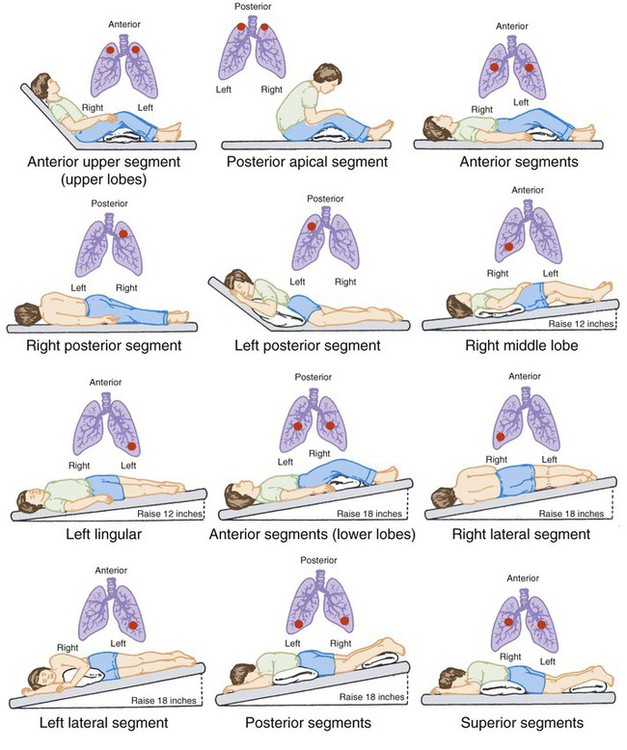
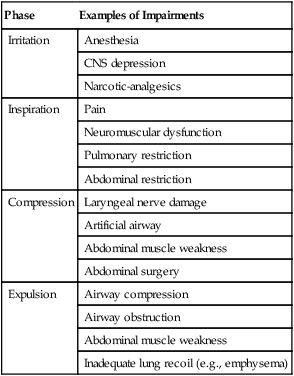
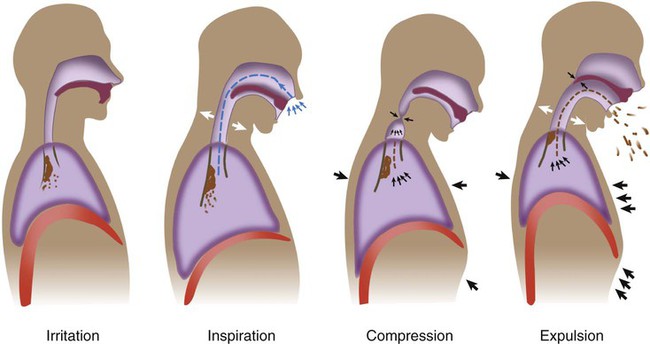
After reading this chapter you will be able to: Airway clearance therapy involves the use of noninvasive techniques designed to help mobilize and remove secretions and improve gas exchange.1–6 Previously, airway clearance methods often were grouped under a broad category of techniques called chest physical therapy (CPT). CPT involves not only airway clearance techniques but also various exercise protocols and breathing retraining methods.1,2 This chapter focuses on noninvasive airway clearance. The primary invasive method of airway clearance, suctioning, is discussed in Chapter 33. Traditionally, airway clearance therapy has involved CPT (postural drainage, percussion, and vibration [PDPV]) combined with cough instruction.6 Over the years, several additional noninvasive airway clearance methods have been developed to augment or replace this traditional approach. These newer techniques include modified breathing and coughing routines, manual hyperinflation, and mechanical devices designed to augment secretion clearance.2 In the past, airway clearance methods were commonly used in medical practice without firm scientific knowledge regarding their effectiveness. One example was to order CPT for essentially all postoperative patients in the hope that its use would prevent the respiratory complications of surgery.7–12 It is now known that this broad application of airway clearance therapy is both ineffective and costly. In an effort to address these types of issues, the American College of Chest Physicians (ACCP) conducted a formal systematic review of the evidence-based practice for nonpharmacologic airway clearance therapies.3 The recommendations of the ACCP are included in this chapter. As a result of evidence-based initiatives, it has been shown that combining certain airway clearance techniques with exercise can improve lung function in patients with cystic fibrosis (CF).3,5,6 Another review of related research raised questions regarding the effectiveness of CPT in patients with acute and stable chronic obstructive pulmonary disease (COPD), chronic bronchitis, or bronchiectasis.13,14 Successful outcomes in airway clearance techniques require knowledge of normal and abnormal physiology, careful patient evaluation and selection, a clear definition of therapeutic goals, rigorous application of the appropriate evidence-based methods, and ongoing assessment and follow-up.15–18 Normal airway clearance requires a patent airway, a functional mucociliary escalator, and an effective cough.5,19,20 Airways normally are kept open by structural support mechanisms (see Chapter 8) and kept clear by proper function of the ciliated mucosa. The mucociliary clearance mechanism operates from the larynx down to the respiratory bronchioles. The mucus itself originates from the goblet cells and submucosal glands, although Clara cells and tissue fluid transudation also contribute to airway secretions. Ciliated epithelial cells normally move this mucus via a coordinated wave of ciliary motion toward the trachea and larynx, where excess secretions can be swallowed or expectorated. Although essentially a reserve clearance mechanism, cough is one of the most important protective reflexes.21–23 By ridding the larger airways of excessive mucus and foreign matter, cough assists the normal mucociliary clearance and helps ensure airway patency. As shown in Figure 40-1, there are four distinct phases to a normal cough: irritation, inspiration, compression, and expulsion. In the initial irritation phase, an abnormal stimulus provokes sensory fibers in the airways to send impulses to the medullary cough center in the brain. This stimulus normally is inflammatory, mechanical, chemical, or thermal. Infection is a good example of cough stimulation caused by an inflammatory process. Foreign bodies can provoke a cough through mechanical stimulation. Chemical stimulation can occur when irritating gases are inhaled (e.g., cigarette smoke). Finally, cold air may cause thermal stimulation of sensory nerves and produce a cough. Any abnormality that alters airway patency, mucociliary function, strength of the inspiratory or expiratory muscles, thickness of secretions, or effectiveness of the cough reflex can impair airway clearance and cause retention of secretions.19,20,22,23 In addition, some therapeutic interventions, especially interventions used in critical care, can result in abnormal clearance. In the presence of pathogenic organisms, retention of secretions can lead to infection. Infectious processes provoke an inflammatory response and the release of chemical mediators. These chemical