Chapter 52
Acute Deep Venous Thrombosis
Surgical and Interventional Treatment
Anthony J. Comerota, Faisal Aziz
Acute deep venous thrombosis (DVT) represents a disease spectrum ranging from asymptomatic calf vein thrombosis to the painful, blue, swollen limb of phlegmasia cerulea dolens resulting from extensive multisegment thrombosis involving the iliofemoral venous segment. Until 2008, national and international guidelines for the treatment of patients with acute DVT recommended anticoagulation only. However, the 8th American College of Chest Physicians (ACCP) Consensus Conference on Antithrombotic and Thrombolytic Therapy1 and the American Heart Association (AHA) Scientific Statement on the management of iliofemoral DVT2 suggest interventional strategies for thrombus removal that include surgical and catheter-based techniques to reduce the incidence of postthrombotic syndrome (PTS), especially in patients with extensive venous thrombosis.
Postthrombotic Syndrome
The most important consideration leading to guideline recommendations for thrombus removal in patients with extensive DVT is the severe morbidity associated with the PTS and the evidence that early elimination of thrombus prevents or reduces postthrombotic morbidity.
Morbidity
PTS is defined as the signs and symptoms resulting from acute DVT. This usually is the consequence of venous hypertension resulting from valve reflux and/or luminal obstruction. Studies have shown that patients with PTS have a significant reduction in quality of life (QoL).3,4 The severity of the patient’s acute DVT is predictive of postthrombotic morbidity, especially when it involves the iliofemoral segment. Patients with iliofemoral DVT appear to be a clinically relevant subset of patients with acute venous thrombosis in that they have severe postthrombotic morbidity when treated with anticoagulation alone.5–8 In a prospective observational study of anticoagulation for acute DVT, iliofemoral DVT was found to be the most powerful predictor of severe PTS (hazard ratio 2.23).8 Labropoulos et al9 monitored venous pressures in patients with PTS after treatment for their acute DVT. They found that patients who were treated for iliofemoral DVT had the highest venous pressures. This confirmed previous observations that iliofemoral DVT patients treated by anticoagulation alone had ambulatory venous hypertension, with 40% demonstrating venous claudication and up to 15% developing venous ulceration within 5 years.5–7 Essentially, all these patients will have reduction in their QoL. The morbidity of PTS escalates substantially with ipsilateral recurrence. A meta-analysis of outcomes after treatment for acute DVT demonstrated that recurrence occurs more commonly in patients with a large burden of thrombus.10
Etiology
The pathophysiology of postthrombotic venous disease is ambulatory venous hypertension, which is defined as elevated venous pressure during exercise.11,12 Ambulatory venous pressure is linearly linked to the pathophysiologic changes observed with chronic venous disease, such as swelling, pigmentation, and lipodermatosclerosis.13 Microcirculatory changes leading to dermal breakdown follow.
The anatomic components contributing to ambulatory venous hypertension are venous valvular incompetence and luminal obstruction. The most severe postthrombotic morbidity is associated with the highest venous pressures, which occur in patients with both valvular incompetence and luminal venous obstruction.11,14 Although valvular function can be reliably assessed with ultrasound by quantifying valve closure times, techniques are not yet available to assess the relative contribution of venous obstruction to the pathologic venous hemodynamics leading to clinical postthrombotic morbidity. Figure 52-1 succinctly illustrates the difficulty of identifying even extensive venous obstruction, either hemodynamically or radiologically. Neither ascending phlebography performed and interpreted by a skilled radiologist nor the maximal venous outflow test performed in an accredited vascular laboratory identified abnormalities attributed to venous obstruction. A cross section of the proximal femoral vein removed during a classic Linton procedure clearly showed recanalization channels through what was once occlusive thrombus, which resulted in chronic obstruction of a large proportion of the luminal surface area. Unfortunately, noninvasive physiologic techniques cannot detect venous hemodynamic impairment of even this advanced degree of obstruction when they are performed on resting patients. This example is not a unique observation, but is common to postthrombotic morbidity. It is evident that venous hemodynamics are adversely affected long before imaging techniques can detect obstruction. The inability to quantitate obstruction has led physicians to underappreciate its contribution to postthrombotic pathophysiology. Luminal venous obstruction causes the most severe forms of PTS. Therefore, treatment strategies for thrombus removal should be developed during the initial encounter with the patient, and if successful, can eliminate obstruction as part of the long-term pathophysiology and should significantly reduce the incidence of PTS.
