12 Airway Management
Note 1: This book is written to cover every item listed as testable on the Entry Level Examination (ELE), Written Registry Examination (WRE), and Clinical Simulation Examination (CSE).
The listed code for each item is taken from the National Board for Respiratory Care’s (NBRC) Summary Content Outline for CRT (Certified Respiratory Therapist) and Written RRT (Registered Respiratory Therapist) Examinations (http://evolve.elsevier.com/Sills/resptherapist/). For example, if an item is testable on both the ELE and the WRE, it will simply be shown as: (Code: …). If an item is only testable on the ELE, it will be shown as: (ELE code: …). If an item is only testable on the WRE, it will be shown as: (WRE code: …).
MODULE A
1. Assess the patient’s airway by inspection
a. Inspect the patient’s face to identify the presence of macroglossia (Code: IB1b) [Difficulty: ELE: R, Ap; WRE: An]
Macroglossia is an excessively large tongue that is often seen to protrude out of the mouth (Figure 12-1). It can partially obstruct the neonate’s upper airway and may be associated with inspiratory stridor. Macroglossia is associated with Down syndrome, Beckwith-Wiedemann syndrome, and several metabolic disorders. Immediate treatment may require (1) manually moving the mandible forward to pull the large tongue out of the airway, (2) inserting an oropharyngeal airway or nasopharyngeal airway, (3) placing the infant in the prone position. If the infant has life-threatening airway obstruction that is not corrected by these procedures, an endotracheal tube or tracheostomy tube must be inserted. Long-term management may require a tracheostomy or corrective facial surgery.
b. Assess for limits in neck range of motion (Code: IB1b) [Difficulty: ELE: R, Ap; WRE: An]
Other people with limited neck range of motion include a patient who has recently had cervical spine surgery and is being weaned from a neck brace or a patient with kyphoscoliosis who is wearing a supportive brace. If a patient wearing a neck brace has an upper airway obstruction, it may be possible to insert an oropharyngeal airway or nasopharyngeal airway to push the tongue forward to ease breathing. If these devices are not effective, and the neck cannot be hyperextended to open the airway, an emergency airway is needed. It is possible that a laryngeal mask airway (LMA) or Combitube could be inserted by an emergency medical technician, paramedic, or respiratory therapist. If these devices are not able to provide a secure airway, a physician will need to perform nasotracheal intubation or a tracheostomy (see Chapter 18).
2. Properly position the patient
b. Properly position the patient to maintain a patent airway (Code: IIIB1) [Difficulty: ELE: R, Ap; WRE: An]
Positioning of the head to open the airway is discussed in Chapter 11. Briefly, use the head tilt-chin lift maneuver to hyperextend the neck of an adult, and slightly extend the neck of a child to open the airway. You can place a small pad behind the neck and head to put the patient in the “sniff position.” Always keep the head in line with the body. If the patient has a known or suspected cervical spine injury, the neck cannot be hyperextended. Instead, open the airway with the jaw-thrust maneuver. Keep the head in line with the body.
3. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
4. Humidify an artificial airway
a. Maintain adequate humidification to the patient’s airway (ELE code: IIIB8) [Difficulty: ELE: R, Ap, An]
MODULE B
1. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
2. Manipulate oropharyngeal airways by order or protocol (ELE code: IIA7a) [Difficulty: ELE: R, Ap, An]
a. Get the necessary equipment
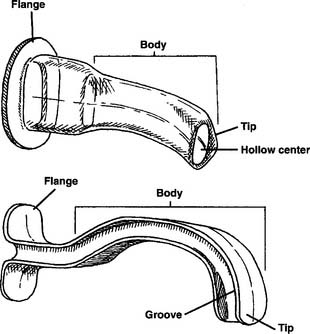
The oropharyngeal airway (or bite block) is made of plastic that is hard enough to withstand any patient’s biting force. A properly sized and placed oropharyngeal airway lifts the tongue forward from the posterior portion of the oropharynx to keep a patent airway and make suctioning oral secretions easier. An oropharyngeal airway is poorly tolerated in a conscious patient and can cause gagging and even vomiting. Oropharyngeal airways are available in a variety of sizes that fit infants or adults. The proper size is found by holding the airway against the patient’s face with the flange against the lips. The end of the airway should reach the angle of the jaw (Figure 12-2). Too large an airway can block the oropharynx by extending past the tongue. An airway that is too small can push the tongue back into the oropharynx rather than pulling the tongue forward, as intended. Figure 12-3 shows a properly placed and sized oropharyngeal airway.
