Acute Stroke after CEA
MATTHEW R. ABATE and MOHAMMED M. MOURSI
Presentation
A 65-year-old Caucasian man is 45 minutes following a right carotid endarterectomy (CEA) and is now in the recovery room. The patient underwent a CEA for a symptomatic right internal carotid stenosis measuring 86% on preoperative cerebral angiography, with the contralateral side measured as a 35% stenosis. The patient was receiving aspirin preoperatively. The operation was performed under regional anesthesia without the use of a shunt, and the carotid artery was closed with the use of a bovine pericardial patch. Initial intraoperative duplex ultrasound scan at the completion of the endarterectomy showed an intimal flap at the distal extent of the endarterectomy site requiring reopening of the artery and placement of several tacking stitches. Completion duplex ultrasound scan after this repair showed no apparent defects. The patient had no hemodynamic instability during the perioperative period and has demonstrated a normal neurologic exam until this point. Now, 45 minutes after arrival in the recovery room, the patient develops a left-sided hemiparesis involving his upper and lower extremities. In addition, he is now unable to respond to verbal commands.
Differential Diagnosis
The diagnosis with this clinical scenario is clear. This patient has signs and symptoms consistent with an acute stroke after CEA. The diagnostic dilemma involves the etiology for this stroke. The differential for the cause of an ipsilateral acute stroke after CEA includes (1) intracerebral hemorrhage, (2) watershed infarction, (3) hypoperfusion intraoperatively or postoperatively, (4) hyperperfusion, (5) embolization of atheromatous plaque or thrombus occurring intraoperatively, (6) embolization occurring postoperatively with or without a technical defect at the endarterectomy site (embolic material could be atheromatous plaque, thrombus, or platelet aggregation), (7) thrombosis of the endarterectomy site with or without a technical defect, (8) heparin-induced thrombocytopenia, (9) kink in the artery resulting in low flow, and (10) embolization from a site other than the carotid bifurcation.
Diagnostic Tests
Given that he had a lucent period in the immediate postoperative period and had a completion duplex ultrasound scan that showed no defect, this patient would be best served by simultaneously preparing the operating room for reexploration and obtaining a duplex scan of the carotid artery to determine patency.
Duplex Ultrasound Scan
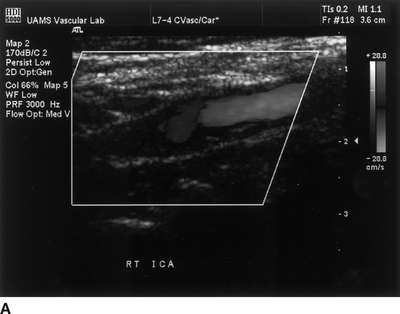
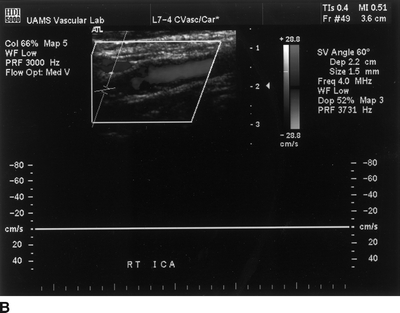
FIGURE 1 A:Duplex ultrasound with thrombosed right internal carotid artery. B:Doppler waveform demonstrating no detectable flow within the right internal carotid artery.
Duplex Ultrasound Scan Report
Duplex ultrasound scan shows an acutely thrombosed internal carotid artery (ICA) (Fig. 1A) with Doppler waveform signal indicating no flow (Fig. 1B).
Diagnosis and Recommendation
The patient has an acute stroke secondary to a thrombosed ICA endarterectomy site, most likely due to fibrin and platelet adhesion to the endarterectomized surface. Given the thrombosed artery and the short period of time (less than 2 hours) since the CEA, the patient needs emergent reexploration of the carotid artery. Although the addition of a duplex scan in this situation is somewhat controversial, one of the cornerstones of diagnosis and treatment for an acute stroke after CEA is to determine patency of the artery. With a normal intraoperative duplex scan and a lucent period postoperatively, a duplex scan is recommended. In most hospital settings, this will not delay the required reexploration, given the portability of the duplex machine and the time required to prepare an operating room. In this situation, the ICA was thrombosed, and reexploration is indicated. However, had the duplex showed a patent artery with no defects, exploration could prove to be harmful. In that circumstance, rather than an operation, the patient would require a computed tomographic (CT) scan of the head and possible cerebral arteriography (see Discussion).
Case Continued
By the time the duplex is completed, the operating room is ready, and the patient is taken for reexploration.
Discussion
Once the carotid artery is found to be thrombosed, the patient is given systemic heparin at 100 U/kg IV bolus. In the operating room, the patient can be reexplored under the original regional anesthetic block if the time interval between cervical block and reexploration is short and if the patient is cooperative. Otherwise, a general anesthetic is administered. The neck incision is opened, and the carotid artery is exposed, and the thrombosed artery is confirmed by visual inspection and/or handheld Doppler. In addition, any kinks or other abnormalities are identified and inspected. The common carotid and external carotid arteries are controlled with vascular clamps, and the arteriotomy is opened; note that no attempt is made to clamp the distal ICA at this time. Upon opening the artery, the thrombus is removed, and the internal carotid is allowed to back bleed into the field; if no back bleeding is observed and there appears to be thrombus extending distally, an embolectomy catheter can be used to gently remove distal clot. Care must be taken to avoid creating a cavernous sinus fistula. Once the thrombus is removed, the endarterectomized surface is inspected for defects. If any defects are identified, they are repaired by either removal of residual plaque or tacking of any intimal flaps. Alternatively, upon opening the artery, platelet aggregation may be identified. Rather than frank thrombus, a defect site may be noted. This should be removed and the defect repaired.
Surgical Approach
The patient undergoes general endotracheal anesthesia, and at exploration, the carotid artery is found to be thrombosed. The clot is removed from the distal internal carotid as well as at the endarterectomy site. No obvious defect can be identified. Therefore, an interposition saphenous vein graft is used to replace the proximal ICA. Low molecular weight dextran is started as a continuous drip. Intraoperative duplex ultrasound scan shows a widely patent interposition graft with no defects.
Case Continued
The patient awakes from anesthesia with a mild left upper extremity weakness as his only neurologic defect. The patient is placed on an additional antiplatelet agent along with aspirin. Physical and occupational therapy are initiated, and the patient is eventually sent home to continue his rehabilitation.
Case Conclusion
In this particular case, since no technical defect was observed, the presumed etiology of the thrombosis is fibrin and platelet aggregation and adhesion to the endarterectomized surface. If this is not replaced, the chance of rethrombosis is high. Therefore, a portion of greater saphenous vein was harvested from the thigh and used as an interposition graft. It is important to initiate pharmacologic antiplatelet therapy both intraoperatively with dextran as well as postoperatively, with another oral antiplatelet agent in addition to aspirin. The neck is then closed; the patient is awakened from the general anesthetic and is continued on dextran for 24 hours and antiplatelet agents. Care is taken to avoid hypotension in the postoperative period (Table 1).