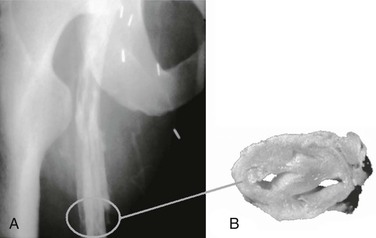
Figure 52-1 Postthrombotic venous disease illustrating the inability to identify obstruction as part of the pathophysiology of chronic venous disease. This patient had had iliofemoral deep venous thrombosis 10 years earlier and was treated with anticoagulation alone. Severe postthrombotic syndrome developed, and the patient underwent multiple hospitalizations for venous ulceration. (A) An ascending phlebogram showed recanalization of the iliofemoral venous system; however, the radiologist’s interpretation was that there was “no obstruction” of the deep venous system, and a 3-second maximal venous outflow test was “normal.” A classic Linton procedure was performed and showed (B) the cross section of the femoral vein at the corresponding location on the phlebogram, just below the profunda femoris vein.
Experimental observations in canine models of acute DVT have shown that successful thrombolysis preserves endothelial function and valve competence.15,16 These experimental observations appear to translate into improved clinical outcomes when put into the perspective of natural history studies of acute DVT treated with anticoagulation alone. Investigators have found that distal valve incompetence develops in patients with persistent venous obstruction treated with anticoagulation alone, even when the distal veins are not initially involved with thrombus.17 When spontaneous lysis occurred, defined as clot resolution within 90 days, valve function was frequently preserved.18 These investigators also confirmed that the combination of valvular incompetence and venous obstruction was associated with the most severe postthrombotic morbidity.14,19 It is intuitive that successful elimination of acute venous thrombus will eliminate luminal obstruction and increase the likelihood that normal valve function will be preserved. It follows, then, that in patients whose thrombus is mechanically or pharmacologically eliminated, postthrombotic morbidity should be avoided or at least significantly reduced.
Rationale for Thrombus Removal
There is a large body of evidence supporting the rationale for a strategy of thrombus removal, especially in patients with iliofemoral DVT. When a strategy of thrombus removal is successful, venous patency is restored, valve function is maintained, QoL is improved, and the risk of recurrence is reduced. Qvarfordt et al20 measured compartment pressures in patients with acute iliofemoral DVT before and after operative venous thrombectomy. Compartment pressures (a surrogate for venous pressures) were pathologically elevated upon presentation but normalized after operative thrombectomy. These important observations documented significant physiologic benefit by restoring the main venous outflow to the lower extremity and formed the basis for a randomized trial.
The Scandinavian investigators randomized patients with iliofemoral DVT to operative venous thrombectomy plus arteriovenous fistula (AVF) and anticoagulation or to anticoagulation alone. This multicenter randomized trial demonstrated that patients who underwent venous thrombectomy enjoyed improved iliac vein patency (P < .05), lower venous pressure (P < .05), less edema (P < .05), and fewer postthrombotic symptoms (P < .05) than did patients receiving anticoagulation alone.21–23 They also observed that patients who underwent venous thrombectomy were more likely to retain venous valve function in their femoropopliteal segment than were those treated by anticoagulation alone. This observation was consistent with that reported by Killewich et al,17 who demonstrated that persistent proximal obstruction leads to distal valve incompetence in veins not initially involved with thrombus, and that elimination of iliofemoral thrombosis maintains distal valve function.
A growing body of evidence suggests that catheter-directed thrombolysis (CDT) is of benefit, especially in patients with iliofemoral DVT.24–27 A case-controlled study demonstrated significantly improved QoL in patients treated by CDT versus anticoagulation alone for iliofemoral DVT.28 In a subsequent analysis, the QoL benefit associated with CDT was directly correlated with the volume of thrombus removed.24 The more residual thrombus at the end of CDT, the worse the QoL. This also correlated with objective measures of PTS; the greater the degree of lysis, the fewer symptoms of PTS observed.27
Baekgaard et al29 followed 103 patients for 6 years after they were treated with CDT for iliofemoral DVT. They reported that 86% of veins were patent without reflux, and only 6% of patients developed recurrence during follow-up.
Pharmacomechanical techniques have been shown to improve outcomes compared with CDT using the drip technique alone. Pharmacomechanical techniques have shortened treatment times, reduced doses of lytic agent, and reduced length of intensive care unit (ICU) and hospital stays.30–32
An underappreciated but important benefit of successful thrombus removal is the reduction in the rate of recurrent DVT. As mentioned earlier, patients with iliofemoral DVT have an exceptionally high recurrence rate compared with patients with less extensive thrombosis.10,33 Aziz and Comerota26 observed that patients with iliofemoral DVT treated with catheter-directed techniques appeared to have a low recurrence rate. Upon further analysis, the benefit was accrued in those patients who had successful thrombus removal, whereas those with the bulk of the thrombus remaining (unsuccessful lysis) had a significantly higher recurrence rate.
Vogel et al34 addressed the issue of whether pharmacomechanical techniques compromised valve function, presumably due to valve injury. In a sequential analysis of CDT versus pharmacomechanical thrombolysis, there did not appear to be any adverse effect on valve function using pharmacomechanical techniques. The important observations were that valves functioned best in patients who had successful results. An interesting observation was that 35% of the veins in the noninvolved limbs had incompetent valves.
There is no argument that large randomized trial data are the best evidence. The results of recent randomized trials of CDT versus anticoagulation for acute DVT, combined with the substantial body of observational, clinical, and case-control evidence, support a strategy of thrombus removal, especially in patients with extensive venous thrombosis.
Randomized Trials of Catheter-Directed Thrombolysis
Elsharawy and Elzayat35 reported a small randomized trial comparing anticoagulation versus CDT. Based upon point estimates used to calculate sample size, they appeared to have achieved their goal. They demonstrated that patients treated with CDT had significantly improved venous patency and a reduction in valvular incompetence compared with those treated with anticoagulation alone. These observations are often overlooked in the absence of measures of QoL and objective analysis of postthrombotic morbidity using such measurements as the Villalta scale or the Venous Clinical Severity Score.
The recently published CaVenT trial reported the long-term outcome after additional CDT versus anticoagulation alone for acute iliofemoral DVT.25 These investigators randomized 209 patients. Their primary endpoint was iliofemoral patency at 6 months and PTS at 2 years. CDT was performed with the UniFuse catheter (AngioDynamics, Latham, NY). Alteplase was infused at a dose of 0.01 mg/kg/hr for a maximum of 96 hours. The alteplase was prepared by mixing 20 mg in 500 mL of 0.9% sodium chloride. This resulted in a 70-kg man being infused with 0.7 mg of recombinant tissue plasminogen activator (rt-PA) in 17.5 mL of infusate. This appears to be an unusually small volume of infusate, which might potentially be a disadvantage in patients.
The mean duration of thrombolysis was 24 days; 43% of patients had complete thrombolysis, 37% had partial, and thrombolysis was unsuccessful in 10%. Patients receiving CDT had a mean clot resolution of 82%. Patients treated with additional CDT had significantly improved iliofemoral venous patency at 6 months (P = .012) and less PTS at 2 years (P = .047). The authors reported that lower thrombus scores at completion of CDT were associated with increased patency (P < .04), and that patency of the iliofemoral venous system correlated with a reduction in PTS (P < .001). There was an absolute risk reduction in PTS of 14.4% in patients who received CDT. Major bleeding complications occurred in 3.3% of patients who underwent CDT. Only one inferior vena cava filter was used in this group, and no symptomatic pulmonary embolism (PE) was observed.
These results demonstrated a significant benefit in those patients receiving additional CDT. The actual benefit would likely have been substantially greater if patients entered into this trial truly had iliofemoral DVT. In reality, only 45% of the patients randomized to thrombolysis and 36% of those in the anticoagulation group had iliofemoral DVT. Therefore, although approximately 60% of patients randomized in this trial had less than iliofemoral DVT, significant benefit was observed. The authors reported that the number needed to treat to prevent one PTS was seven, but we believe that the reduction of postthrombotic morbidity would have been substantially greater (and the number needed to treat would be smaller) if all patients in CaVenT had truly had iliofemoral DVT.
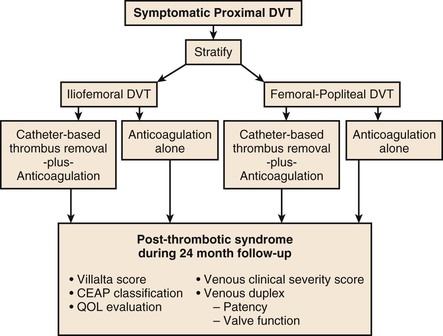
A much larger study, the ATTRACT trial, sponsored by the National Institutes of Health, is prospectively randomizing patients with symptomatic proximal DVT.36 The target sample size is 692 patients. Patients with iliofemoral and femoropopliteal DVT will be stratified at entry into the study to catheter-based techniques of thrombolysis versus anticoagulation alone. The primary endpoint is PTS at 24 months. The ATTRACT trial will also evaluate relative benefits of pharmacomechanical techniques versus the CDT drip technique and will include a careful cost analysis. The basic design of ATTRACT is illustrated in Figure 52-2.
Strategies for Thrombus Removal
Randomized trials demonstrating positive outcomes for patients undergoing a strategy of thrombus removal have now been published21–23,25 and the largest is underway.36 CDT is the preferred treatment option for most patients who have no contraindication to thrombolytic therapy. Pharmacomechanical techniques are becoming increasingly popular and tend to shorten treatment time and reduce the lytic dose.
Contemporary venous thrombectomy is generally available to all patients. There are few contraindications to operative thrombectomy short of old thrombus that is adherent to the vein wall and cannot be removed. The goal of venous thrombectomy is to remove the iliofemoral and infrainguinal thrombus and restore unobstructed venous return to the vena cava. Knowing the full extent of thrombosis preoperatively and having good imaging intraoperatively are crucial for a well-planned and successful procedure.
Thrombolytic Therapy
Initial attempts at pharmacologic resolution of acute DVT used systemic thrombolysis. Early studies involving systemic delivery of plasminogen activators resulted in high rates of bleeding complications and less than optimal lytic results. Many patients were treated for infrainguinal DVT; therefore, even when lytic therapy was successful, the benefits were not as apparent as in patients with iliofemoral venous thrombosis. A summary of studies comparing anticoagulation with systemic thrombolysis was reported.37 Results were disappointing considering the increased bleeding risk. However, an important observation demonstrated the improved long-term outcome in patients with phlebographically successful systemic thrombolysis. Catheter-based procedures have rapidly replaced systemic thrombolysis as the preferred method of treating patients with extensive DVT.
Intrathrombus Catheter-Directed Thrombolysis
During the process of thrombosis, Glu-plasminogen binds to fibrin, which is converted to Lys-plasminogen. This modification produces more binding sites for plasminogen activators, and therefore, more efficient production of plasmin. The basic mechanism of thrombolysis is the activation of fibrin-bound plasminogen and the resultant production of plasmin. It is intuitive that delivery of the plasminogen activator within the thrombus is more effective and potentially safer than systemic infusion of plasminogen activators. Additionally, intrathrombus delivery protects plasminogen activators from circulating plasminogen activator inhibitor, and more importantly, protects the active enzyme plasmin from neutralization by circulating antiplasmin. This neutralization of circulating plasminogen is so effective that the half-life of plasmin in the systemic circulation is only a fraction of a second.
Numerous reports have demonstrated good outcomes of CDT for acute DVT, and most have been tabulated.37 In general, when patients with acute DVT are treated, success rates in the range of 75% to 90% can be anticipated. The rate of bleeding complications generally ranges from 5% to 11%. Fortunately, serious distant bleeding is uncommon, and intracranial bleeding is a rarity. Most bleeding complications are localized to the venous access site. Symptomatic PE during infusion is uncommon, and fatal PE is a rarity.
An interesting report by Chang et al38 documented the benefit of sequential intrathrombus bolus dosing of rt-PA without a continous infusion in a small group of patients (12 lower extremities with acute DVT). This study’s careful observations lend credence to high-pressure bolus dosing (pulse-spray) of plasminogen activator into the acute thrombus. These observations underscore the importance of saturating the thrombus with a plasminogen activator and the effective activation of Lys-plasminogen.
Outcomes from the National Venous Registry.
The National Venous Registry is the largest report to date of patients treated with lytic therapy for acute DVT, with 71% having iliofemoral DVT.39 Although significant advances in treatment have been made since the publication of this report, a number of the early observations remain important for clinicians to recognize.
There was a significant correlation (P < .001) of thrombus-free survival with the results of initial therapy. At 1 year, 78% of the patients with initially complete clot resolution had patent veins versus only 37% of patients who had less than 50% lysis. In the group of patients with first-time iliofemoral DVT who initially had successful thrombolysis, 96% of the veins remained patent at 1 year. Initial lytic success also correlated with valve function at 6 months. Sixty-two percent of patients with less than 50% thrombolysis had venous valvular incompetence, whereas 72% with complete lysis had normal valve function (P < .02).
A cohort-controlled QoL study was performed to determine whether lytic therapy altered QoL in patients with iliofemoral DVT in the National Venous Registry.28 Results demonstrated that CDT was associated with better QoL than anticoagulation alone. QoL was directly related to initial success of thrombolysis. Patients who had a successful lytic outcome reported a better Health Utilities Index, improved physical functioning, less stigma of CVD, less health distress, and fewer overall postthrombotic symptoms. Not surprisingly, patients in whom CDT failed had outcomes similar to those treated with anticoagulation alone.
Available data to date present a compelling argument for CDT. Institutions participating in randomized trials should make every effort to enroll patients who are eligible. Those not participating in trials should adopt a strategy of thrombus removal that is based upon evidence to date.
Pharmacomechanical Thrombolysis
Although good results can be achieved with CDT, treatment times are often unacceptably long, and therefore, bleeding risk and cost associated with therapy are unacceptably high. This was succinctly characterized by Sillesen et al40 when they reported that 93% of their patients were successfully treated and discharged with patent veins and that more than 90% of the patients discharged with patent veins had normal venous valve function at 1 year. The treated patients had a mean duration of symptoms of just 7 days, and patients with symptoms exceeding 14 days were excluded. Therefore, lysis would be expected quickly in these patients because they truly had acute DVT. However, treatment time for CDT averaged 71 hours. This duration of acute care is logistically difficult, if not impossible, for many practitioners and many medical centers. The associated cost is high because all patients receiving lytic therapy are generally monitored in ICUs.
Endovascular Mechanical Thrombectomy.
Mechanical techniques alone or in combination with thrombolysis have been developed to more rapidly clear the venous system. Vedantham et al41 evaluated the effectiveness of mechanical thrombectomy alone or in combination with pharmacologic thrombolysis in 28 limbs of patients with acute DVT. They evaluated multiple devices, including the Amplatz (ev3, Inc., Plymouth, Minn), AngioJet (Possis Medical, Minneapolis, Minn), Trerotola (Arrow International, Reading, Penn), and Oasis (Boston Scientific/Medi-tech, Natick, Mass) catheters. Venographic scoring was performed at each step of the procedure. Twenty-six percent of the thrombus was removed by mechanical thrombectomy alone, whereas adding a plasminogen activator solution to the mechanical technique (pharmacomechanical) removed 82% of the thrombus. This tabulation includes patients with chronic occlusion who did not respond. Mechanical thrombectomy alone was successful in removing intraprocedural thrombus, which is generally gelatinous and not cross-linked with fibrin. The average infusion time was approximately 17 hours per limb, and 14% of patients had major bleeding complications.
Lin et al32 reported their 8-year experience with pharmacomechanical thrombolysis via a rheolytic thrombectomy catheter. Of their 98 patients, 46 received CDT alone and 52 underwent pharmacomechanical thrombolysis. Pharmacomechanical thrombolysis with the AngioJet catheter was associated with significantly fewer phlebograms, shorter ICU stays, shorter hospital stays, and fewer blood transfusions. Bleeding complications were not different between the two groups. A smaller patient group treated by rheolytic thrombectomy was reported by Kasirajan et al,42 who demonstrated that mechanical thrombectomy alone was less effective than combined pharmacomechanical thrombolysis.
Ultrasound-Accelerated Thrombolysis.
Parikh et al31 reported their initial clinical experience with ultrasound-accelerated thrombolysis in 53 patients treated for acute DVT with the EKOS EndoWave (Ekos Corp, Bothell, Wash) system. Unfortunately, both upper and lower extremity DVT patients were included in this report, and a variety of lytic agents were used. Complete lysis (≥90%) was observed in 70% of patients and overall lysis (complete and partial) in 91%. The median infusion time was 22 hours, and 4% of the patients had major complications, which were essentially puncture site hematomas. The authors’ impression was that compared with historical controls (a weakness of this report), treatment time and the dose of lytic agents were reduced with ultrasound-accelerated thrombolysis.
Isolated Segmental Pharmacomechanical Thrombolysis.
An interesting new technique is isolated segmental pharmacomechanical thrombolysis (ISPMT), which is achieved by using the Trellis catheter (Covidien, Mansfield, Mass). This double-balloon catheter is inserted into the thrombosed venous segment with the proximal balloon positioned at the upper edge (cephalic end) of the thrombus. When the balloons are inflated, plasminogen activator is infused into the thrombosed segment isolated by the balloons. The intervening catheter assumes a spiral configuration and spins at 1500 rpm for 15 to 20 minutes. The liquefied and fragmented thrombus is aspirated and treatment success evaluated by repeat segmental phlebography. If successful, the catheter is repositioned and additional thrombosed segments are treated; if residual thrombus persists, repeat treatment or other appropriate intervention (rheolytic thrombectomy, ultrasound-accelerated thrombolysis, balloon angioplasty, stenting) is performed. Martinez et al30 reviewed 52 consecutive limbs treated for iliofemoral DVT—the first 27 with CDT and the following 25 with ISPMT plus CDT when necessary. Thrombus burden and treatment outcomes were quantified. Ninety-three percent of the patients were treated with rt-PA, venoplasty and stenting were used to correct underlying stenoses in all patients, and all received long-term therapeutic anticoagulation. Sixteen of the 27 legs treated by CDT required other adjunctive mechanical techniques to clear the thrombus, such as the AngioJet, ultrasound-accelerated lysis, or pulse-spray techniques, whereas only 7 of the 25 limbs treated with ISPMT required additional adjunctive techniques. A larger percentage of the thrombus was removed with ISPMT than with CDT. Complete lysis (≥90%) was achieved in 11% of the limbs of CDT patients as opposed to 28% of the limbs treated by ISPMT (P = .077). Treatment time was shorter (23.4 hours vs 55.4 hours; P < .001), and the rt-PA dose was lower (33.4 mg vs 59.3 mg, P = .009) with ISPMT. Hospital and ICU length of stay was no different, which was the result of underlying patient comorbid conditions. If the ISPMT catheter was used alone, only 18% of the limbs underwent complete lysis. This was consistent with the observations of O’Sullivan et al.43 Bleeding complications occurred in 5% of patients who underwent CDT alone and in 5% of the patients treated by ISPMT.
Operative Venous Thrombectomy
Contemporary venous thrombectomy for iliofemoral venous thrombosis offers effective short- and long-term outcomes with relatively few complications. In a report of 230 patients, no fatal PEs and only 1 operative death occurred.44 The long-term benefits of venous thrombectomy relate to its ability to achieve proximal patency and maintain distal valve competence. Both are influenced by the initial technical success and avoidance of recurrent thrombosis. Therefore, attention to operative detail, removal of all thrombus, and correction of underlying lesions, as well as maintenance of therapeutic anticoagulation postoperatively, are crucial.
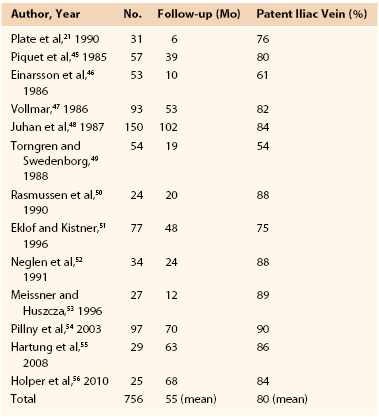
Pooled data from a number of contemporary reports on iliofemoral venous thrombectomy (Table 52-1)22,45–56 indicate that the early and long-term patency rate of the iliofemoral venous segment is 75% to 80% versus 30% in patients treated by anticoagulation alone.7 Femoropopliteal venous valve function is preserved in the majority of patients. The Scandinavian investigators reported their randomized trial of operative venous thrombectomy versus anticoagulation alone in patients with iliofemoral venous thrombosis.21–23 Patients underwent systematic follow-up with venous imaging and physiologic measurements. Six-month, 5-year, and 10-year follow-up showed that patients randomized to venous thrombectomy demonstrated improved patency (P < .05), lower venous pressure (P < .05), less leg edema (P < .05), and fewer postthrombotic symptoms (P < .05) than did patients treated with anticoagulation alone.
Technique of Contemporary Venous Thrombectomy
A brief summary of the important points of contemporary venous thrombectomy is provided in Box 52-1. The principles of venous thrombectomy are those of basic vascular surgical techniques: remove the thrombus; provide unobstructed outflow from the iliofemoral venous segment and unobstructed inflow from the infrainguinal venous segment; correct any underlying lesions; and prevent re-thrombosis. The sequential salient technical points follow.
Preoperative Care.
Preoperative anticoagulation is generally initiated with unfractionated heparin (UFH) because it has a short half-life and can be controlled more easily than low-molecular-weight heparin or direct factor Xa inhibitors. The full extent of thrombus (distal and proximal) is identified (see Box 52-1; Fig. 52-3).
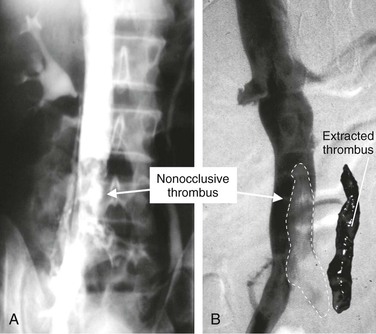
Figure 52-3 A and B, Contralateral iliocavagrams show nonocclusive thrombus in the vena cava and illustrate the importance of imaging to detect the proximal extent of thrombus. In B, the outlined area shows where the adjacent thrombus was extracted from the vena cava by balloon catheter thrombectomy. The proximal vena cava was protected with the balloon catheter (see Fig. 52-6).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree