Determining accurate left ventricular (LV) function is clinically important. Three-dimensional echocardiography (3DE) achieves better estimation than 2-dimensional echocardiography. However, underestimation of LV volumes has often been reported without a systematic attempt to synthesize these data. This meta-analysis aimed to assess the bias of 3DE in evaluating LV volumes and ejection fraction (EF) and to investigate factors affecting that bias. Studies that compared LV volumes and/or EF between 3DE and magnetic resonance imaging were eligible. Meta-analysis of 95 studies including 3,055 subjects revealed significant underestimation of LV end-systolic volume (−4.7 ml, p <0.0001) and end-diastolic volume (−9.9 ml, p <0.0001), whereas measurement for EF revealed excellent accuracy (−0.13%, p = 0.41). Meta-regression analysis for factors of systematic bias in volumetry revealed that female gender and existence of cardiac disease were associated with more underestimation, whereas use of semiautomatic tracking and matrix-array transducers counteracted the underestimation. In conclusion, by meta-analysis synthesizing many small studies, we found underestimation of LV volumes and factors affecting the systematic bias by 3DE. These data provide a more detailed basis for analyzing and improving the accuracy of 3DE, an indispensable step toward further clinical application in LV assessment.
Accurate quantification of left ventricular (LV) volumes and function is gaining clinical importance. However, LV assessment by 2-dimensional echocardiography is limited by the foreshortened apical views and geometric assumptions. Magnetic resonance imaging (MRI) has been employed as the clinical gold standard, but is time and resource intensive and is sometimes contraindicated. Three-dimensional echocardiography (3DE) has shown better correlation than 2-dimensional echocardiography with MRI measurements in validation studies in vitro and in vivo. In clinical studies, however, underestimation of volumes and ejection fraction (EF) by 3DE has often been reported, creating major discrepancy in this field and hindering further clinical application of 3DE. There has been no systematic attempt to synthesize these data. Therefore, the aims of this study were to determine the existence and extent of systematic bias in LV volumes and EF measured by 3DE compared to MRI and to investigate patient characteristics and soft/hardware factors affecting the systematic bias.
Methods
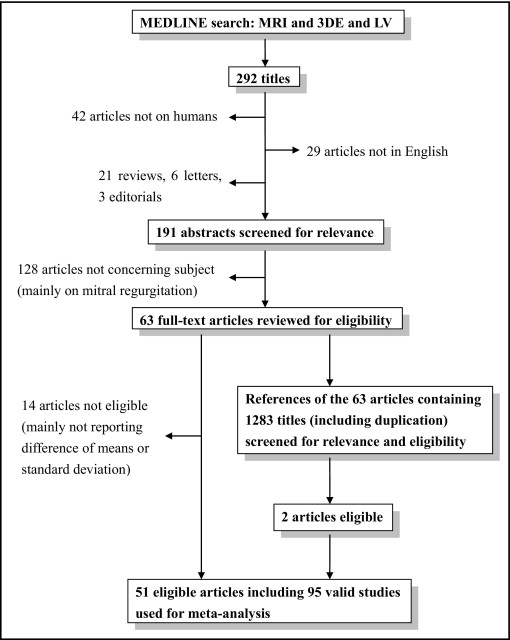
We searched MEDLINE with the Medical Subject Heading function up to June 13, 2010. The key terms used for the literature search were “magnetic resonance imaging,” “left ventricle,” and “3-dimensional echocardiography” and relevant phrases. Articles that included these 3 key phrases were screened by title and abstract for relevance. The search was restricted to human studies published in English. References of relevant articles were also reviewed. Abstracts without subsequent full-text publications, reviews, comments, letters, and literature that were not original articles were excluded ( Figure 1 ).
Studies were considered eligible if the article assessed the difference of LV end-systolic volume, LV end-diastolic volume, and/or LVEF between 3DE and MRI showing mean difference ± SD or if these data could be obtained from the original article. Independent reviewers (Y.J.S. and T.S.) retrieved full texts of the relevant articles to assess eligibility.
Mean difference ± SD of LV end-systolic volume, LV end-diastolic volume, and LVEF between 3DE and MRI were obtained from the text, tables, or graphs. If data were presented only graphically, crude numbers were obtained from the graph. If 1 article included different populations or methods of 3DE validated by MRI, results of each population and method were considered separate studies.
Meta-analysis was performed by random-effects model weighted by inverse variance to evaluate the systematic bias of LV end-systolic volume, LV end-diastolic volume, and LVEF between 3DE and MRI. Heterogeneity was assessed with Cochrane Q test by chi-square test and was quantified with the I 2 test.
Meta-regression analysis with inverse-variance weighted, random-intercept, fixed-slopes model was performed to investigate factors related to bias in LV end-systolic volume, LV end-diastolic volume, and LVEF. The dependent variable was the absolute difference between 3DE and MRI, and independent variables were determined a priori including number of patients in each study, mean patient age, percentage of women, percentage of patients with acquired or congenital cardiac disease, use of matrix-array transducer, use of semiautomatic contour tracking system compared to manual-only tracking, use of contrast agent, use of disk-summation method compared to apical-rotation method, number of manually tracked images, number of included subjects, and publication year. Independence of predictors was evaluated by a variance inflation factor. A maximal variance inflation factor <5 was used as a cutoff for independence.
Continuous values are presented as mean ± SD, and discrete variables are presented as percentages. Review Manager 5.0 (Nordic Cochrane Centre, Cochrane Collaboration, Copenhagen, Denmark) and SPSS 17.0 for Windows (SPSS, Inc., Chicago, Illinois) with Macro Syntax for meta-analysis and meta-regression analysis (D.B. Wilson, meta-analysis macros for SPSS, available at: http://mason.gmu.edu/∼dwilsonb/ma.html ) were used for analysis. A p value <0.05 was considered statistically significant.
Results
In total 292 titles were screened for relevance, of which 51 articles were considered eligible including 95 studies with a total of 3,055 subjects ( Figure 1 ). Most excluded studies were on mitral regurgitation from the search term “MR,” which was intended for MRI. Cross-reference check of relevant studies yielded 2 eligible articles. Table 1 lists characteristics of the included studies.
| Study Number | First Author | Publication Year | Number of Patients (men) | Age (mean ± SD and/or range) | Patient Characteristics | Volumetric Method | Matrix-Array Transducer | Semiautomated Tracking | Contrast Agents | Miscellaneous | Hardware | Software |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1 | Apfel | 1996 | 18 (8) | 11.6 (0.75–42) | PAH | DS | − | − | − | acoustic spatial locator GP 8-3D ⁎ with model 77020AC † | ||
| 2 | Iwase | 1997 | 30 (26) | 58 (22–83) | 7 normal subjects, 23 with “various cardiac diseases” | DS | − | + | − | CFM-800 † with 2.5-MHz annular-array transducer | ||
| 3 | Altmann | 1997 | 12 (8) | 8.6 (0.5–22) | single left ventricle | DS | − | − | − | acoustic spatial locator GP 8-3D ⁎ with model 77020AC † | ||
| 4 | Gopal | 1997 | 30 (13) | 56.6 ± 15.9 (15–87) | 15 with IC, 5 with idiopathic or hypertensive CM, 5 with VHD, 2 with alcoholic CM, 1 with primary PAH, 2 with CHD | DS | − | − | − | acoustic spatial locator (Freepoint 3D § ) with model 77020AC † | ||
| 5 | Buck | 1997 | 23 (14) | 63 ± 99 | chronic stable LV aneurysms | DS | − | − | − | Sonolayer SSH-140A ∥ with 3.75-MHz transducer | Echo-scan, TomTec †† | |
| 6 | Nosir | 1998 | 46 (36) | 51 ± 17 (26–72) | 15 normal subjects, 31 with IHD | DS | − | − | − | Sonolayer SSH-140A ∥ with 3.75-MHz transducer | Echo-scan, TomTec †† | |
| 7 | Mele | 1998 | 20 (NR) | NR | 39 with IHD (32 after MI, 22 with aneurysm), 8 with VHD, 7 with CM | DS | − | − | − | 3.25-MHz annular array transducer of CFM 750 ‡ and 800 ‡ SuperVision | Vingmed system ‡ | |
| 8 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | 24 normal subjects, 17 with abnormal hearts, 14 with EF <55%, 13 with dilated left ventricle, 7 with regional LV systolic dysfunction | DS (2 planes) | − | − | − | Sonos 1500 system ¶ with 2.5-MHz transthoracic transducer | Hewlett-Packard Series 735 † | |
| 9 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (4 planes) | − | − | − | as above | as above | |
| 10 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (6 planes) | − | − | − | as above | as above | |
| 11 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (8 planes) | − | − | − | as above | as above | |
| 12 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (10 planes) | − | − | − | as above | as above | |
| 13 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (12 planes) | − | − | − | as above | as above | |
| 14 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (16 planes) | − | − | − | as above | as above | |
| 15 | Danias | 1998 | 41 (32) | 39 ± 19 (24–77) | as above | DS (20 planes) | − | − | − | as above | as above | |
| 16 | Nosir | 1999 | 15 (15) | 52 ± 16.5 | normal subjects | DS | − | − | − | A | Sonolayer SSH-140A ∥ | Echo-scan †† |
| 17 | Nosir | 1999 | 15 (15) | 52 ± 16.5 | normal subjects | DS | − | − | − | B | as above | as above |
| 18 | Nosir | 1999 | 25 (25) | 52 ± 16.5 | IC | DS | − | − | − | A | as above | as above |
| 19 | Nosir | 1999 | 25 (25) | 52 ± 16.5 | IC | DS | − | − | − | B | as above | as above |
| 20 | Chuang | 1999 | 8 (NR) | NR | NR | NR | − | − | − | Sonos 1500 or 2500 ¶ using 2.5-MHz phased-array probe | custom scanner software ¶ | |
| 21 | Chuang | 1999 | 20 (16) | 44 ± 16 (24–76) | 7 with CAD and regional WMA, 2 with MV disease/LVD, 2 with impaired LV function, 1 with PDA/membranous VSD/DC, 1 with postpartum DC | AR | − | − | − | as above | as above | |
| 22 | Shiota | 1999 | 19 (NR) | NR | 6 with aortic disease, 13 with CM | DS | − | − | − | 3D ultrasound system # with 2.5-MHz phased-array transducer | software equipped with 3D system # | |
| 23 | Qin | 2000 | 32 (22) | 54 ± 11 | 6 with right ventricular dysplasia, 9 with aortic regurgitation, 9 with MR, 4 with DC, 12 with IC | AR (2 planes) | NR | − | − | 3D ultrasound system # with 2.5-MHz phased-array transducer | 3D EchoTech †† | |
| 24 | Qin | 2000 | 32 (22) | 54 ± 11 | as above | AR (4 planes) | NR | − | − | as above | as above | |
| 25 | Qin | 2000 | 32 (22) | 54 ± 11 | as above | AR (6 planes) | NR | − | − | as above | as above | |
| 26 | Qin | 2000 | 32 (22) | 54 ± 11 | as above | AR (9 planes) | NR | − | − | as above | as above | |
| 27 | Qin | 2000 | 32 (22) | 54 ± 11 | as above | DS | NR | − | − | as above | as above | |
| 28 | Nosir | 2000 | 21 (15) | 49 ± 16 (26–66) | 5 healthy volunteers, 12 with ischemic segmental WMA, 4 with global hypokinesis from DC | AR | − | − | − | 2° | Sonolayer SSH-140A ∥ (3.75 MHz) | Echo-scan, TomTec †† |
| 29 | Nosir | 2000 | 21 (15) | 49 ± 16 (26–66) | as above | AR | − | − | − | 8° | Sonolayer SSH-140A ∥ (3.75 MHz) | Echo-scan, TomTec †† |
| 30 | Nosir | 2000 | 21 (15) | 49 ± 16 (26–66) | as above | AR | − | − | − | 16° | Sonolayer SSH-140A ∥ (3.75 MHz) | Echo-scan, TomTec †† |
| 31 | Hibberd | 2000 | 25 (18) | 23–76 | 12 healthy volunteers, 5 with IC with focal WMA, 8 with nonischemic DC | NR | − | − | − | Sonos 1500/2500 with 2.5-MHz phased-array transducer | custom software ¶ | |
| 32 | Kim | 2001 | 10 (5) | 25.2 ± 2.44 | healthy volunteers | AR (6 planes) | − | + | − | phased-array transducer (Vingmed System Five ‡ ) | EchoPac-3D ‡ | |
| 33 | Kim | 2001 | 10 (5) | 25.2 ± 2.44 | healthy volunteers | AR (6 planes) | − | + | − | with harmonic | as above | as above |
| 34 | Kim | 2001 | 18 (NR) | 59.9 ± 11.6 | 21 with IC, 1 with DC | AR (6 planes) | − | + | − | as above | as above | |
| 35 | Kim | 2001 | 18 (NR) | 59.9 ± 11.6 | 21 with IC, 1 with DC | AR (6 planes) | − | + | − | with harmonic | as above | as above |
| 36 | Poutanen | 2001 | 30 (15) | 10.6 ± 1.4 (8.4–13.2) | healthy volunteers | DS | − | + | − | GE Vingmed System Five ‡ ultrasound scanner (3.5 or 5 MHz) | ||
| 37 | Lee | 2001 | 25 (17) | 50.8 ± 15.4 | “various cardiac disorders” | AR (7 planes) | + | − | − | Volumetrics system # with a 2.5-MHz matrix-array transducer | ||
| 38 | Mannaerts | 2003 | 27 (21) | 50.2 ± 19.5 | 7 normal, 16 after MI (6 had apical aneurysm), 1 with HC, 2 with moderate aortic regurgitation, 1 with severe MR | AR (2 planes) | − | − | − | breath-hold | ATL HDI 5000 ¶ | Echo-scan 4.2, TomTec †† |
| 39 | Mannaerts | 2003 | 27 (21) | 50.2 ± 19.5 | as above | AR (2 planes) | − | − | − | free-breath | as above | as above |
| 40 | Kühl | 2004 | 24 (NR) | NR | 10 without apparent heart disease, 4 with DC, 10 with IC | AR (8 planes) | + | + | − | Sonos 7500 ¶ with X4 transducer | CardioView RT ¶ | |
| 41 | Jenkins | 2004 | 50 (41) | 64 ± 8 | 7 normal, 41 with regional WMA, 7 with global WMA due to hypertension | AR (12 planes) | + | + | − | Sonos 7500 ¶ with X4 transducer | 4D analysis, Tomtec †† | |
| 42 | Müller | 2004 | 15 (12) | 62 ± 8 | 6 with anterior MI, 4 with posterior MI | AR (8 planes) | − | − | − | Sequoia C 256 ⁎⁎ | Tomtec †† | |
| 43 | Müller | 2004 | 15 (12) | 62 ± 8 | 6 with anterior MI, 4 with posterior MI | DS | − | − | − | as above | as above | |
| 44 | Müller | 2004 | 12 (8) | 46 ± 19 | normal subjects | AR (8 planes) | − | − | − | as above | as above | |
| 45 | Müller | 2004 | 12 (8) | 46 ± 19 | normal subjects | DS | − | − | − | as above | as above | |
| 46 | Gutiérrez-Chico | 2005 | 35 (28) | 60.6 ± 16.6 (31–87) | after MI | AR (2 planes) | + | − | − | Sonos 7500 ¶ with X4 transducer | 4D CardioView RT 1.0 Build 983 ¶ | |
| 47 | Gutiérrez-Chico | 2005 | 35 (28) | 60.6 ± 16.6 (31–87) | after MI | AR (4 planes) | + | − | − | as above | as above | |
| 48 | Gutiérrez-Chico | 2005 | 35 (28) | 60.6 ± 16.6 (31–87) | after MI | AR (8 planes) | + | − | − | as above | as above | |
| 49 | Bu | 2005 | 19 (10) | 10.6 ± 2.8 | normal subjects | AR (8 planes) | + | − | − | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 4D CardioView RT 1.2 ¶ | |
| 50 | Corsi | 2005 | 30 (19) | 58 ± 19 | 6 normal volunteers, 11 with CAD, 9 with DC, 2 with VHD, 1 with aortic coarctation, 1 with right atrial mass | + | + | − | Sonos 7500 ¶ with X4 transducer | Matlab (MathWorks, Inc., Matick, Massachusetts) | ||
| 51 | Caiani | 2005 | 46 (27) | 53 ± 17 | 7 normal subjects, 9 with DC, 15 with CAD, 4 with LVH, 3 with myocarditis, 8 with VHD | AR (4 planes) | + | + | − | without contrast | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 3DQ–Qlab ¶ |
| 52 | Caiani | 2005 | 14 (NR) | NR | NR | AR (4 planes) | + | + | + | with contrast | as above | as above |
| 53 | Angelini | 2005 | 10 (NR) | 33 (6–63) | PAH | DS | NR | − | − | manual tracing | not specified | 3D EchoTech †† |
| 54 | Angelini | 2005 | 10 (NR) | 33 (6–63) | PAH | DS | NR | NR | − | 3D-deformable model | as above | as above |
| 55 | Caiani | 2005 | 20 (10) | 58 ± 17 | 7 with CAD, 9 with DC, 2 with HC, 1 with PAH, 1 with normal left ventricle | AR (4 planes) | + | + | + | continuous imaging | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 3DQ–Qlab ¶ |
| 56 | Caiani | 2005 | 20 (10) | 58 ± 17 | as above | AR (4 planes) | + | + | + | dual triggering | as above | as above |
| 57 | van den Bosch | 2006 | 29 (19) | 31 ± 9 (19–51) | distorted LV geometry from congenital heart malformation | AR (8 planes) | + | − | − | Sonos 7500 ¶ with X4 transducer | 4D LV analysis 1.2 and EchoView 5.2 †† | |
| 58 | Jacobs | 2006 | 50 (27) | 58 ± 19 | 24 with CAD, 18 with DC, 4 with VHD, 2 with aortic coarctation, 2 with right atrial mass | AR | + | + | − | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 3DQ Advanced ¶ | |
| 59 | Chan | 2006 | 30 (23) | 62 ± 9 | after MI | AR (12 planes) | + | + | − | Sonos 7500 ¶ | 4D analysis, Tomtec †† | |
| 60 | De Castro | 2006 | 30 (30) | NR | 18 athletes, 12 sedentary men | AR (8 planes) | + | NR | − | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 4D Cardio View RT, TomTec †† | |
| 61 | Krenning | 2006 | 17 (17) | 52 (29–74) | after MI | AR (7 planes) | − | + | − | Vingmed Vivid 5 ‡ with 64-element array transducer (3 MHz) | TomTec 4D LV analysis †† | |
| 62 | Sugeng | 2006 | 31 (17) | 60 ± 15 | 9 with normal hearts, 14 with CAD, 7 with dilated ventricles, 1 with apical HC | AR (6 planes) | + | + | − | Sonos 7500 ¶ with X4 transducer in harmonic mode | TomTec 4D LV analysis †† | |
| 63 | Nikitin | 2006 | 64 (51) | 65 ± 12 | 10 normal subjects, 54 with cardiac disease | AR (8 planes) | + | + | − | Sonos 7500 ¶ with X4 transducer | TomTec 4D LV analysis †† | |
| 64 | Jenkins | 2006 | 110 (94) | 63 ± 10 | LV dysfunction, 98 from regional WMA and 12 from global WMA | AR (12 planes) | + | + | − | off-line | iE33 ¶ with 4× matrix-array transducer | TomTec †† |
| 65 | Jenkins | 2006 | 110 (94) | 63 ± 10 | as above | automatic detection | + | + | − | on-line | as above | Qlab ¶ |
| 66 | Qi | 2007 | 58 (40) | 59 (21–83) | 14 normals, 23 with CAD, 7 with DC, 3 with ASD or VSD, 3 with VHD | AR (8 planes) | + | − | − | iE33 ¶ with a 4× matrix-array transducer | TomTec †† Echoview 5.2 | |
| 67 | Jenkins | 2007 | 30 (22) | 66 ± 7 | after MI | AR (12 planes) | + | + | − | Matrix | Sonos 7500 ¶ with X4 transducer | TomTec †† 4D LV analysis |
| 68 | Jenkins | 2007 | 30 (22) | 66 ± 7 | after MI | AR (12 planes) | − | + | − | reconstruction | as above | as above |
| 69 | Soliman | 2007 | 53 (28) | 56 ± 12 | 9 with IC, 11 with noncompaction, 20 with HC, 13 with idiopathic DC | AR (8 planes) | + | + | − | multiplane interpolation | Sonos 7500 ¶ with X4 transducer | 4D LV analysis 1.2/EchoView 5.2 †† |
| 70 | Soliman | 2007 | 41 (28) | 56 ± 11 | as above | automated | + | + | − | full-volume reconstruction | as above | TomTec 4D LV analysis 2.0 †† |
| 71 | Soliman | 2007 | 41 (28) | 56 ± 11 | as above | AR (2 planes) | + | + | − | Qlab | as above | off-line QLAB 4.2, 3DQ Advanced ¶ |
| 72 | Krenning | 2007 | 39 (34) | 58 ± 15 (24–79) | 28 after MI, 10 with CM, 1 with myocarditis | AR (8 planes) | + | − | − | without contrast | X4 transducer, Sonos 7500 ¶ (n = 18) or IE33 ¶ with X3-1 transducer (n = 21) | TomTec EchoView 5.2 †† |
| 73 | Krenning | 2007 | 39 (34) | 58 ± 15 (24–79) | 28 after MI, 10 with CM, 1 with myocarditis | AR (8 planes) | + | − | + | with contrast | as above | as above |
| 74 | Riehle | 2008 | 12 (7) | 15.9 (1–33) | 5 with repaired ToF, 2 PS s/p valvotomy, 2 with aortic coarctation, 1 with midaortic stenosis, 1 with AS, 1 with anomalous left coronary artery | AR (2 planes) | + | + | − | iE33 ¶ with 1- to 3-MHz X3-1 matrix-array transducer | 3DQ-LAB ¶ | |
| 75 | Soriano | 2008 | 27 (NR) | 7 months | functional single ventricle | NR | + | − | − | Sonos 7500 ¶ with X4 transducer (2–4 Hz) | 4D EchoView, TomTec †† | |
| 76 | Lu | 2008 | 20 (11) | 10.6 ± 2.8 (6–18) | 19 healthy volunteers, 1 with secundum ASD | automated | + | + | − | matrix-array transducer (X4, 2–4 MHz) | QLAB-3DQ ¶ | |
| 77 | Lu | 2008 | 20 (11) | 10.6 ± 2.8 (6–18) | 19 healthy volunteers, 1 with secundum ASD | AR (4 planes) | + | + | − | as above | 4D EchoView 5.4, TomTec †† | |
| 78 | Lu | 2008 | 20 (11) | 10.6 ± 2.8 (6–18) | 19 healthy volunteers, 1 with secundum ASD | AR (8 planes) | + | + | − | as above | as above | |
| 79 | Mor-Avi | 2008 | 92 (69) | 57 ± 16 | “patients” | AR | + | − | − | iE33 ¶ and an X3-1 matrix-array transducer | QLAB-3DQ Advanced ¶ | |
| 80 | Bicudo | 2008 | 20 (13) | 32 ± 14 | HC | NR | + | − | − | Sonos 7500 ¶ with X4 transducer | Q-Lab 4.0 and 4.2.1 ¶ | |
| 81 | Pouleur | 2008 | 83 (67) | 54 ± 19 (7–85) | 20 normal subjects, 20 with aortic valve disease, 10 with severe MR, 33 after MI | NR | + | + | − | Sonos 7500 ¶ or IE33 systems with matrix-array transducer | Qlab ¶ | |
| 82 | Soliman | 2008 | 17 (12) | 53 ± 15 | 7 normal subjects, 10 with IC, 7 with idiopathic DC | AR | + | + | − | iE33 ¶ with an X3-1 transducer | QLAB-3DQ Advanced 6.0 ¶ | |
| 83 | Chukwu | 2008 | 35 (22) | 55.2 ± 15.4 | normal subjects | AR (2 planes) | + | + | − | Sonos 7500 ¶ with X4 transducer | 4D Echoview 5.3, TomTec †† | |
| 84 | Chukwu | 2008 | 35 (22) | 55.2 ± 15.4 | normal subjects | AR (4 planes) | + | + | − | as above | as above | |
| 85 | Chukwu | 2008 | 35 (22) | 55.2 ± 15.4 | normal subjects | AR (6 planes) | + | + | − | as above | as above | |
| 86 | Chukwu | 2008 | 35 (22) | 55.2 ± 15.4 | normal subjects | AR (8 planes) | + | + | − | as above | as above | |
| 87 | Chukwu | 2008 | 35 (22) | 55.2 ± 15.4 | normal subjects | 3D automated | + | + | − | as above | 4D LV analysis 2.0, TomTec †† | |
| 88 | Chukwu | 2008 | 35 (22) | 65.8 ± 5.5 | after MI | AR (2 planes) | + | + | − | as above | as above | |
| 89 | Chukwu | 2008 | 35 (22) | 65.8 ± 5.5 | after MI | AR (4 planes) | + | + | − | as above | as above | |
| 90 | Chukwu | 2008 | 35 (22) | 65.8 ± 5.5 | after MI | AR (6 planes) | + | + | − | as above | as above | |
| 91 | Chukwu | 2008 | 35 (22) | 65.8 ± 5.5 | after MI | AR (8 planes) | + | + | − | as above | as above | |
| 92 | Chukwu | 2008 | 35 (22) | 65.8 ± 5.5 | after MI | 3D automated | + | + | − | as above | 4D LV analysis 2.0, TomTec †† | |
| 93 | Jenkins | 2009 | 50 (46) | 63 ± 10 | after MI | AR (12 planes) | + | + | − | without contrast | Sonos 7500 ¶ with X4 transducer | 4D LV analysis 2.0, TomTec †† |
| 94 | Jenkins | 2009 | 50 (46) | 63 ± 10 | after MI | AR (12 planes) | + | + | + | with contrast | as above | as above |
| 95 | Nesser | 2009 | 43 (28) | 59 ± 16 | 9 normal subjects, 17 with CAD (6 after MI), 10 with DC, 4 with myocarditis, 3 with VHD | AR (2 planes) | + | + | − | Artida 4D with matrix-array transducer (PST-25SX) ∥ | 3D wall motion tracking software |
Stay updated, free articles. Join our Telegram channel

Full access? Get Clinical Tree