mediators, including leukotrienes, proteases, and elastases, can damage the airway epithelium and increase mucus production, resulting in a vicious cycle of worsening airway clearance.20 Compounding these problems may be failure of the cough reflex. In patients with retained secretions, interference with any one of the four phases of cough can result in ineffective airway clearance. Table 40-1 provides examples of factors that can impair the normal cough reflex. TABLE 40-1 Mechanisms Impairing Cough Reflex As indicated in Box 40-1, additional factors can impair airway clearance in critically ill patients with artificial airways, the most important of which is the airway itself.16 The presence of the tube in the trachea increases mucus secretion, whereas the cuff of the tube mechanically blocks the mucociliary escalator. In addition, movement of the tube tip and cuff can cause erosion of the tracheal mucosa and impair mucociliary clearance further. Lastly, endotracheal tubes impair the compression phase of the cough reflex by preventing closure of the glottis (see Table 40-1). Although suctioning is used to aid secretion clearance, it too can cause damage to the airway mucosa and impair mucociliary transport. Inadequate humidification can cause thickening or inspissation of secretions, mucous plugging, and airway obstruction. High fractional inspired oxygen (FiO2) concentrations can impair mucociliary clearance, either directly or by causing acute tracheobronchitis. Several common drugs, including some general anesthetics and narcotic-analgesics, can depress mucociliary transport. Lastly, several diseases commonly seen in critically ill patients are associated with poor secretion clearance; these are discussed in the following sections.3,12 Several diseases are associated with abnormal clearance, including diseases affecting airway patency, composition and production of mucus, ciliary structure and function, and normal cough reflex.3,20,24 Internal obstruction or external compression of the airway lumen can impair airway clearance. Examples include foreign bodies, tumors, and congenital or acquired thoracic anomalies such as kyphoscoliosis. Internal obstruction also can occur with mucus hypersecretion, inflammatory changes, or bronchospasm, further narrowing the lumen. Examples include asthma, chronic bronchitis, and acute infections. Diseases that alter normal mucociliary clearance can also cause retention of secretions. CF is a common disorder in this category. In CF, the solute concentration of the mucus is altered because of abnormal sodium and chloride transport.25 This alteration increases the viscosity of mucus and impairs its movement up the respiratory tract. Although less common, there are several conditions in which the respiratory tract cilia do not function properly.26 These ciliary dyskinetic syndromes also can contribute to ineffective airway clearance. Chronic airway inflammation and infection can lead to bronchiectasis, a common finding in CF and ciliary dyskinetic syndromes. In bronchiectasis, the airway is permanently damaged, dilated, and prone to constant obstruction by retained secretions.14 Other conditions that can lead to bronchiectasis include chronic obstructive lung diseases, foreign body aspiration, and obliterative bronchiolitis.27 As previously discussed, any condition that affects the four components of an effective cough also alters airway clearance. Mucociliary function may be normal, but without an effective cough, mucous plugs, obstruction, and atelectasis can occur. The most common conditions affecting the cough reflex are musculoskeletal and neurologic disorders, including muscular dystrophy, amyotrophic lateral sclerosis, spinal muscular atrophy, myasthenia gravis, poliomyelitis, and cerebral palsy (see Chapter 29). The primary goal of airway clearance therapy is to help mobilize and remove retained secretions, with the ultimate aim to improve gas exchange, promote alveolar expansion, and reduce the work of breathing. Box 40-2 lists general indications for airway clearance therapy.3,5,12 More specific indications are described as each airway clearance technique is discussed. Patients with acute conditions in whom airway clearance therapy may be indicated include (1) acutely ill patients with copious secretions; (2) patients in acute respiratory failure with clinical signs of retained secretions (audible abnormal breath sounds, deteriorating arterial blood gases, chest radiographic changes); (3) patients with acute lobar atelectasis; and (4) patients with Airway clearance therapy has proved effective in aiding secretion clearance and improving pulmonary function in chronic conditions associated with copious sputum production, including CF, bronchiectasis, and chronic bronchitis in certain patients.3,10,15–17 Generally, sputum production must exceed 25 to 30 ml/day for airway clearance therapy to improve secretion removal significantly. Airway clearance therapy has been used as a preventive mode of respiratory care in various disorders. Current evidence is inclusive regarding the benefits of this approach. The best-documented preventive uses of airway clearance therapy include (1) body positioning and patient mobilization to prevent retained secretions in acutely ill patients and (2) CPT combined with physical activity to maintain lung function in patients with CF.3,4,6,8,28 Other preventive applications of airway clearance therapy have not proved to be useful.3,5 Box 40-3 lists the key factors that must be considered when assessing a patient’s need for airway clearance therapy.3,15–17 Physical findings such as a loose, ineffective cough, labored breathing pattern, decreased or bronchial breath sounds, coarse inspiratory and expiratory crackles, tachypnea, tachycardia, or fever may indicate a potential problem with retained secretions. A chest radiograph often shows atelectasis and areas of increased density in such cases. CPT (percussion, postural drainage, and vibration) has long been considered a standard of care in patients with CF and in some other patients with specific pulmonary conditions. Evidence suggests that these therapies benefit mucus transport and assist in the expectoration of secretions.3,11,21 Postural drainage involves the use of gravity and mechanical energy to help mobilize secretions. The various body positions assumed are intended to drain secretions from each of the patient’s lung segments into the central airways, where they can be removed by cough or suctioning.1,2,15,29–31 This drainage is accomplished by simply placing the segmental bronchus to be drained in a more vertical position, permitting gravity to assist in the process. Positions generally are held for 3 to 15 minutes (longer in special situations) and modified as the patient’s condition and tolerance warrant.15 Cough methods are used with postural drainage therapy and are discussed separately. To guide practitioners in applying postural drainage techniques, the American Association for Respiratory Care (AARC) has developed and published a clinical practice guideline on postural drainage. Excerpts from the AARC guideline, including indications, contraindications, hazards and complications, assessment of need, assessment of outcome, and monitoring, appear in Clinical Practice Guideline 40-1.15 Postural drainage is most effective in conditions characterized by excessive sputum production (>25 to 30 ml/day). For maximum effect, head-down positions should exceed 25 degrees below horizontal.1,2,30–33 Positions can be modified if a patient’s condition presents a contraindication to treatment.2 Postural drainage is not likely to succeed unless and until adequate systemic and airway hydration is ensured.34,35 In patients in critical care, including patients on mechanical ventilation, postural drainage should be performed every 4 to 6 hours as indicated. In spontaneously breathing patients, frequency should be determined by assessing patient response to therapy. To avoid gastroesophageal reflux and the possibility of aspiration, treatment times should be scheduled before or at least Before positioning, the procedure (including adjunctive techniques) should be explained to the patient. As necessary, clothing around the waist and neck should be loosened. Also, the clinician should inspect any monitoring leads, intravenous tubing, and oxygen (O2) therapy equipment connected to the patient and, if necessary, make adjustments to ensure continued function during the procedure. Because postural drainage positioning predisposes patients to arterial desaturation, pulse oximetry should be considered if hypoxemia is suspected.15 Before starting the procedure, the clinician should measure the patient’s vital signs and auscultate the chest. These simple assessments serve as baseline measurements for monitoring the patient’s response during the procedure and can assist in determining outcomes. Figure 40-2 depicts the primary positions used to drain the various lung lobes and segments. Generally, to obtain the proper head-down position, the clinician must lower the head of the bed by at least 16 to 18 inches to achieve the desired 25-degree angle. In the ambulatory care setting, a tilt table can be used in lieu of a hospital bed. A tilt table allows precise positioning at head-down angles up to 45 degrees. When angles this large are used, shoulder supports must be provided to prevent the patient from sliding off the tilt table.
