Anatomy of the Thoracic Duct and Chylothorax
David W. Johnstone
The lymphatic system is derived from the venous system. In the embryo, the cisterna chyli and bilateral jugular lymphatic sacs anastomose to form the thoracic duct. The thoracic duct is initially a bilateral structure, which usually joins to form a single duct system.41 This pattern of maturation leads to anatomic variations; the standard pattern is found in only 65% of humans.13
Anatomy of the Thoracic Duct
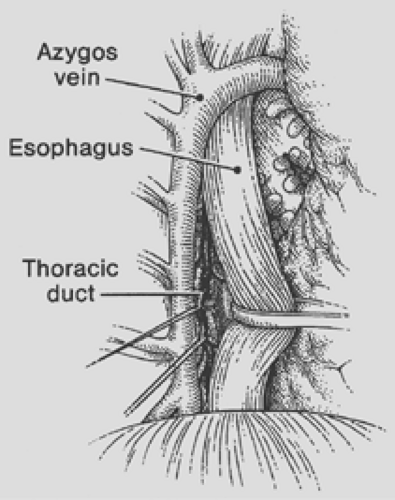
The usual course of the thoracic duct is illustrated in Figure 66-1. The thoracic duct is the common channel draining lymphatic fluid from the body to the venous system with the exception of the right face and neck, right arm, right thorax and lung, and convex surface of the liver. The thoracic duct originates in the cisterna chyli anterior to the second lumbar vertebra (range T10–L3), passes through the aortic hiatus, and ascends posterior to the esophagus between the aorta and the azygos vein to the right of the midline (Fig. 66-2). At the fifth or sixth thoracic vertebra, the duct crosses to the left posterior to the aortic arch and origin of the left subclavian artery and passes to the thoracic inlet along the left side of the esophagus. The duct receives tributaries from the bronchomediastinal trunk before exiting the mediastinum. Once the duct enters the neck, it arches laterally at the C7 level anterior to the subclavian artery and thyrocervical arteries. It continues superficial to the phrenic nerve and the scalenus anticus muscle, passes behind the left carotid sheath and jugular vein, and terminates into the posterior confluence of the left jugular and subclavian veins. This termination may be as single (80%) or multiple trunks (20%).27,45 The duct has valves at various points along its course.
Lymph from the right side of the head, neck, and chest wall as well as from the right lung drains into the right lymphatic duct. This duct also carries lymph from the heart and the dome of the liver and from the right diaphragm. The right lymphatic trunk typically has its major drainage into the posterior junction of the right subclavian and jugular veins; this duct is small and rarely seen.4
Major Variations of the Thoracic Duct
Variations occur in nearly half the cases studied, generally consisting of multiple mediastinal trunks, variable crossover levels, and variable drainage of accessory trunks from the right chest, arm, and head.1,13,53 Major variations include doubling (5%–40% depending on extent), left-sidedness, right-sided or bilateral termination (2%), and rare azygos vein termination. The duct may also pass posterior to the vertebral and subclavian arteries en route to its venous termination. Multiple studies of the duct termination indicate that variation is the rule: <40% join the left venous confluence, with most other variations consisting of termination into the subclavian and jugular veins, or combinations.46
Composition of Chyle
The term chyle derives from the Latin chylus, meaning juice. Of the fluid traversing the thoracic duct in a healthy person, nearly all originates in the intestines and liver. The primary physiologic role of the cisterna chyli and thoracic duct is to deliver digestive fat to the venous system. Approximately 60% of ingested fat reaches the bloodstream via the thoracic duct. Fat from intestinal absorption gives chyle its characteristic milky appearance. Consequently chyle appears serous in the fasting state.
The composition of chyle is summarized in Table 66-1. Concentrations of fat, protein, and lymphocytes vary considerably depending on the timing, composition, and amount of food ingested.
The fat in thoracic duct lymph is composed of neutral fat, free fatty acids, sphingomyelin, phospholipids, cholesterol, and cholesterol esters. Fatty acids of <10 carbon atoms are absorbed directly into the portal system and therefore largely bypass the lymphatic circulation. For that reason, a diet restricting fat to medium-chain triglycerides (MCTs) has been used to reduce thoracic duct flow. Ingested fat passes from the intestine to the systemic circulation over approximately 1.5 hours, with peak absorption 6 hours after ingestion.
The main cellular elements of thoracic duct lymph are lymphocytes, predominantly T lymphocytes.25 Thoracic duct lymphocytes differ from peripheral blood lymphocytes in their reactivity to antigenic stimulation. Fat-soluble vitamins, antibodies, enzymes, and urea nitrogen are present in thoracic duct lymph. In addition to chyle, the thoracic duct transports excess tissue fluid, extravasated proteins, and other macromolecules from the interstitium to the venous system.
Chyle is bacteriostatic, probably owing to its high fatty acid content. Its specific gravity and alkaline pH result in very little pleural reaction.
Table 66-1 Composition of Chyle | ||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| ||||||||||||||||||||||||||||||||
Physiology of the Thoracic Duct
The flow of lymph in the thoracic duct has been estimated to be 1.38 mL/kg of body weight per hour, varying between 30 and 190 mL/hr.46 Flow increases after ingestion of food and water and during abdominal massage.12 Hepatic lymph increases by 150% after meals, whereas the basal intestinal lymph flow may increase 10-fold after fatty meals.4 Volumes up to 2,500 mL of chyle in 24 hours have been collected from the cannulated human thoracic duct. Starvation and complete rest decrease the flow of thoracic duct lymph.
The inflow of chyle into the lacteal system is driven by absorption of intestinal food and liquid and is augmented by intestinal contractions. The negative transdiaphragmatic pressure gradient helps upward flow of chyle. Muscular contractions of the duct wall occur every 10 to 15 seconds independent of respiratory movements. The intraductal pressure ranges from 10 to 25 cm H2O; with obstruction, it may increase to 50 cm H2O.44 The thoracic duct’s valves, located throughout its course but mostly in the upper portion, promote upward flow.
Causes of Chylothorax
A chylothorax is the presence of lymphatic fluid in the pleural space. Its causes can be broadly grouped into congenital, traumatic, and neoplastic (Table 66-2).
Congenital Chylothorax
Congenital, or primary, chylothorax is the most common cause of pleural effusion in the neonatal period.8 It presents at birth or during the first weeks of life as respiratory distress. Most cases are
idiopathic. Chylothorax is associated with syndromes involving abnormal lymphatic development. The thoracic duct may be absent or atretic, or it may have multiple dilatated lymphatic channels with abnormal communications including fistulas to the pleural space. Birth trauma, including hyperextension of the neck, and conditions elevating pressure in the superior vena cava, may be causes as well.3
idiopathic. Chylothorax is associated with syndromes involving abnormal lymphatic development. The thoracic duct may be absent or atretic, or it may have multiple dilatated lymphatic channels with abnormal communications including fistulas to the pleural space. Birth trauma, including hyperextension of the neck, and conditions elevating pressure in the superior vena cava, may be causes as well.3
Table 66-2 Etiology of Chylothorax | ||
|---|---|---|
|
Treatment of congenital chylothorax is generally conservative, with expectation of resolution in 4 to 5 weeks. Continued breast feeding has not prevented resolution in many cases, though MCT diet or parenteral nutrition may be needed in refractory cases. Thoracentesis is appropriate for initial relief of respiratory distress; pleuroperitoneal shunting is preferred in absence of ascites; thoracic duct ligation and/or pleurodesis may be required in some cases.3
Traumatic Chylothorax
Chylothorax may occur following blunt or penetrating trauma. The most common form of nonpenetrating injury to the thoracic duct is produced by sudden hyperextension of the spine with rupture of the duct just above the diaphragm. Sudden stretching over the vertebral bodies may be enough in itself to tear the duct, but usually the duct has been fixed as a result of prior disease or malignancy. Vomiting or violent coughing also can result in tearing of the thoracic duct.5 Penetrating trauma to the thoracic duct is unusual and is typically of lower priority than other associated injuries.
Surgical Injuries
Injury to the thoracic duct can occur during any operation in the vicinity of the mediastinum or lower neck. Chylothorax has been reported following most types of thoracic procedures. The duct is at particular risk during esophagectomy, aortic operations, coarctation repair, ligation of patent ductus arteriosus, left pneumonectomy, removal of posterior mediastinal tumors, and sympathectomy. Chylothorax may also complicate radical neck dissections, abdominal sympathectomy, and lymph node dissections. Occasional chylothorax following central venous cannulation may be due to venous occlusion rather than direct injury to the duct.31
Awareness of the typical ductal anatomy and its variability combined with vigilance when working in areas at risk is the best strategy for avoiding damage. Injury to the duct is often unrecognized intraoperatively because patients have not had oral intake for many hours and the duct lymph is serous. Diagnosis of postoperative chylothorax is thus delayed by days. Injuries to the duct below the T6 level tend to present on the right and those above that level tend to present on the left.
The incidence of chylothorax following esophagectomy varies between 0.5% and 3.4% in large contemporary reports and does not clearly depend on the approach chosen. Orringer36 reported <1% incidence in 1,085 patients undergoing transhiatal esophagectomy. Dugue17 reported a 2.7% incidence among 850 patients undergoing Ivor-Lewis esophagectomy. A report of 1,787 esophagectomies performed with a 1.1% incidence of chylothorax found no difference between transthoracic and transhiatal approaches (1% of 1,237 patients versus 1.3% of 464 patients, respectively).30 A meta-analysis of 44 published reports found a 2.1% incidence among 2,675 transhiatal esophagectomies and a 3.4% incidence among 2,808 Ivor–Lewis esophagectomies.39
Chylothorax following pulmonary resection is unusual. In a large retrospective study from the Mayo Clinic, over 11,000 patients who underwent thoracic surgical procedures included 47 (0.42%) who developed a postoperative chylothorax.7 Thirteen of these patients had undergone a pulmonary resection. Sarsam42 reported that chylothorax developed in 9 of 1,800 patients (0.5%) who underwent pneumonectomy. Terzi50 reported 13 chylothoraces occurring among 1,744 patients after pleuropulmonary surgery (0.74%). The majority of cases occur after pneumonectomy, extensive lymphadenectomy, sleeve resections, or other resections involving more extensive dissection in the hilum and paratracheal area.21,24
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree