AIOD/PVOD—Critical Limb Ischemia
AMY B. REED
Presentation
A 61-year-old male is referred for evaluation of right lower extremity pain. He has a long-standing history of one-block claudication; however, 2 weeks ago, his right foot developed a bluish discoloration after showering. Since then, he has noted increasing redness upon standing, decreased sensation, and pain in the foot at night. He reports a 60-pack-year smoking history, hypertension, hyperlipidemia, and a history of myocardial infarction treated with percutaneous coronary angioplasty. On physical examination, his blood pressure is 132/80 mm Hg in both arms. The femoral pulses are weakly palpable. The right foot is cool with sluggish capillary refill and a monophasic Doppler signal in the dorsalis pedis (DP). There are no open sores or ulcerations on either lower extremity. Laboratory studies including complete blood cell count, creatinine level, and prothrombin time are normal.
Differential Diagnosis
The differential diagnoses for unilateral lower extremity pain without ulceration include diabetic neuropathy, nerve root compression, reflex sympathetic dystrophy, venous disease, and arterial insufficiency. In this patient with a history of extensive atherosclerosis and lower extremity claudication, which has now progressed to rest pain, critical limb ischemia from atherosclerotic occlusive disease must be considered the primary diagnosis.
Discussion
Critical limb ischemia results from insufficient arterial perfusion to supply the basal metabolic demands of the toes, foot, or ankle. After taking a careful history and performing a thorough physical examination, measurement of the ankle-brachial index (ABI) is a fundamental diagnostic tool for evaluation of lower extremity arterial insufficiency. Many patients, including diabetic patients, will often have heavily calcified arteries, rendering them noncompressible and thus falsely elevating the ABI. Pulse volume recordings (PVRs) and toe pressures are often unaffected by calcification and should be obtained in these patients. Arterial duplex of the aortoiliac vessels and the bilateral lower extremities will be informative in localizing the disease. ABIs less than 0.40, ankle pressures below 50 mm Hg, and toe pressures under 30 mm Hg with monophasic pulse volume recordings are all indicative of critical limb ischemia.
Recommendation
Noninvasive vascular laboratory studies, including ABI and PVRs, and aortography with bilateral lower extremity arteriography are ordered.
Vascular Laboratory Reports
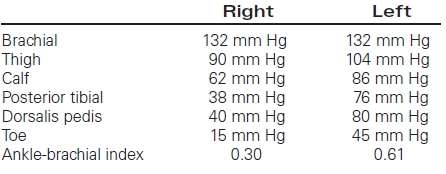
Pulse volume recordings: Monophasic waveforms are noted at all levels on the right. Waveforms are biphasic at the thigh and calf level on the right and monophasic at all infrageniculate levels on the left.
Arteriography
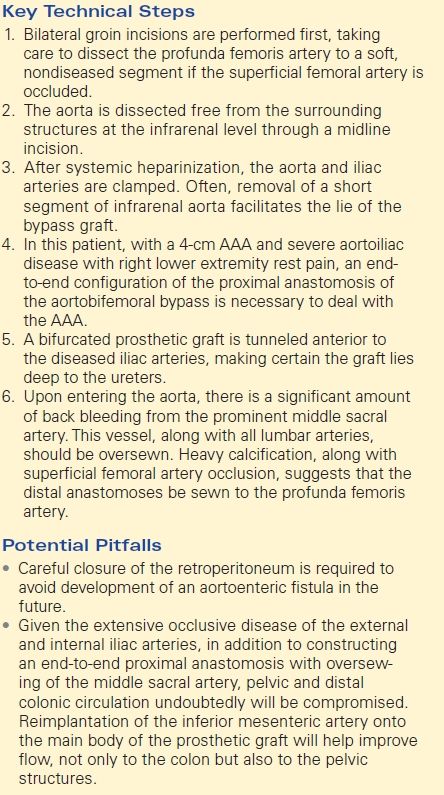
Aortogram with bilateral lower extremity runoff reveals the following images (Figs. 1 to 4).
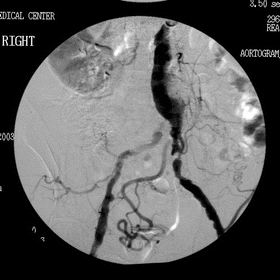
FIGURE 1 Aortoiliac imaging revealing high grade right common iliac lesion.
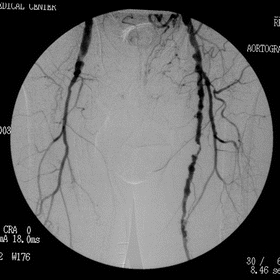
FIGURE 2 Occluded right superficial femoral artery.
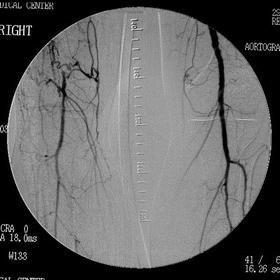
FIGURE 3 Digital subtraction angiogram demonstrating reconstitution of below knee popliteal segment.
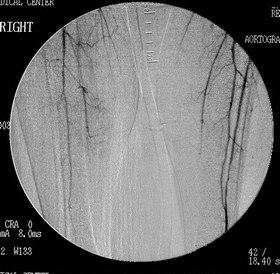
FIGURE 4 Right tibial level arterial occlusive disease.
Arteriography Report
There is dilation of the infrarenal aorta, suggestive of aneurysmal disease in addition to severe aortoiliac occlusive disease bilaterally. The hypogastric arteries are heavily diseased with the appearance of a prominent middle sacral artery supplying the pelvis. The superficial femoral artery is occluded on the right with single-vessel runoff. The left superficial femoral is diseased, but patent with two-vessel runoff.
Recommendation
Ultrasonography is indicated for follow-up on the arteriographic findings, suggestive of an infrarenal abdominal aortic aneurysm (AAA). A computed tomographic (CT) study could also be used; however, this typically requires an additional dye load (150 mL of intravenous contrast on average) on top of the 100 mL utilized for the arteriography and is best avoided.
Ultrasound Report
Ultrasound reveals a heavily calcified 4.0-cm AAA without iliac involvement.
Diagnosis and Recommendation
The patient has a 4-cm AAA with severe bilateral iliac arterial occlusive disease and right superficial femoral artery occlusion with single-vessel runoff to the right foot. This patient is offered an aortobifemoral bypass with possible right femoral to popliteal artery bypass. The presence of aneurysmal disease precludes the use of percutaneous iliac angioplasty and stenting in this patient. It is explained to the patient that the right lower extremity bypass may need to be performed at a later date if the operation is lengthy or significant bleeding is encountered, but that improving the inflow will be the first step in resolution of his rest pain.
Complications mentioned include bleeding, myocardial infarction, stroke, death, and graft failure requiring further surgery and possible amputation. The patient is instructed to continue all of his preoperative medications up to the day of surgery, particularly beta-blockade and aspirin. Smoking cessation and its importance postoperatively in helping to maintain graft patency is discussed with the patient.
Surgical Approach
Bilateral groin incisions are performed first, taking care to dissect the profunda femoris artery to a soft, nondiseased segment if the superficial femoral artery is occluded. The aorta is dissected free from the surrounding structures at the infrarenal level through a midline incision. After systemic heparinization, the aorta and iliac arteries are clamped. Often, removal of a short segment of infrarenal aorta facilitates the lie of the bypass graft. In this patient, with a 4-cm AAA and severe aortoiliac disease with right lower extremity rest pain, an end-to-end configuration of the proximal anastomosis of the aortobifemoral bypass is necessary to deal with the AAA. A bifurcated prosthetic graft is tunneled anterior to the diseased iliac arteries, making certain the graft lies deep to the ureters. Careful closure of the retroperitoneum is required to avoid development of an aortoenteric fistula in the future.
Case Continued
Upon entering the aorta, there is a significant amount of back bleeding from the prominent middle sacral artery previously noted on arteriography. This vessel, along with several lumbar arteries, is oversewn. Heavy calcification, along with superficial femoral artery occlusion on the right, requires that the distal anastomoses be sewn to the profunda femoris artery. Inspection of the sigmoid colon at this time reveals a pale, grayish color to the serosa with no signals on Doppler insonation.
Approach
Given the extensive occlusive disease of the external and internal iliac arteries, in addition to constructing an end-to-end proximal anastomosis with oversewing of the middle sacral artery, pelvic and distal colonic circulation undoubtedly will be compromised. Reimplantation of the inferior mesenteric artery onto the main body of the prosthetic graft will help improve flow, not only to the colon but also to the pelvic structures. At this time, the patient is cold and has been under anesthesia for nearly 6 hours (Table 1).
TABLE 1. AIOD/PVOD—Combined Rest Pain