Acute and Chronic Mediastinal Infections
Michael J. Liptay
Anthony W. Kim
Mediastinal infections are also known as mediastinitis. Acute mediastinitis is usually secondary to infections following operations requiring sternotomy or arising from perforation of the aerodigestive tract. Acute mediastinitis due to the spread of oropharyngeal infections, otherwise known as descending mediastinitis, represents a less common but extremely lethal form of this disease.
Chronic infections are uncommon; therefore only a minor amount of change in the presentation, diagnosis, and management of this disease has evolved. Most are the result of fungal disease originating in the various mediastinal node groups, while a few are secondary to mycobacterial organisms. Chronic fungal or tubercular infections may be self-limiting but may progress into the clinical entity of chronic fibrosing mediastinitis.
Postoperative Sternal Infection and Mediastinitis
The incidence of mediastinitis after cardiac surgical intervention in recent history generally has been between 1% and 4%. The causes and risk factors are many; they include diabetes, chronic obstructive pulmonary disease, congestive heart failure, use of internal mammary artery grafts (unilateral or bilateral), smoking, reoperation, lower ejection fraction, prolonged ventilation, obesity, high body mass index (BMI), immunosuppressive therapy, older age, use of bone wax, preoperative renal failure, duration of operation, prolonged cardiopulmonary bypass and aortic cross-clamp times, off-center sternotomy, improper stabilization of the sternum, poor hemostasis, use of pacing
wires, need for repeated blood transfusions in the early postoperative period, use of electrocautery, presence of infection elsewhere, extended intensive care unit stay and overall hospitalization, readmission to the hospital, and several others depending on the study reviewed (see references for more information).
wires, need for repeated blood transfusions in the early postoperative period, use of electrocautery, presence of infection elsewhere, extended intensive care unit stay and overall hospitalization, readmission to the hospital, and several others depending on the study reviewed (see references for more information).
The mechanism of infection has yet to be established, but different theories exist. One theory postulates that local osteomyelitis at the sternotomy site is allowed to propagate.29 Another theory supposes that sternal instability contributes to the superficial wound dehiscence and that this serves as a portal of ingress for infections.130 A third theory postulates that inadequate drainage in the retrosternal space serves as a culture medium for the source of mediastinal infection. A final theory suggests that concomitant infections, such as a nosocomial pneumonia, act to seed the sternotomy site.54
The bacterial pathogens found are usually Staphylococcus aureus and Staphylococcus epidermidis, which account for 50% to 80% of isolates. This supports the idea that skin flora at the time of operation are responsible for the infection. Perioperative contamination can also contribute pathogenic gram-positive infections. Also, the leg incision used to harvest a saphenous vein graft can be a source of pathogens and may be responsible for gastrointestinal flora found in some cases. Postoperative contamination is another potential source of infection. Gram-negative organisms such as Pseudomonas, Serratia, and Klebsiella are becoming more common pathogens. This may be reflective of the convergence of increased nosocomial infections and prolonged antibiotic use in the postoperative care of more complex and challenging cardiac patients. Mixed infections account for up to 40% of cases. Fungal mediastinitis is an infrequent cause of poststernotomy mediastinitis but should be considered in the setting of failed therapy or prolonged antibiotic use.
Diagnosis
The mortality rate associated with mediastinitis after coronary bypass surgery is 10% to 50%. Braxton and associates13 reported that the first-year survival rate after coronary artery bypass graft was 78% with mediastinitis and 95% without, with a threefold increase in mortality rate at 4 years’ follow-up. Others have corroborated a long-term negative effect of poststernotomy mediastinitis despite intervention.76,129 Some have suggested that early recognition and intervention of poststernotomy mediastinitis can lessen this negative effect.76
Clinical Manifestations
Clinically, postoperative mediastinitis should be suspected in the infected sternotomy wound. This can occur early or late in the clinical course. Classic signs may include erythema, purulent discharge, and sternal instability. A history of pain with breathing or difficulty lying in the lateral decubitus position is indicative of the two halves of the sternum moving against each other. It has been suggested that sternal instability as assessed by bimanual alternating sternal compression is the most helpful diagnostic maneuver.51 Sometimes the classic signs and symptoms may not be obvious. Fever, sepsis, or leukocytosis, especially without an obvious source may, be a presentation. Patients who are recovering slowly from a sternotomy may have their protracted course explained by an indolent poststernotomy mediastinitis.43
Radiographic studies are not routinely used, as clinical judgment usually suffices to detect poststernotomy mediastinitis, particularly in the acute early postoperative period. However, there are situations that warrant computed tomography (CT) scanning. These scans are useful either in the late presentation of poststernotomy mediastinitis or in the evaluation of unresolving sepsis due to an untreated source of mediastinitis. An undrained fluid collection or air–fluid level will be the classic finding on CT scan. CT scans are very helpful in poststernotomy mediastinitis that presents >30 days after surgery, as it can reveal bone and soft tissue involvement at the infereior aspect of the wound, which is not uncommon in this scenario.51 As for other imaging modalities, nuclear imaging studies, which are used in other forms of osteomyelitis, are at best controversial in poststernotomy mediastinitis.51
Treatment
Treatment of poststernotomy mediastinitis has evolved tremendously in recent years. Despite the large number of series evaluating the risk factors for poststernotomy mediastinitis, the majority of these reports do not include an analysis of its management. Only a handful of the recently published reports with large numbers in their series have included a description of the management philosophy.31,42 However, there has not been a complete, in-depth analysis of the management and its impact on outcomes. Conventional therapy—defined as opening and debriding the wound, serially packing the wound, and eventually closing the wound primarily—has been associated with an unacceptably high mortality rate, some authors having reported rates as high as 50%.120 High rates of treatment failure warranting additional surgical interventions are not uncommon.39 The mediocre results associated with conventional therapy have been the impetus behind the search for more aggressive management. A minor variation of debridement and primary closure has involved the use of retrosternal high-negative-pressure catheters, known as Redon catheters, to facilitate wound healing.132 Despite this addition, the use of the high negative pressure catheters is not commonly used.
The use of various flap closure techniques in the treatment of poststernotomy mediastinitis is frequently accepted as the standard therapy for these deep sternal wound infections. This management philosophy is largely based on series that have demonstrate early sternal debridement with flap closure, which is associated with mortality rates of <10% as well as low complication rates.72 Certain clinical situations, such as sternal instability without infection or in an infected mediastinum without internal mammary grafts, have demonstrated the benefits of muscle flap closure.112 Multivariate analysis has also demonstrated that the lack of flap closure in poststernotomy mediastinitis is associated with a significant increase in 1-year mortality.76 Despite these ostensibly convincing data, recent advances in the treatment of poststernotomy mediastinitis have challenged flap closure as the method of choice. In large part, this is due to the excellent results published with other management techniques, including those that include more recent innovations.
The addition of closed mediastinal irrigation with either saline or antibiotic solution to the debridement and primary closure is one alternative therapy that has yielded acceptable results.96,101 In 2004, Merrill and associates96 reported a 95% success rate in 40 patients with poststernotomy mediastinitis treated
with this single-stage revision. Dilute povidone-iodine or antibiotic irrigation was used until mediastinal fluid cultures dictated its cessation. Molina and colleagues101 have described simple debridement with rewiring of the sternum laterally for stabilization (Robicsek weave) and primary closure followed by postoperative closed mediastinal irrigation. Their closure technique, followed by a culture-driven antibiotic irrigation solution, resulted in a remarkable success rate of 98%. Equally impressive in both series was the fact that the mortality rates were 0%. Closed drainage irrigation using Redon catheters has been described as another variation of closed mediastinal drainage.79 Comparisons of Redon catheters to closed mediastinal irrigation have shown that the use of the latter technique is associated with improved failure and mortality rates.19 In contrast to these studies, others have shown that closed mediastinal irrigation following primary closure of sternal dehiscence in culture-proven mediastinitis is associated with an extremely high rate of failure. This has led some authors to caution against the use of this modality where an internal thoracic graft has been used and there is culture-proven infection.112
with this single-stage revision. Dilute povidone-iodine or antibiotic irrigation was used until mediastinal fluid cultures dictated its cessation. Molina and colleagues101 have described simple debridement with rewiring of the sternum laterally for stabilization (Robicsek weave) and primary closure followed by postoperative closed mediastinal irrigation. Their closure technique, followed by a culture-driven antibiotic irrigation solution, resulted in a remarkable success rate of 98%. Equally impressive in both series was the fact that the mortality rates were 0%. Closed drainage irrigation using Redon catheters has been described as another variation of closed mediastinal drainage.79 Comparisons of Redon catheters to closed mediastinal irrigation have shown that the use of the latter technique is associated with improved failure and mortality rates.19 In contrast to these studies, others have shown that closed mediastinal irrigation following primary closure of sternal dehiscence in culture-proven mediastinitis is associated with an extremely high rate of failure. This has led some authors to caution against the use of this modality where an internal thoracic graft has been used and there is culture-proven infection.112
Flap coverage is not limited to the pectoralis advancement flap. Omental flaps have been reported to be an adequate source of flap coverage and some have reported its benefits over muscle flaps. Milano and colleagues97 demonstrated that omental flaps were associated with shorter operations and decreased lengths of hospitalization as well as lower rates of early complications. Furthermore, recurrent infections are more common with muscle flaps.97,145 Brandt and Alvarez12 have used both pectoralis flaps and omental flaps to cover the wound and occupy any potential dead spaces, with impressive results, including fewer major complications, shorter hospitalizations, decreased mortality rates, and increased overall survival.12
Combination therapy with closed mediastinal irrigation using either primary closure alone or in combination with flap coverage has also been described with success. Rand and colleagues112 showed that muscle flap closure with closed mediastinal irrigation. Hirata and colleagues65 outlined the use of closed drainage irrigation following open debridement and omental flap closure in the setting of methicillin resistant S. aureus (MRSA) infections in four patients.
Vacuum-assisted closure for the treatment of open wounds was first described by Argenta and Morykwas5 in 1997. Since then, its use has been expanded to include poststernotomy wounds due to mediastinitis. The benefits of wound vacuum-assisted therapy have been postulated to be multifactorial, but they share the common theme of relying on the associated effects of negative pressure. An increase in local blood flow; decrease in tissue edema and bacterial load; and removal of stagnant fluid, necrotic debris and proteins impeding healing are all believed to promote wound healing. Furthermore, the mechanical effects exerted by the negative pressure is also thought to promote wound closure.52,86
Obdeijn and colleagues106 published one of the first reports of a vacuum-assisted closure of open wounds in three patients with poststernotomy mediastitinitis. In this report all of the patients avoided the need for secondary surgical closure, as closure by accelerated secondary intention was achieved. Subsequent experiences, on a larger scale, have demonstrated that vacuum-assisted treatment of wounds can be an extremely useful adjunct in the management of poststernotomy mediastinitis.28,36,52,86,97,125,126,127 Some of these studies have relied on vacuum-assisted closure exclusively.36,52,86 However, not all investigations have employed vacuum-assisted therapy as the sole form of wound closure, since others have used this technique intentionally as a “bridge” to another form of definitive therapy.36,86 However, even with this intention, vacuum-assisted therapy has, in some cases, precluded the need for flap coverge or sternectomy.28 The depth of infection has been thought to determine which patients will require progression to a second operation for closure.36
Direct comparisons to all forms of conventional therapy with omental or muscle flap closure have shown a significant advantage of vacuum-assisted therapy for wound closure in terms of decreased mortality, increased survival, lower frequencies of local failure, and shorter hospitalizations.52 In contrast, studies of poststernotomy mediastinitis that have not included vacuum-assisted wound closure therapy have described a worse long-term survival. Sjogren and colleagues125,126,127 have demonstrated that with the use of this treatment, long-term survival is no different than that of postoperative coronary artery bypass patients without mediastinitis. Others have shown that vacuum-assisted therapy can facilitate primary closure by accelerating granulation.37 Catarino and colleagues21 have shown that vacuum-assisted therapy compared with closed drainage irrigation alone is associated with no treatment failures and decreased lengths of hospitalization. Others have also demonstrated that there is a shorter length of hospitalization with vacuum-assisted therapy when compared with continuous irrigation.21,37
Perforation of the Aerodigestive Tract
Perforation of the aerodigestive tract can result in mediastinal infection. Typically these infections result from perforation of the esophagus caused by either spontaneous or iatrogenic trauma. Anastomotic leaks following esophagogastrectomy can also lead to acute mediastinitis (SOURCE). However mediastinitis can also result from airway disruptions, as with tracheal injury.53 Disruption of the esophagus in the thoracic cavity permits the egress of oropharyngeal bacteria and gastric contents into the visceral compartment of the mediastinum. Perforation of the cervical esophagus, on the other hand, results in leakage of oropharyngeal secretions and infection of the fascial spaces within the neck, which communicate with the anterior and visceral compartments of the mediastinum. The causes, clinical manifestations, diagnostic interventions, treatment, and outcome of esophageal perforations have been reviewed by Jones and Ginsberg73 as well as by Whyte,138 Wright,144 Engum,44 Bufkin,17 and Iannettoni66 and their colleagues and are beyond the scope of this chapter (see Chapter 146). Management strategies of esophageal perforation including that accompanying mediastinitis are based on four principles:
Eliminate source of soilage by primary repair or diversion away from the esophageal perforation.
Provide thorough and wide mediastinal drainage to control ongoing mediastinal suppuration occurring after primary repair or diversion. In addition, gastrostomy tube decompression should be performed to decrease gastric reflux and mediastinal soilage.
Appropriate antibiotics should be administered to augment host defenses, which must be effective against both gram-positive and gram-negative bacteria and against both aerobic and anaerobic bacteria.
Maintain adequate nutrition. The ultimate goal is to restore alimentary tract continuity, as emphasized by Burnett and associates.18
The details of the techniques of management of esophageal perforations are discussed in Chapter 146.
Descending Necrotizing Mediastinitis
Estrera and associates46 described acute purulent mediastinitis due to oropharyngeal infection as descending necrotizing mediastinitis. This infection remains an uncommon but still lethal form of mediastinitis.
Etiology
Of the reported cases, 60% to 70% are secondary to odontogenic infections.46,88,137 Other common causes have included peritonsillar abscesses0,89 (T et al.), retropharyngeal and parapharyngeal abscesses,27,46 (Freeman et al.) and epiglottitis.23,78 Other less common causes of descending necrotizing mediastinitis include trauma to the neck, including neck or mediastinal surgery; cervical lymphadenitis; and endotracheal intubation, as reported by Guardia and associates,63 Uram and Hauser,133 and Gould and colleagues.61 Alsoub and Chacko4 have listed the many causes of this lethal infection.
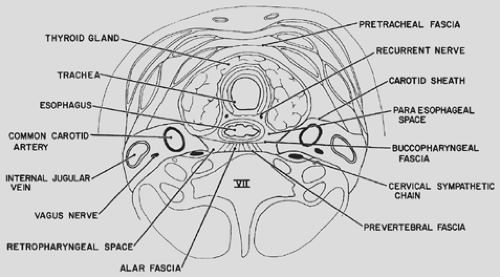
Anatomically, there are three potential planes through which descending necrotizing mediastinitis can progress: (a) pretracheal, (b) perivascular, and (c) prevertebral spaces. The pretracheal space, also referred to as the superficial layer, is just anterior to the trachea. It is bound by the thyroid cartilage superiorly and pericardium and parietal pleura inferiorly at the carina. The perivascular space is bound by the carotid sheath and descends into the mediastinum along with the structures within the carotid sheath. This route of spread results in infections of the middle mediastinum. Finally, the prevertebral space, also referred to as the retropharyngeal space, is bound anteriorly by the posterior aspect of cervical fascia and posteriorly by the alar fascia; it extends inferiorly until these two fascia coalesce at the first thoracic vertebra.60,102,108 Most cases of descending necrotizing mediastinitis are secondary to spread in this last plane and result in involvement of the posterior mediastinum (Fig. 173-1). All these spaces are joined by loose connective tissue, which facilitates direct spread within these planes.99 Gravity and negative pressure during inspiration allow for the descent of the infected and purulent material into the mediastinum and pleura.99 Odontogenic and peritonsillar abscesses may extend to involve the submandibular and parapharyngeal spaces, which, as McCurdy and colleagues93 have noted, readily communicate with all major cervical fascial spaces.
Chow24 and Brook and Frazier15 have recorded that the microbiological features of descending necrotizing mediastinitis are polymicrobial, with aerobes and anaerobes, reflecting the indigenous microflora of the oral cavity. The most common organisms isolated include Prevotella, Peptostreptococcus, Fusobacterium, Veillonella, Actinomyces, oral Streptococcus, Bacteroides, S. aureus, Haemophilus species, and Bacteroides melaninogenicus. Symbiosis between one or more species of gram-negative aerobic bacteria and an anaerobe can result in synergistic necrotizing cellulitis.
Mathieu and associates90 have described predisposing conditions that may favor this infectious process; such conditions include diabetes (13.3%), alcoholism (17.7%), neoplasm (4.4%), and radionecrosis (3.3%). In particular, they found that age >70 years and underlying diabetes were fatal risk factors.
Diagnosis
The criteria used for the diagnosis of descending necrotizing mediastinitis are clearly defined by Estrera and colleagues46 and include (a) clinical evidence of severe oropharyngeal infection, (b) characteristic roentgenographic features of mediastinitis, (c) documentation of necrotizing mediastinal infection at the operation or postmortem or both, and (d) establishment of the relationship between descending necrotizing mediastinitis and the oropharyngeal process.
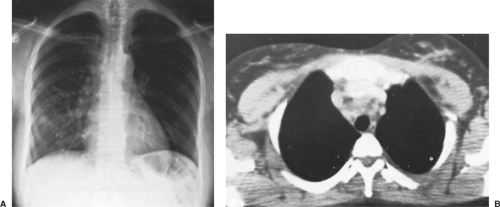
Because this infection progresses rapidly, early diagnosis is essential. Computed tomography (CT) scanning is more reliable
than chest radiography and can provide precise information on the extent of the infection, which will guide the optimal approach used for surgical drainage.
than chest radiography and can provide precise information on the extent of the infection, which will guide the optimal approach used for surgical drainage.
Clinical Manifestations
Descending necrotizing mediastinitis is seen most often in a patient who is under treatment for a deep cervical infection resulting from one of the aforementioned causes. Despite antibiotics and even drainage of the deep cervical space, the infection progresses to involve the mediastinum. Early diagnosis is often difficult because of the vagueness of early symptoms that would indicate mediastinal involvement. Unfortunately the usual delay in diagnosis contributes greatly to the high mortality associated with descending necrotizing mediastinitis.88 Descending necrotizing mediastinitis may occur at any time after cervical infection, manifest by signs and symptoms of sepsis with stiffness, swelling, and neck pain. Cranial nerve deficits, trismus, and stridor have also been described.60 Dysphagia may or may not be present. Mediastinal involvement may occur as soon as 12 hours to as late as 2 weeks, but it is most commonly seen within 48 hours after the onset of deep cervical infection. Diffuse brawny induration of the neck and upper anterior chest wall is seen. Pitting edema and crepitance may be present in the area. Substernal pain, increased dysphagia, cough, and dyspnea may also develop. Pleural and pericardial involvement may occur, since the necrotizing process involves the adjacent spaces. Pleural effusion, nonspecific electrocardiographic changes, and even infection of the retroperitoneal space of the abdomen may develop as the inflammatory process ensues. The capillary leak that occurs with sepsis can further exacerbate dehydration and lead to acute respiratory distress syndrome, cardiac tamponade, and empyema.78,108
Radiographic Features
CT is the diagnostic imaging modality of choice. Estrera and associates46 reported four radiographic features of the neck and chest present in descending necrotizing mediastinitis: (a) widening of the retrocervical space with or without an air–fluid level, (b) anterior displacement of the tracheal air column, (c) mediastinal emphysema, and (d) loss of the normal lordosis in the cervical spine. Also, the superior mediastinal shadow can be widened, and findings of pleural or pericardial involvement may be evident (Fig. 173-2).
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree