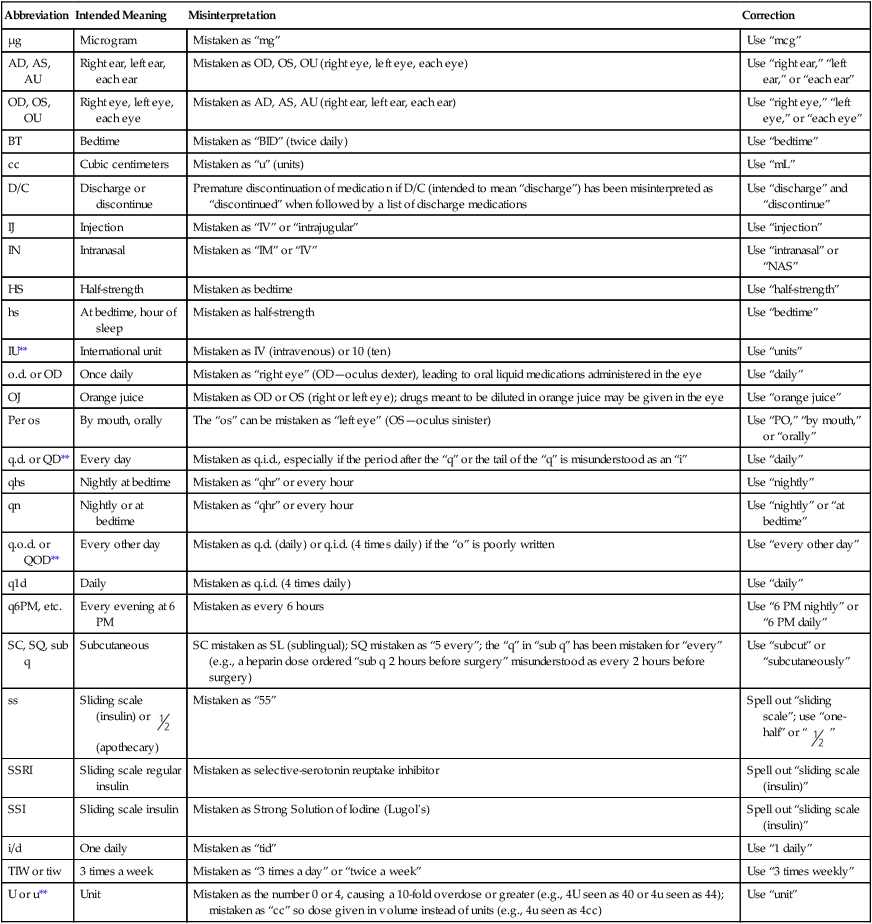
2. Describe the three phases that constitute the course of drug action from dose to effect. 3. Describe the classes of drugs that are delivered via the aerosol route. 4. Compare the available aerosol formulations, brand names, and dosages for each specific drug class. 5. Select the appropriate drug class for a given patient or clinical situation. The primary objective of airway pharmacology is the delivery of inhaled aerosols to the respiratory tract for the diagnosis and treatment of pulmonary diseases. Because the administration of medications is such an important part of the daily activities of a respiratory therapist (RT), a deep understanding of them is essential. How medications work is an important part of the assessment process and in choosing the right medication to treat the pulmonary needs of your patients. Three phases constitute the course of drug action from dose to effect: (1) the drug administration phase, (2) the pharmacokinetic phase, and (3) the pharmacodynamic phase. These three phases of drug action may be applied to treatment of the respiratory tract with bronchoactive inhaled agents and are defined in Box 18-1. Devices that are most commonly used to administer orally inhaled aerosols are the metered-dose inhaler (MDI), the small-volume nebulizer (SVN), and the dry-powder inhaler (DPI). They will be discussed in more detail in Chapter 19. With RTs being responsible for the administration of numerous pulmonary medications, it may be a complex and demanding part of their daily responsibilities. Patients may be receiving several different inhaled medications during their hospital stay. Consequently, it is important to always practice safe medication administration. In the United States, The Joint Commission (TJC) accredits health care organizations, and improving patient safety must be a constant goal of the organizations. Medication safety aspects of the national patient safety goals are listed in Box 18-2. Safe medication administration begins with the six rights of medication administration: Regardless of how you receive an order (verbal, written, protocol), you should always compare it with the medication administration record (MAR; eMAR for electronic versions) to ensure that the right medication is being administered. Many respiratory medications come in ampoules with measured doses. This does not negate the responsibility of the therapist to confirm that the right dose is being given. Concentration differences and the addition of a combination medication may result in a dose error if the RT is not careful. Two patient identifiers are mandatory before giving medication to a patient. The majority of respiratory medications are given via aerosolization. However, the order always has a designated route. The RT should assess the patient and make sure that the ordered route is the best for the patient’s current condition. The Institute for Safe Medication Practice (ISMP) compiled a list of error-prone abbreviations. Table 18-1 lists some abbreviations that are commonly misinterpreted. The right time for respiratory medications to be delivered may help the patient control his or her symptoms, as with delivery of inhaled corticosteroids, or used to relieve current complaints such as shortness of breath caused by bronchospasm. TABLE 18-1 Institute for Safe Medication Practice List of Error-Prone Abbreviations* *These abbreviations, symbols, and dose designations have been reported to ISMP though the USP-ISMP Medication Error Reporting Program for being frequently misinterpreted and involved in harmful medication errors. They should never be used when communicating medical information. The Joint Commission has established a National Patient Safety Goal that specifies that certain abbreviations must appear on an accredited organization’s do-not-use list; those items are indicated with a double asterisk (**). These abbreviations are included on The Joint Commission’s “minimum list” of dangerous abbreviations, acronyms, and symbols that must be included on an organization’s “Do Not Use” list, effective January 1, 2004. Report medication errors or near misses to the ISMP Medicaton Errors Reporting (MERP) at 1-800-FAILSAF(E) or online at www.ismp.org. Used with permission, Institute for Safe Medication Practice (ISMP): http://www.ismp.org. 1. Review the patient’s chart. 2. Verify the physician’s order or the facility’s protocol for standard of care. 3. Compare the order with the MAR or the eMAR. 4. Avoid any distractions during medication preparation. 5. Read the label on the medication container, and compare the instructions with the MAR three times:
Airway Pharmacology
Equipment
» Skill Check Lists
18-1 Medication Administration
Abbreviation
Intended Meaning
Misinterpretation
Correction
µg
Microgram
Mistaken as “mg”
Use “mcg”
AD, AS, AU
Right ear, left ear, each ear
Mistaken as OD, OS, OU (right eye, left eye, each eye)
Use “right ear,” “left ear,” or “each ear”
OD, OS, OU
Right eye, left eye, each eye
Mistaken as AD, AS, AU (right ear, left ear, each ear)
Use “right eye,” “left eye,” or “each eye”
BT
Bedtime
Mistaken as “BID” (twice daily)
Use “bedtime”
cc
Cubic centimeters
Mistaken as “u” (units)
Use “mL”
D/C
Discharge or discontinue
Premature discontinuation of medication if D/C (intended to mean “discharge”) has been misinterpreted as “discontinued” when followed by a list of discharge medications
Use “discharge” and “discontinue”
IJ
Injection
Mistaken as “IV” or “intrajugular”
Use “injection”
IN
Intranasal
Mistaken as “IM” or “IV”
Use “intranasal” or “NAS”
HS
Half-strength
Mistaken as bedtime
Use “half-strength”
hs
At bedtime, hour of sleep
Mistaken as half-strength
Use “bedtime”
IU**
International unit
Mistaken as IV (intravenous) or 10 (ten)
Use “units”
o.d. or OD
Once daily
Mistaken as “right eye” (OD—oculus dexter), leading to oral liquid medications administered in the eye
Use “daily”
OJ
Orange juice
Mistaken as OD or OS (right or left eye); drugs meant to be diluted in orange juice may be given in the eye
Use “orange juice”
Per os
By mouth, orally
The “os” can be mistaken as “left eye” (OS—oculus sinister)
Use “PO,” “by mouth,” or “orally”
q.d. or QD**
Every day
Mistaken as q.i.d., especially if the period after the “q” or the tail of the “q” is misunderstood as an “i”
Use “daily”
qhs
Nightly at bedtime
Mistaken as “qhr” or every hour
Use “nightly”
qn
Nightly or at bedtime
Mistaken as “qhr” or every hour
Use “nightly” or “at bedtime”
q.o.d. or QOD**
Every other day
Mistaken as q.d. (daily) or q.i.d. (4 times daily) if the “o” is poorly written
Use “every other day”
q1d
Daily
Mistaken as q.i.d. (4 times daily)
Use “daily”
q6PM, etc.
Every evening at 6 PM
Mistaken as every 6 hours
Use “6 PM nightly” or “6 PM daily”
SC, SQ, sub q
Subcutaneous
SC mistaken as SL (sublingual); SQ mistaken as “5 every”; the “q” in “sub q” has been mistaken for “every” (e.g., a heparin dose ordered “sub q 2 hours before surgery” misunderstood as every 2 hours before surgery)
Use “subcut” or “subcutaneously”
ss
Sliding scale (insulin) or  (apothecary)
(apothecary)
Mistaken as “55”
Spell out “sliding scale”; use “one-half” or “  ”
”
SSRI
Sliding scale regular insulin
Mistaken as selective-serotonin reuptake inhibitor
Spell out “sliding scale (insulin)”
SSI
Sliding scale insulin
Mistaken as Strong Solution of Iodine (Lugol’s)
Spell out “sliding scale (insulin)”
i/d
One daily
Mistaken as “tid”
Use “1 daily”
TIW or tiw
3 times a week
Mistaken as “3 times a day” or “twice a week”
Use “3 times weekly”
U or u**
Unit
Mistaken as the number 0 or 4, causing a 10-fold overdose or greater (e.g., 4U seen as 40 or 4u seen as 44); mistaken as “cc” so dose given in volume instead of units (e.g., 4u seen as 4cc)
Use “unit”
Procedural Preparation
![]()
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


Airway Pharmacology











