Although smoking is a risk factor for coronary atherosclerosis, the age-related impact on lesion morphology has not been studied. The aim of this study was to assess the age-related impact of smoking on the extent of atherosclerosis and arterial remodeling. In Providing Regional Observations to Study Predictors of Events in the Coronary Tree, 687 patients with acute coronary syndrome underwent 3-vessel gray scale and virtual histology intravascular ultrasound imaging of 3,185 nonculprit lesions. In 207 patients ≤65 years, current (smoking within 1 month) and former (no smoking for >1 month) smokers showed significantly smaller normalized volumes of external elastic membrane (EEM), lumen, and P + M (plaque + media) compared with nonsmokers. At the minimal lumen area site, current and former smokers had significantly smaller EEM, lumen, and P + M areas than nonsmokers. Conversely, in 480 patients >65 years, current smokers had greater normalized P + M volumes than nonsmokers with no difference in normalized EEM or lumen volumes. Finally, in patients >65 years (but not in patients ≤65 years), current smokers showed more plaque ruptures (4.7% vs 1.8%, p = 0.05) and echolucent plaques (8.3% vs 3.9%, p = 0.05) compared with nonsmokers. On multivariable analysis, a history of smoking (combining current and former smoking) predicted smaller normalized EEM volumes compared with nonsmokers ≤65 years. In conclusion, in patients ≤65 years, but not in patients >65 years, smoking had a vascular constrictive effect that contributed to severe luminal stenosis. Conversely, smokers >65 years had more plaque with greater plaque instability.
Smoking is a risk factor for coronary atherosclerosis and is associated with a high rate of cardiovascular events, including earlier development of myocardial infarction. However, previous angiographic and intravascular ultrasound (IVUS) studies have not consistently shown any effects of smoking on coronary disease progression. Although smoking is an important modifiable predictor of adverse clinical outcomes, morphologic lesion characteristics in different age groups and mechanisms of action on nonculprit lesions remain unclear. Because smoking alters endothelial function, vasomotor tone, platelet and hemostatic function, and atheroma burden, its influence may vary in subjects of different ages and stages of atherosclerosis. Previous studies have suggested that patients >65 versus ≤65 years showed different patterns of nonculprit lesion morphology, atherosclerotic progression, and clinical outcomes after revascularization. To assess the age-related impact of smoking on extent of atherosclerosis and arterial remodeling, we used gray scale and virtual histology (VH)-IVUS to evaluate nonculprit coronary lesions in 2 age groups (>65 vs ≤65 years) of patients with acute coronary syndromes who were enrolled in the Providing Regional Observations to Study Predictors of Events in the Coronary Tree (PROSPECT) study.
Methods
The PROSPECT study design, major inclusion and exclusion criteria, end points, and definitions have been previously described in detail. In brief, 697 patients with acute coronary syndromes underwent angiography and multimodality intracoronary imaging of the proximal 6 to 8 cm of all 3 major epicardial coronary arteries after performance of successful and uncomplicated percutaneous coronary intervention of all coronary lesions responsible for index events (culprit lesions) and other severe angiographic stenoses. Of the 697 patients enrolled in PROSPECT, IVUS and history of smoking data were available in 687 patients with 3,185 nonculprit lesions, thus comprising the study population. Both gray scale and VH-IVUS were obtained using a synthetic aperture array, 20-MHz, 3.2 Fr catheter (Eagle Eye, In-Vision Gold; Volcano Corporation, Rancho Cordova, California) with motorized catheter pullback (0.5 mm/s). Based on previous data, age of 65 years was used to separate the 687 patients into 2 age groups. There were 480 patients ≤65 years and 207 patients >65 years who were then divided into nonsmokers, former smokers (no smoking for >1 month), and current smokers (smoking within 1 month). The study was approved by the institutional review board or medical ethics committee at each participating center, and all patients gave written informed consent.
The quantitative and qualitative analyses performed in PROSPECT have also been described in detail previously. Baseline angiograms and gray scale and VH-IVUS studies were analyzed at separate core laboratories at the Cardiovascular Research Foundation (New York, New York) that were blinded to clinical outcomes. Quantitative coronary angiography was performed using CMS software, version 7.0 (Medis, Leiden, The Netherlands). Minimal lumen diameter, interpolated reference vessel diameter, and diameter stenosis were measured for all culprit lesions.
Gray scale and VH-IVUS analyses were performed using QCU-CMS software (Medis), pcVH 2.1 software (Volcano Corporation) and proprietary qVH software (Cardiovascular Research Foundation). The external elastic membrane (EEM) and luminal borders were contoured for each frame. Quantitative gray scale IVUS measurements included the cross-sectional areas of the EEM, lumen, and plaque and media (P + M = EEM minus lumen) and plaque burden (P + M divided by EEM area). The remodeling index was calculated as the EEM area at the minimal lumen area (MLA) site divided by the average of the proximal and distal reference EEM areas. Plaque rupture was defined as an intraplaque cavity that communicated with the lumen with an overlying residual fibrous cap fragment. Echolucent plaque was defined as a plaque containing a non-echoreflective dark zone. An IVUS nonculprit lesion was defined by a plaque burden of at least 40% in at least 3 consecutive frames. Lesions were considered separate if there was a ≥5-mm-long segment with <40% plaque burden between them.
On the basis of VH-IVUS, plaque components were categorized as dense calcium (white), fibrous tissue (green), fibrofatty (yellow), or necrotic core (red) and reported as percentages of total plaque areas and volumes. A fibroatheroma was defined as >10% confluent necrotic core. If there was >30° of necrotic core abutting to the lumen in 3 consecutive slices, the fibroatheroma was classified as thin-cap fibroatheroma; otherwise, it was classified as thick-cap fibroatheroma. Each IVUS lesion was coregistered to the angiographic roadmap using fiduciary branches for alignment as previously described.
All statistical analyses were performed using SAS, version 9.2 (SAS Institute, Inc., Cary, North Carolina). Categorical variables were summarized using percentages and counts and were compared using the chi-square tests or Fischer’s exact test where appropriate. Continuous variables were compared using analysis of variance (ANOVA) and unpaired t tests or nonparametric Wilcoxon rank-sum test and shown as median and interquartile ranges. For lesion-level data, a model with a generalized estimating equation approach was used to compensate for potential cluster effects of multiple nonculprit lesions in the same patient and presented as least square means with 95% confidence intervals. Using generalized estimating equation, multivariable linear regression analysis was also performed to the independent determinants to predict normalized EEM volume. A p value <0.05 was considered statistically significant.
Results
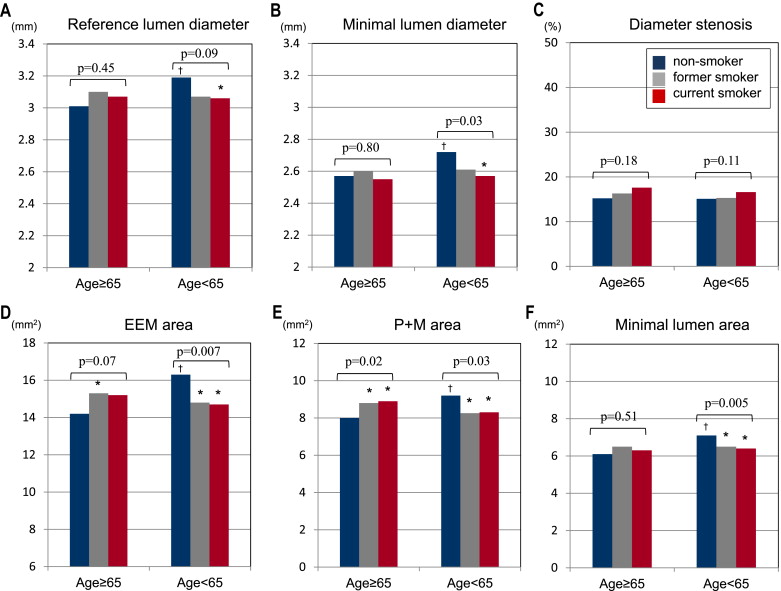
Patient characteristics are summarized in Table 1 . Compared with patients >65 years, there were more men than women in the group of patients ≤65 years (82% vs 63%, p <0.001); and the prevalence of diabetes mellitus was higher in patients >65 years than in patients ≤65 years (23% vs 15%, p = 0.005). Angiographic diameter stenosis of the worst nonculprit lesion per patient was 45.9% (37.5, 57.8%) in patients ≤65 years and 46.8% (38.2, 59.6%) in patients >65 years (p = 0.39). Figure 1 compares quantitative angiographic and IVUS data among current smokers, former smokers, and nonsmokers in patients ≤65 and >65 years.
| Variable | Total (N = 687) | Nonsmoker (n = 192) | Former smoker (n = 167) | Current smoker (n = 328) |
|---|---|---|---|---|
| Age (years) | 58.1 [50.5, 66.6] | 64.2 [55.2, 72.3] | 63.3 [54.6, 69.9] | 53.5 [47.1, 60.6] ∗ , † |
| Men | 521 (76%) | 127 (66%) | 137 (82%) ∗ | 257 (78%) ∗ |
| Diabetes | 117 (17%) | 47 (25%) | 24 (14%) ∗ | 46 (14%) ∗ |
| Metabolic syndrome | 322 (48.6%) | 93 (49%) | 81 (50%) | 148 (47%) |
| Hypertension | 313 (46%) | 112 (59%) | 86 (52%) | 115 (36%) ∗ , † |
| Estimated creatinine clearance (mL/min) ‡ | 97.8 [76.4, 123.3] | 88.6 [67.0, 113.2] | 93.1 [73.3, 117.5] | 106.0 [85.3, 135.7] ∗ , † |
| Previous myocardial infarction | 73 (11%) | 18 (10%) | 20 (12%) | 35 (11%) |
| Clinical presentation | ||||
| ST-segment elevation myocardial infarction | 209 (30%) | 46 (24%) | 52 (31%) | 111 (34%) ∗ |
| Non-ST elevation myocardial infarction | 449 (65%) | 138 (72%) | 104 (62%) | 206 (63%) ∗ |
| Unstable angina | 29 (4.2%) | 8 (4.2%) | 11 (6%) | 10 (3%) |
| Height (cm) | 173.0 [166.4, 178.0] | 170.0 [163.0, 176.0] | 174.0 [168.0, 180.0] ∗ | 174.0 [168.0, 180.0] ∗ |
| Weight (kg) | 82.8 [73.0, 95.0] | 82.0 [72.8, 95.3] | 83.5 [74.8, 96.5] | 82.6 [73.0, 94.8] |
| Waist circumference (cm) | 100.0 [92.0, 109.0] | 101.0 [92.0, 111.8] | 100.0 [94.0, 109.0] | 99.1 [91.4, 107.0] |
| Body mass index (kg/m 2 ) | 27.9 [25.1, 31.2] | 28.3 [25.6, 32.5] | 27.8 [25.8, 30.4] | 27.6 [24.5, 30.9] ∗ |
| Total cholesterol (mg/dL) | 170.5 [149.0, 198.0] | 162.0 [142.0, 194.0] | 167.0 [148.0, 192.3] | 174.0 [153.8, 203.0] |
| Low-density lipoprotein cholesterol (mg/dL) | 100.8 [79.2, 128.2] | 98.4 [78.4, 127.2] | 97.6 [74.8, 122.6] | 103.4 [85.2, 130.0] |
| High-density lipoprotein cholesterol (mg/dL) | 38.6 [33.0, 46.0] | 39.0 [35.0, 51.0] | 38.6 [35.0, 46.0] | 38.6 [32.0, 43.0] ∗ , † |
| Triglycerides (mg/dL) | 125.0 [88.6, 177.1] | 118.0 [88.6, 162.0] | 119.5 [88.6, 177.1] | 136.0 [97.0, 179.0] ∗ |
| Statin at admission | 314 (46%) | 83 (43%) | 70 (42%) | 161 (49%) |
| High-sensitivity C-reactive protein at admission (mg/L) | 7.25 [2.45, 19.00] | 7.40 [2.15, 19.70] | 6.05 [2.15, 16.40] | 8.45 [3.00, 19.55] |
† p <0.05 versus former smokers.
In 480 patients ≤65 years, there were 2,226 nonculprit lesions: 38.8% in the left anterior descending artery, 31.1% in the left circumflex artery, 29.5% in the right coronary artery, and 0.4% in the left main coronary artery. Comparing nonsmokers, former smokers, and current smokers, there was no significant difference in nonculprit IVUS lesion length (16.0 mm [14.4, 17.7] vs 15.8 mm [14.2, 17.5] vs 15.2 mm [14.3, 15.9], p = 0.56) or distance from the MLA to the ostium (33.6 mm [30.8, 36.4] vs 32.6 mm [29.8, 35.5] vs 33.4 mm [31.9, 34.8], p = 0.88).
Current and former smokers showed significantly smaller normalized volumes of EEM, lumen, and P + M compared with nonsmokers ( Table 2 ). At the MLA site, current and former smokers also had significantly smaller EEM, lumen, and P + M areas than nonsmokers. However, there was no difference in %plaque volume or %plaque burden at the MLA site among the groups. There were similar trends at proximal and distal reference segments.
| Variable | Nonsmoker (n = 438) | Former smoker (n = 443) | Current smoker (n = 1345) | p value (ANOVA) | ∗ p Value | † p Value | ‡ p Value |
|---|---|---|---|---|---|---|---|
| Volumetric data | |||||||
| Normalized EEM (mm 3 /mm) | 17.7 [16.8, 18.5] | 15.9 [15.2, 16.6] | 16.0 [15.5, 16.4] | 0.003 | 0.002 | <0.001 | 0.77 |
| Normalized lumen (mm 3 /mm) | 9.2 [8.7, 9.6] | 8.2 [7.8, 8.6] | 8.3 [8.0, 8.5] | 0.003 | 0.002 | <0.001 | 0.87 |
| Normalized plaque and media (mm 3 /mm) | 8.5 [8.0, 8.9] | 7.6 [7.3, 8.0] | 7.7 [7.5, 7.9] | 0.008 | 0.003 | 0.003 | 0.68 |
| %Plaque volume | 48.0 [47.3, 48.8] | 48.2 [47.4, 48.9] | 48.2 [47.8, 48.6] | 0.96 | 0.79 | 0.79 | 0.95 |
| At the minimal lumen area site | |||||||
| EEM area (mm 2 ) | 16.3 [15.4, 17.2] | 14.8 [14.1, 15.4] | 14.7 [14.3, 15.1] | 0.007 | 0.006 | 0.001 | 0.83 |
| Minimal lumen area (mm 2 ) | 7.1 [6.7, 7.5] | 6.5 [6.1, 6.9] | 6.4 [6.2, 6.6] | 0.005 | 0.02 | <0.001 | 0.65 |
| Plaque and media area (mm 2 ) | 9.2 [8.6, 9.9] | 8.3 [7.9, 8.7] | 8.3 [8.0, 8.5] | 0.03 | 0.02 | 0.009 | 0.95 |
| Plaque burden (%) | 55.8 [54.6, 57.1] | 56.1 [55.0, 57.3] | 56.1 [55.5, 56.7] | 0.92 | 0.71 | 0.72 | 0.93 |
| Remodeling index | 0.93 [0.91, 0.95] | 0.93 [0.91, 0.94] | 0.92 [0.91, 0.92] | 0.21 | 0.75 | 0.19 | 0.15 |
| Area stenosis (mm 2 ) | 25.2 [23.4, 27.0] | 25.7 [23.9, 27.5] | 27.4 [26.4, 28.4] | 0.07 | 0.73 | 0.04 | 0.10 |
| Echolucent plaque | 15 (3.4%) | 14 (3.2%) | 54 (4.0%) | 0.66 | 0.79 | 0.65 | 0.44 |
| Plaque rupture | 15 (3.4%) | 9 (2.0%) | 51 (3.8%) | 0.20 | 0.23 | 0.77 | 0.10 |
∗ p value, nonsmokers versus former smokers.
† p value, nonsmokers versus current smokers.
In 207 patients >65 years, there were 959 nonculprit lesions: 42.4% in the left anterior descending artery, 30.2% in the left circumflex artery, 26.7% in the right coronary artery, and 0.7% in the left main coronary artery. Comparing nonsmokers, former smokers, and current smokers, there was no significant difference in nonculprit angiographic lesion length (16.2 mm [14.7, 17.7] vs 17.0 mm [15.4, 18.7] vs 17.8 mm [15.6, 20.0], p = 0.46) or the distance from the MLA to the ostium (33.4 mm [31.0, 35.7] vs 31.3 mm [28.3, 34.3] vs 32.5 mm [29.3, 35.6], p = 0.57).
Current and former smokers had greater normalized P + M volumes compared with nonsmokers ( Table 3 ). However, because of a difference in EEM volumes (larger in current and former smokers than in nonsmokers), normalized lumen volumes remained similar among the groups. At the MLA site, P + M area was larger in current and former smokers than in nonsmokers, but there was no difference in lumen areas among the groups. Similar trends were seen at proximal and distal reference segments.
| Variable | Nonsmoker (n = 434) | Former smoker (n = 333) | Current smoker (n = 192) | p Value (ANOVA) | ∗ p Value | † p Value | ‡ p Value |
|---|---|---|---|---|---|---|---|
| Volumetric data | |||||||
| Normalized EEM (mm 3 /mm) | 15.5 [14.8, 16.2] | 16.9 [15.9, 17.8] | 16.6 [15.6, 17.5] | 0.04 | 0.02 | 0.07 | 0.64 |
| Normalized lumen (mm 3 /mm) | 7.9 [7.6, 8.3] | 8.6 [8.1, 9.1] | 8.4 [7.8, 8.9] | 0.12 | 0.051 | 0.18 | 0.65 |
| Normalized plaque and media (mm 3 /mm) | 7.6 [7.2, 7.9] | 8.3 [7.8, 8.8] | 8.2 [7.7, 8.7] | 0.02 | 0.01 | 0.04 | 0.69 |
| %Plaque Volume | 48.6 [47.8, 49.4] | 49.3 [48.4, 50.1] | 49.5 [48.3, 50.7] | 0.39 | 0.28 | 0.23 | 0.77 |
| At the minimal lumen area site | |||||||
| EEM area (mm 2 ) | 14.2 [13.6, 14.8] | 15.3 [14.5, 16.1] | 15.2 [14.2, 16.2] | 0.07 | 0.04 | 0.09 | 0.90 |
| Minimal lumen area (mm 2 ) | 6.1 [5.8, 6.5] | 6.5 [6.0, 6.9] | 6.3 [5.8, 6.9] | 0.51 | 0.25 | 0.54 | 0.73 |
| Plaque and media area (mm 2 ) | 8.0 [7.6, 8.4] | 8.8 [8.3, 9.3] | 8.9 [8.3, 9.5] | 0.02 | 0.02 | 0.02 | 0.92 |
| Plaque burden (%) | 56.4 [55.3, 57.6] | 57.4 [56.2, 58.6] | 58.2 [56.7, 60.0] | 0.18 | 0.26 | 0.07 | 0.40 |
| Remodeling index | 0.92 [0.90, 0.93] | 0.91 [0.89, 0.92] | 0.91 [0.89, 0.93] | 0.77 | 0.47 | 0.70 | 0.78 |
| Area stenosis (mm 2 ) | 27.2 [25.3, 29.1] | 27.9 [26.1, 29.7] | 28.7 [26.2, 31.2] | 0.63 | 0.59 | 0.34 | 0.60 |
| Echolucent plaque | 17 (3.9%) | 14 (4.2%) | 16 (8.3%) | 0.05 | 0.85 | 0.05 | 0.09 |
| Plaque rupture | 8 (1.8%) | 11 (3.3%) | 9 (4.7%) | 0.13 | 0.20 | 0.05 | 0.44 |
∗ p value, nonsmokers versus former smokers.
† p value, nonsmokers versus current smokers.
As listed in Tables 3 and 4 , patients >65 years who were current smokers had more nonculprit plaque ruptures (4.7% vs 1.8%, p = 0.05), echolucent plaques (8.3% vs 3.9%, p = 0.05), and noncalcified thick-cap fibroatheromas (20.3% vs 13.0%, p = 0.03) compared with nonsmokers. Conversely, in patients ≤65 years, there were no significant intergroup differences in plaque composition and lesion morphology.
| Variable | Age >65 | Age ≤65 | ||||
|---|---|---|---|---|---|---|
| Never Smoked (n = 409) | Former Smoker (n = 287) | Current Smoker (n = 177) | Never Smoked (n = 376) | Former Smoker (n = 395) | Current Smoker (n = 1194) | |
| Virtual histology plaque type | ||||||
| Fibroatheroma | 241 (58.9%) | 192 (66.9%) | 116 (65.5%) | 222 (59.0%) | 246 (62.3%) | 690 (57.8%) |
| TCFA | 80 (19.6%) | 54 (18.8%) | 43 (24.3%) | 84 (22.3%) | 101 (25.6%) | 268 (22.4%) |
| Calcified ThCFA | 108 (26.4%) | 82 (28.6%) | 37 (20.9%) | 70 (18.6%) | 85 (21.5%) | 205 (17.2%) |
| Non-calcified ThCFA | 53 (13.0%) | 56 (19.5%) ∗ | 36 (20.3%) ∗ | 68 (18.1%) | 60 (15.2%) | 217 (18.2%) |
| Normalized volume | ||||||
| Necrotic core (mm 3 /mm) | 0.53 [0.46, 0.60] | 0.71 [0.60, 0.83] ∗ | 0.60 [0.50, 0.71] | 0.58 [0.50, 0.66] | 0.54 [0.47, 0.61] | 0.52 [0.48, 0.56] |
| Dense calcium (mm 3 /mm) | 0.29 [0.24, 0.34] | 0.45 [0.36, 0.53] ∗ | 0.31 [0.21, 0.42] | 0.28 [0.22, 0.34] | 0.24 [0.21, 0.28] | 0.23 [0.20, 0.25] |
| Fibrous (mm 3 /mm) | 2.38 [2.21, 2.56] | 2.74 [2.50, 2.98] ∗ | 2.75 [2.50, 2.99] ∗ | 2.99 [2.68, 3.29] | 2.51 [2.31, 2.70] ∗ | 2.58 [2.46, 2.70] ∗ |
| Fibrofatty (mm 3 /mm) | 0.93 [0.81, 1.06] | 0.96 [0.83, 1.09] | 1.05 [0.90, 1.20] | 1.11 [0.97, 1.24] | 0.90 [0.79, 1.01] ∗ | 0.98 [0.91, 1.05] |
| Media (mm 3 /mm) | 3.40 [3.32, 3.47] | 3.57 [3.47, 3.67] ∗ | 3.54 [3.42, 3.66] ∗ | 3.62 [3.52, 3.72] | 3.46 [3.39, 3.53] ∗ | 3.42 [3.37, 3.48] ∗ |
| %Area at the minimal lumen area site | ||||||
| Necrotic core (%) | 14.4 [12.8, 16.1] | 14.9 [12.9, 16.8] | 13.1 [11.1, 15.1] | 13.4 [11.7, 15.0] | 14.1 [12.5, 15.7] | 13.4 [12.5, 14.4] |
| Dense calcium (%) | 7.5 [6.3, 8.6] | 9.0 [7.3, 10.6] | 5.9 [4.4, 7.5] † | 6.2 [5.1, 7.4] | 6.4 [5.4, 7.5] | 5.6 [4.9, 6.2] |
| Fibrous (%) | 58.3 [56.9, 59.7] | 57.2 [55.1, 59.4] | 60.1 [58.0, 62.1] | 59.2 [57.6, 60.8] | 59.7 [58.2, 61.2] | 60.6 [59.7, 61.4] |
| Fibrofatty (%) | 19.8 [17.5, 22.1] | 18.9 [16.7, 21.1] | 21.2 [18.2, 24.1] | 21.2 [18.8, 23.6] | 19.8 [17.4, 22.1] | 20.3 [19.2, 21.5] |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