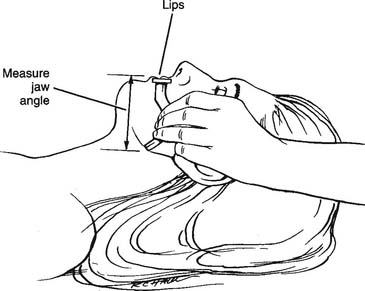
Figure 12-2 Procedure for measuring the proper size of the oropharyngeal airway.
(From Eubanks DH, Bone RC: Comprehensive respiratory care, ed 2, St Louis, 1990, Mosby.)
A number of manufacturers make oropharyngeal airways, which fall into two basic types: hollow center and I-beam (Figure 12-4).
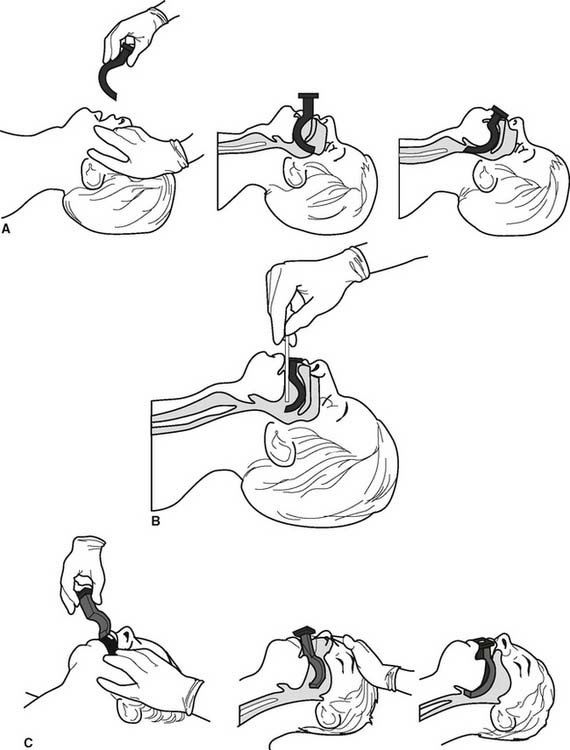
d. Insert the correct oropharyngeal airway (ELE Code: IIIB2) [Difficulty: ELE: R, Ap, An]
There are three widely used methods to insert an oropharyngeal airway.
1. First method
MODULE C
1. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
2. Manipulate nasopharyngeal airways by order or protocol (ELE code: IIA7a) [Difficulty: ELE: R, Ap, An]
a. Get the necessary equipment
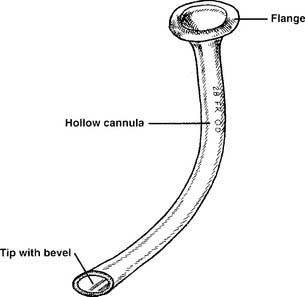
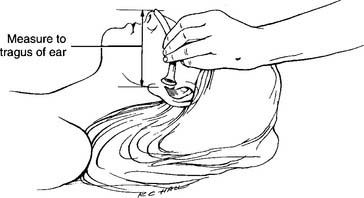
See Figure 12-5 for a close-up of a nasopharyngeal airway. All nasopharyngeal airways have a flange that fits close to the patient’s nostril. This prevents the entire tube from being pushed into the patient. All nasopharyngeal airways have a cannula with a channel for breathing or suctioning. Nasopharyngeal airways are available in a variety of sizes for adults. They can be properly sized by measuring from the tip of the nose to the tragus of the ear and adding 2 to 3 cm (Figure 12-6).
b. Put the equipment together and make sure that it works properly
All nasopharyngeal airways are made up of a single piece. There is nothing to assemble.
c. Troubleshoot any problems with the equipment
Make sure that the tube is not plugged by dried secretions, blood, or a foreign body. If plugged, the patient cannot breathe through it, and a suction catheter cannot be passed through it. Remove a plugged nasopharyngeal airway.
d. Insert the correct nasopharyngeal airway (ELE Code: IIIB2) [Difficulty: ELE: R, Ap, An]
The following steps are taken to insert a nasopharyngeal airway:
e. Assess the nasopharyngeal tube placement (ELE code: IIIB5) [Difficulty: ELE: R, Ap, An]
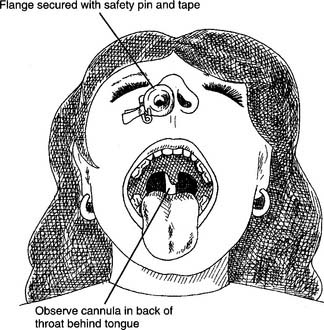
Check the placement by looking into the patient’s mouth with a flashlight and tongue depressor. A properly placed nasopharyngeal airway can be seen in the oropharynx and extends behind the tongue (Figures 12-7 and 12-8). The placement should be checked each time a tube is replaced or moved from one nostril to the other. If a nasopharyngeal tube is inserted too deeply, it can block the glottis opening into the trachea.
MODULE D
1. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
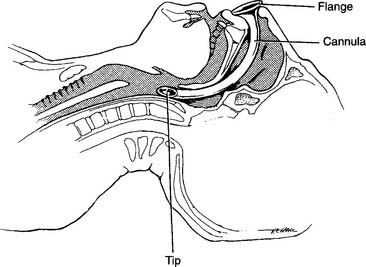
A laryngeal mask airway (LMA) is composed of a modified endotracheal tube with a standard 15-mm-outer diameter (OD) adapter (for attaching a resuscitation bag or ventilator circuit) at the proximal end and a silicone laryngeal mask at the distal end. The mask is inflated by attaching a syringe to the one-way valve and pilot balloon on an inflation tube, in the same manner as an endotracheal tube cuff (Figure 12-9). When the mask is inflated it surrounds and seals the larynx. LMAs were first used in the operating room by anesthesiologists. Their use has been expanded; today, emergency medical personnel and respiratory therapists use LMAs as an alternative to endotracheal tubes or Combitubes in patients with a difficult airway or during a CPR effort. Experience has shown that an LMA can be easily and quickly inserted without any additional equipment. Patients with asthma or irritable airways will have less coughing or bronchospasm than if an endotracheal tube were inserted. It has been shown that ventilating a patient with a resuscitation bag to an LMA is as effective or better than bag-mask ventilation. See Box 12-1 for indications, contraindications, and limits to an LMA.
BOX 12-1 Indications, Contraindications, and Limits of a Laryngeal Mask Airway
INDICATIONS
CONTRAINDICATIONS
Remember that an LMA does not provide as secure an airway as an endotracheal tube. There are two limitations to using an LMA. First, the LMA does not absolutely protect against aspiration. Second, tidal volume gas can leak if mechanical ventilation pressures are greater than 20 cm H2O. This can lead to a smaller than desired tidal volume and/or gas being forced into the stomach. Excessive air in the stomach can cause vomiting. If either of these possibilities is of paramount clinical concern, the patient should have an endotracheal tube inserted rather than an LMA.
2. Manipulate laryngeal mask airways by order or protocol (Code: IIA7f) [Difficulty: ELE: R, Ap; WRE: An]
a. Get the necessary equipment
Several manufacturers make standard LMAs like that shown in Figure 12-9. In addition, there are two commonly seen modifications. The first is an LMA that facilitates tracheal intubation by easily allowing an endotracheal tube to slide through its lumen. The second is an LMA that includes a port for gastric suction to vent any air in the stomach. Adjunct supplies include a watersoluble lubricant for the laryngeal mask, syringe to inflate the mask, and protective gear for the practitioner, such as a face mask and gloves.
3. Assess the placement of the LMA (ELE code: IIIB5) [Difficulty: ELE: R, Ap, An]
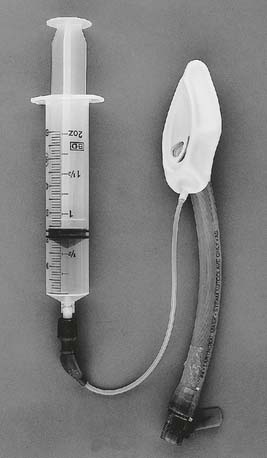
While the NBRC does not list the insertion of an LMA as a testable item, proper placement is needed to ensure that it can be correctly maintained in the airway. Figure 12-10 shows the procedure for inserting an LMA and how the inflated mask covers the laryngeal inlet (glottis opening into the trachea). When the properly sized LMA is being placed, it is gently advanced until resistance is felt. (If the LMA is too small, no resistance will be felt since it will slide into the esophagus.) The distal tip of the mask will stop at the upper esophageal sphincter. The cuff is then inflated to cover the tracheal opening and seal off the esophagus. (Later, the cuff pressure can be measured; it should not exceed 60 cm H2O.) Manually ventilate the patient’s lungs with a resuscitation bag. The following steps should be taken to ensure that the LMA is properly placed to cover the opening to the trachea: (1) when the LMA mask is inflated, the tube will move out of the mouth about 1 to 2 cm; (2) auscultate for equal, bilateral breath sounds; (3) auscultate for the absence of sounds over the stomach; (4) an end-tidal carbon dioxide monitor should show exhaled CO2.
MODULE E
1. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
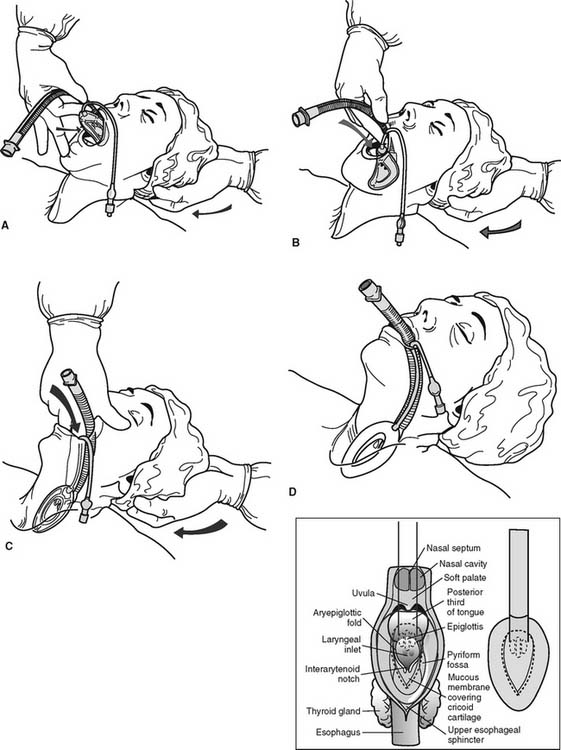
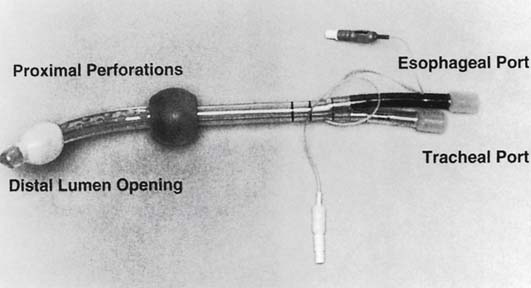
The Combitube (also known as the esophageal-tracheal Combitube or ETC) is a double-lumen tube that can be used to ventilate a patient whether the tube is placed into the esophagus (as intended) or trachea (Figure 12-11). The Combitube is one version of a series of tubes called esophageal obturator airways (EOAs) that are designed to be placed into the esophagus of an unconscious adult patient. Clinical experience has shown that a Combitube provides a reasonably secure airway in emergency situations, such as when performing CPR. It can be used as an alternative to an LMA. At the time this book was being published, there were five different types of EOA that provide the same two functions: ensure a stable airway for artificial ventilation and prevent vomiting and aspiration. Clinical experience with the various types of esophageal obturator airways is highly recommended because they do not appear or operate like standard endotracheal tubes. See Box 12-2 for a comparison of a Combitube with an endotracheal tube.
BOX 12-2 Indications, Contraindications, Advantages, and Disadvantages of the Combitube
ADVANTAGES
2. Manipulate a Combitube by order or protocol (Code: IIA7g) [Difficulty: ELE: R, Ap; WRE: An]
3. Assess the placement of the Combitube (ELE code: IIIB5) [Difficulty: ELE: R, Ap, An]
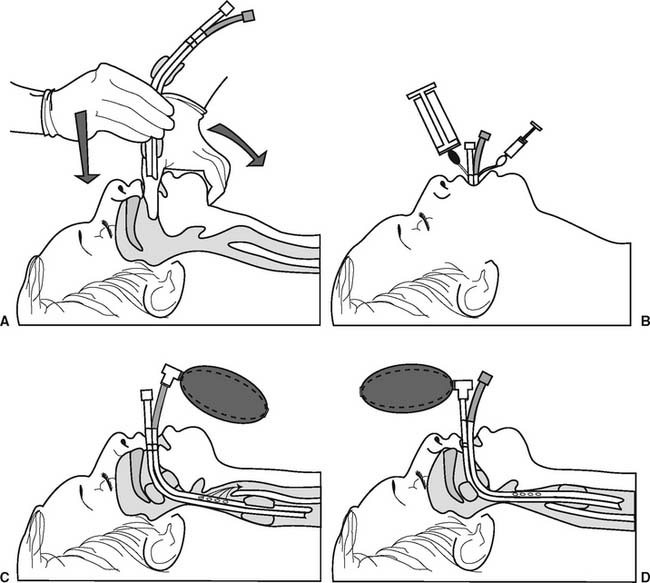
While the NBRC does not list the insertion of the Combitube as a testable item, proper placement is needed to ensure that it can be correctly maintained in the airway. Figure 12-12 shows the procedure for inserting a Combitube. When the tube enters the esophagus as intended, both cuffs are inflated, and the patient is ventilated through the longer, colored tube, bilateral breath sounds will be heard (see Figure 12-12, C). Continue to ventilate the patient’s lungs and tape the tube in place. If breath sounds are not heard, the tube has accidentally entered the patient’s trachea. Now, ventilate through the shorter, clear tube and listen for bilateral breath sounds. If they are heard, continue to ventilate and tape the tube in place (see Figure 12-12, D).
MODULE F
1. Recommend the insertion of an artificial airway or a change in the type of artificial airway (Code: IIIG1f) [Difficulty: ELE: R, Ap; WRE: An]
2. Manipulate standard and fenestrated tracheostomy tubes by order or protocol (ELE code: IIA7c) [Difficulty: ELE: R. Ap, An]
a. Get the necessary equipment
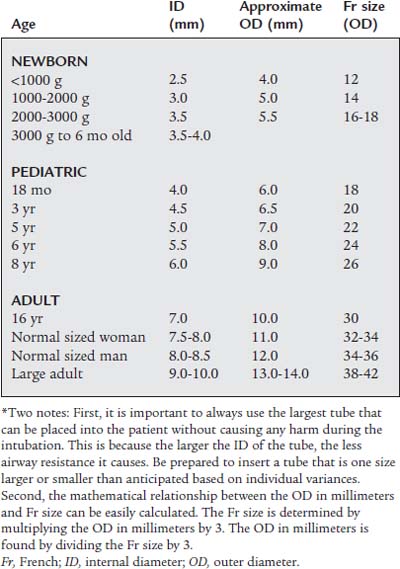
These tubes are available in a variety of sizes for patients of all ages from neonate to adult. See Table 12-1 for tracheostomy tube sizes (this also applies to tracheostomy buttons and endotracheal tubes) based on patient age. It is common practice to refer to the needed tube size by its inner diameter (ID). For example, a tracheostomy tube for an adult female would be 7.5- or 8.0-mm ID.
b. Put the equipment together and make sure that it works properly
The following are commonly seen examples of tracheostomy tube styles:
1. Standard tracheostomy tube
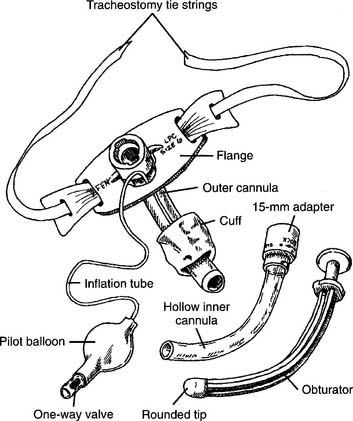
After the tracheostomy procedure is completed, the majority of patients have a standard tube placed into the stoma. Refer to Figure 12-13 for these features of a typical tracheostomy tube:
2. Fenestrated tracheostomy tube
Refer to Figure 12-14 when reviewing these features of the fenestrated tracheostomy tube:
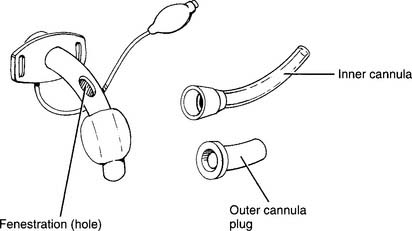
Figure 12-14 Fenestrated tracheostomy tube with its component parts and features.
(From Eubanks DH, Bone RC: Comprehensive respiratory care, ed 2, St Louis, 1990, Mosby.)
4. Maintain the proper position and appropriate cuff inflation of a tracheostomy tube (Code: IIIB4d) [Difficulty: ELE: R, Ap; WRE: An]
5. Change the tracheostomy tube (ELE code: IIIB7) [Difficulty: R, Ap, An]
b. Routine tube change
6. Independently perform tracheostomy care (Code: IIIF2g5) [Difficulty: ELE: R, Ap; WRE: An] (ELE code: IIIB6) [Difficulty: ELE: R, Ap, An]
7. Extubate the patient
a. Recommend extubation (Code: IIIG1h) [Difficulty: ELE: R, Ap; WRE: An]
Extubation should only be performed after correction of the causes that led to insertion of the tracheostomy tube. If the patient has required mechanical ventilation, review the discussion in Chapter 15 that relates to weaning the patient and extubation.
b. Perform extubation (Code: IIIB9) [Difficulty: ELE: R, Ap; WRE: An]
Extubation should be performed only by trained personnel and under the proper conditions to ensure the patient’s safety. See Box 12-3 for a list of complications that can occur after extubation. The generally recommended steps in extubation include the following:
Alternatively, in rapid succession:
Routine stoma care to ensure healing usually includes the following each shift: