ao, aorta; LA, left atrium; LLPV, left lower pulmonary vein; LUPV, left upper pulmonary vein; RLPV, right lower pulmonary vein; RPA, right pulmonary artery; RUPV, right upper pulmonary vein; SVC, superior vena cava. B: Corresponding two-dimensional echocardiograph demonstrating the LA and the relative positions of the four pulmonary vein entrances (yellow asterisks). C: Diagram of the “crab” superimposed on a suprasternal short-axis image demonstrating an abnormal “crab view.” The RLPV is not demonstrated entering the LA in this patient with scimitar syndrome. D: Suprasternal short-axis view demonstrating an imaging pitfall. In this image, the yellow asterisk depicts the LA appendage and not the LUPV. E: A “true” crab view in which the pulmonary veins (arrows) are clearly identified connecting to the LA. The course of the proximal RPA just posterior to the ascending Ao is also demonstrated.
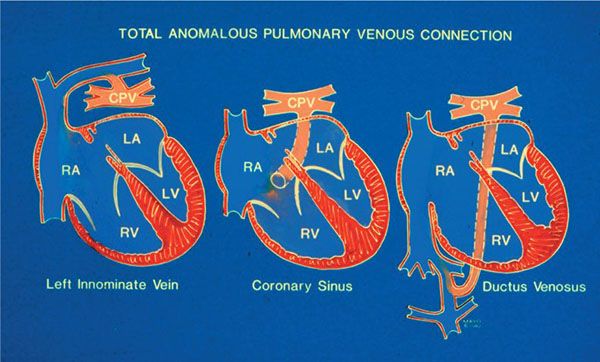
Figure 5.5. Three forms of total anomalous pulmonary venous connection (TAPVC): supracardiac type (left), cardiac type to the coronary sinus (middle), infracardiac type (right). CPV, pulmonary venous confluence.
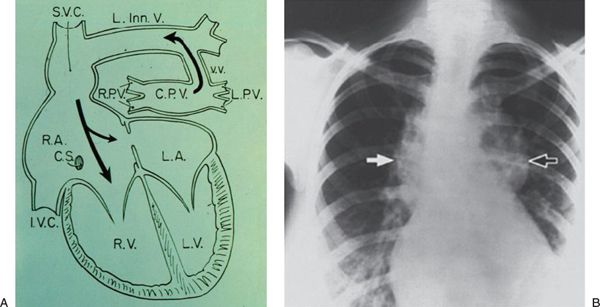
Figure 5.6. Supracardiac total anomalous pulmonary venous connection (TAPVC). A: Diagram depicting supracardiac TAPVC. The respective right (RPV) and left (LPV) pulmonary veins connect to a confluence (CPV) that is superior to the dome of the left atrium (LA). The pulmonary venous confluence connects to a dilated vertical vein (VV). In turn, the vertical vein connects to the left innominate vein (L Inn. V) and ultimately the superior vena cava (SVC). Both the SVC and innominate vein will appear dilated. CS, coronary sinus; IVC, inferior vena cava. B: Chest radiograph in a child with supracardiac TAPVC demonstrating the “snowman” sign. The left-sided mediastinal shadow (black arrow) is the dilated VV. The right-sided mediastinal shadow (white arrow) is the dilated SVC.
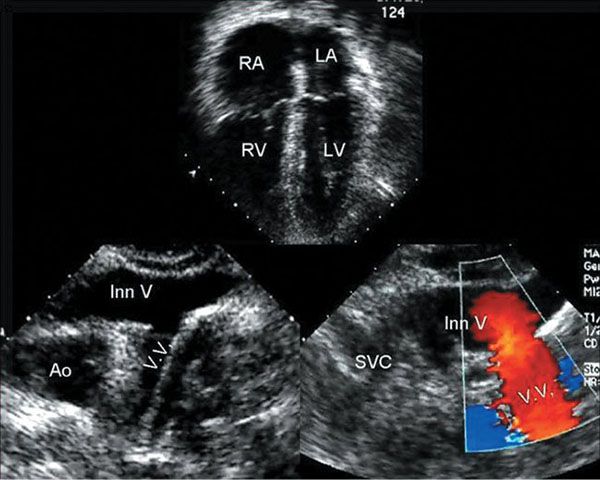
Figure 5.7. More common anatomic form of supracardiac total anomalous pulmonary venous connections (TAPVC). Top: Apical four-chamber view demonstrating right atrial (RA) and right ventricular (RV) dilation in a child with supracardiac TAPVC. Bottom left: Two-dimensional suprasternal notch image of a left-sided vertical vein (VV) connecting to the innominate vein (Inn V). Ao, aorta. Bottom right: Color Doppler image in the same plane demonstrating cephalad (red) flow in the vertical vein as it joins the innominate vein. SVC, superior vena cava.
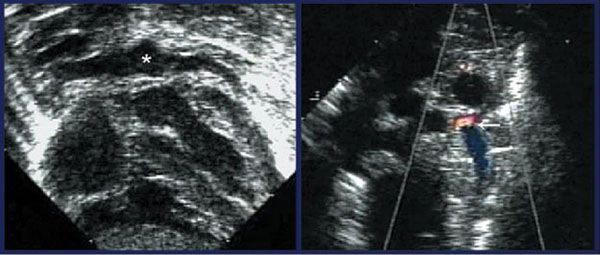
Figure 5.8. “Vascular vise.” Left: Subcostal coronal image demonstrating the pulmonary venous confluence (asterisk) with the appearance of a “hat” on top of the superior aspect of the left atrium (LA). Right: Suprasternal short-axis view with color Doppler demonstrating a left vertical vein with aliased flow (arrow) at the point of a “vascular vise.” The vertical vein is partially obstructed as it passes between the left mainstem bronchus and the left pulmonary artery.
The diagnosis of infracardiac TAPVC may be particularly challenging in the premature newborn with lung disease. The signs and symptoms may be misinterpreted as persistent pulmonary hypertension. Echocardiographic imaging can be especially difficult if the patient is intubated and requires aggressive ventilator management. Clear 2D images of the pulmonary veins may be limited. In these patients, both color and spectral Doppler techniques need to be extensively used to ensure that flow from the pulmonary veins is demonstrated into the LA. In some situations, these neonates deteriorate rapidly. Resuscitation may include extracorporeal membrane oxygenation (ECMO). If the diagnosis of TAPVC is not established before initiation of ECMO, it may be difficult to wean the child from the circuit. In these circumstances, an alternative imaging method, such as angiography, may be useful to discover obstructed infracardiac TAPVC. Relief of pulmonary venous obstruction is needed to wean from ECMO.
The fourth and least common type of TAPVC is generically referred to as “mixed.” This form represents a combination of at least two of the other types. In the mixed form of TAPVC, there is no true pulmonary venous confluence. Imaging errors can easily be made in this situation. Unilateral obstruction may occur and patients with heterotaxy syndromes are predisposed to the mixed form of TAPVC. Patients with heterotaxy syndromes with situs ambiguous of the atria may have “ipsilateral” anomalous pulmonary veins, wherein the right and left veins connect to their respective sides of a common atrium.
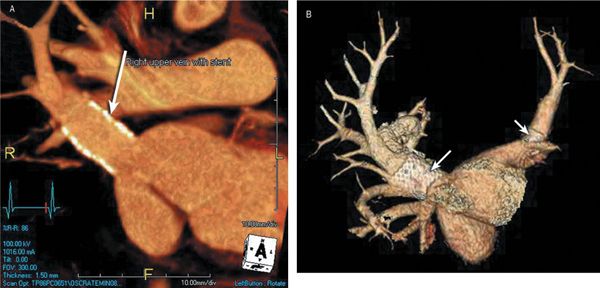
Figure 5.9. Pulmonary vein stent placement. 3D CT reconstruction images in a young adult who was born with TAPVC to the coronary sinus. After neonatal repair he developed bilateral pulmonary vein stenosis. He required multiple surgical revisions and cath lab interventions. This ultimately resulted in stent placement to relieve obstruction in the left atrial appendage/left pulmonary vein connection and in the reconstructed right pulmonary vein confluence (A and B: arrows). He struggled with elevated RV systolic pressures through much of his young life but eventually achieved normal RV pressures after the most recent intervention at age 17 years.
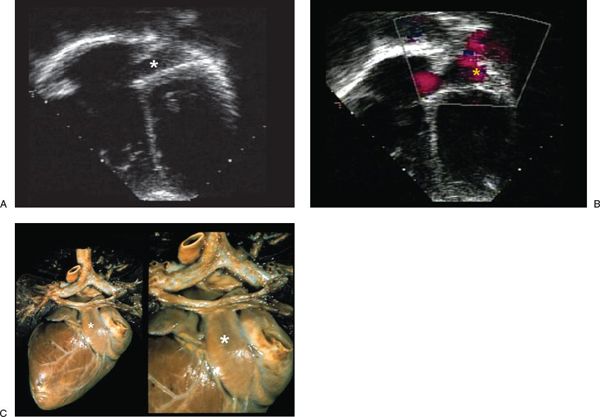
Figure 5.10. Dilated coronary sinus. A: Apical four-chamber scan demonstrating a dilated coronary sinus (asterisk) in a patient with anomalous pulmonary venous connection to the coronary sinus. B: Color Doppler image in the same projection as A, demonstrating antegrade flow in the coronary sinus (yellow asterisk). C: Pathologic specimen from a posterior view demonstrating a pulmonary venous confluence connecting to a dilated coronary sinus (asterisk) in a cardiac form of total anomalous pulmonary venous connections (TAPVC).
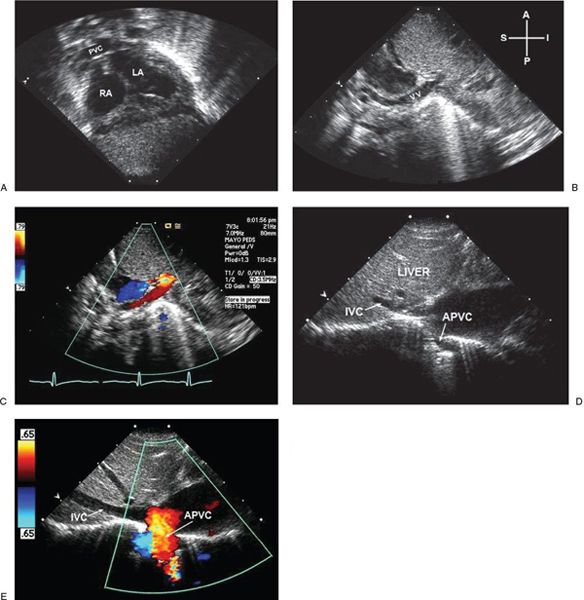
Figure 5.11. Newborn patient with mild cyanosis and tachypnea. A: The pulmonary venous confluence (PVC) fails to connect to the dome of the left atrium (LA). B: A vertical vein (VV) in this patient descends below the diaphragm and enters the liver, where it is partially obstructed. C: Color Doppler image in the same projection as B, demonstrating flow from the vertical vein into the liver (red). D: Two-dimensional image in a different patient demonstrating an anomalous pulmonary vein (APVC) entering the right atrium (RA)–inferior vena cava (IVC) junction. E: Color Doppler of the patient in D demonstrating flow from the APVC into the RA–IVC junction.
Partial Anomalous Pulmonary Venous Connections
PAPVC, first described by Winslow in 1739, is an uncommon congenital anomaly found in 0.4% to 0.7% of autopsy series, therefore the true incidence may be higher. Both TTE and TEE have major roles in the detection of PAPVC. Echocardiography is important in the evaluation of associated hemodynamic changes such as volume overload of the right heart chambers, tricuspid regurgitation, and pulmonary hypertension. Children with PAPVC may be asymptomatic and escape detection until adulthood. When symptomatic, patients with PAPVC present with dyspnea, fatigue, atrial arrhythmia, pulmonary hypertension, unexplained cardiomegaly on chest radiograph, or unexplained right ventricular volume overload on TTE. PAPVC can be an isolated defect with an intact atrial septum or associated with a PFO or ASD. PAPVC is associated with 85% of patients with sinus venosus defects. In addition, PAPVC has been associated with AV septal defect, tetralogy of Fallot, congenitally corrected transposition and Turner syndrome.
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