Airway Clearance Therapy
 Describe how normal airway clearance mechanisms work and the factors that can impair their function.
Describe how normal airway clearance mechanisms work and the factors that can impair their function.
 Identify pulmonary diseases associated with abnormal clearance of secretions.
Identify pulmonary diseases associated with abnormal clearance of secretions.
 State the goals and clinical indications for airway clearance therapy.
State the goals and clinical indications for airway clearance therapy.
 Describe the proper technique and potential benefit of each of the following:
Describe the proper technique and potential benefit of each of the following:
 Directed coughing and related expulsion techniques
Directed coughing and related expulsion techniques
 Positive expiratory pressure therapy
Positive expiratory pressure therapy
 High-frequency compression/oscillation methods
High-frequency compression/oscillation methods
 Evaluate a patient’s response to airway clearance therapy.
Evaluate a patient’s response to airway clearance therapy.
 Modify airway clearance therapies on the basis of patient response.
Modify airway clearance therapies on the basis of patient response.
Physiology of Airway Clearance
Normal Clearance
Abnormal Clearance
Phase
Examples of Impairments
Irritation
Anesthesia
CNS depression
Narcotic-analgesics
Inspiration
Pain
Neuromuscular dysfunction
Pulmonary restriction
Abdominal restriction
Compression
Laryngeal nerve damage
Artificial airway
Abdominal muscle weakness
Abdominal surgery
Expulsion
Airway compression
Airway obstruction
Abdominal muscle weakness
Inadequate lung recoil (e.g., emphysema)
Diseases Associated With Abnormal Clearance
General Goals and Indications
Airway Clearance Therapy for Acute Conditions
 abnormalities owing to lung infiltrates or consolidation.15–17 In treating acute respiratory conditions, inhaled bronchodilator therapy before airway clearance therapy may improve the overall effectiveness of the treatment both by opening the airways and by increasing the mucociliary activity. For acute pulmonary infections, inhaled antibiotics after airway clearance therapy can lead to improved deposition of the antibiotic.2 Acute conditions for which airway clearance therapy is probably not indicated include (1) acute exacerbations of COPD, (2) pneumonia without clinically significant sputum production, and (3) uncomplicated asthma.3,5
abnormalities owing to lung infiltrates or consolidation.15–17 In treating acute respiratory conditions, inhaled bronchodilator therapy before airway clearance therapy may improve the overall effectiveness of the treatment both by opening the airways and by increasing the mucociliary activity. For acute pulmonary infections, inhaled antibiotics after airway clearance therapy can lead to improved deposition of the antibiotic.2 Acute conditions for which airway clearance therapy is probably not indicated include (1) acute exacerbations of COPD, (2) pneumonia without clinically significant sputum production, and (3) uncomplicated asthma.3,5
Airway Clearance Therapy for Chronic Conditions
Airway Clearance Therapy to Prevent Retention of Secretions
Determining the Need for Airway Clearance Therapy
Airway Clearance Methods
Chest Physical Therapy
Technique
 to 2 hours after meals or tube feedings.36,37 If the patient assessment indicates that pain may hinder treatment implementation, the clinician also should consider coordinating the treatment regimen with prescribed pain medication.
to 2 hours after meals or tube feedings.36,37 If the patient assessment indicates that pain may hinder treatment implementation, the clinician also should consider coordinating the treatment regimen with prescribed pain medication.



 ) imbalances.
) imbalances. abnormalities caused by unilateral lung disease
abnormalities caused by unilateral lung disease