The purpose of this study was to evaluate the influence of a home-based walking program on erectile function and the relation between functional capacity and erectile dysfunction (ED) in patients with recent myocardial infarctions. Patients with acute myocardial infarctions deemed to be at low cardiovascular risk were randomized into 2 groups: (1) a home-based walking group (n = 41), instructed to participate in a progressive outdoor walking program, and (2) a control group (n = 45), receiving usual care. Functional capacity was determined by the 6-minute walk test and evaluation of sexual function by the International Index of Erectile Function questionnaire; the 2 tests were performed at hospital discharge and 30 days later. In the overall cohort, 84% of patients reported previous ED at hospital discharge. After 30 days, ED had increased by 9% in the control group in relation to baseline (p = 0.08). However, the home-based walking group had a significant decrease of 71% in reported ED (p <0.0001). The 6-minute walk distance was statistically significant higher in the home-based walking group compared with the control group (p = 0.01). There was a significant negative correlation between 6-minute walk distance and ED 30 days after hospital discharge (r = −0.71, p <0.01). In conclusion, an unsupervised home-based progressive walking program led to significant improvements in functional capacity in men at low cardiovascular risk after recent acute myocardial infarctions. In addition, this intervention demonstrated a link between functional capacity and exercise training and erectile function improvement.
Few studies have assessed erectile dysfunction (ED) in men participating in exercise-based cardiac rehabilitation program after acute myocardial infarctions (AMIs). This is particularly the case for home-based exercise programs implemented in this population. We hypothesized a link between ED and functional capacity as well as a beneficial role for exercise training as a nonpharmacologic therapeutic strategy to alleviate ED. Therefore, the purpose of this study was to evaluate (1) the influence of a home-based walking program on erectile function and (2) the relation between functional capacity and ED in patients with recent AMIs.
Methods
This study was performed at the São Paulo Hospital, Federal University of São Paulo, from February 2011 to December 2013. The institutional ethics committee approved this randomized controlled study. Before study inclusion, all patients were informed about the study, and a signed consent form was obtained from each subject.
The subjects were prospectively selected from patients with AMIs within the first 12 hours of intensive care unit admission who underwent successful percutaneous coronary intervention with clinical signs of reperfusion. The diagnosis of AMI was confirmed by serum cardiac enzyme levels, with or without ST-segment elevation. The ages of subjects included in this study ranged from 40 to 70 years, and all had stable, long-term relationships with the same sexual partner. Female patients as well as those with cardiogenic shock or cardiac arrest, recurrent pain, diagnosed neuromuscular diseases, hemodynamic instability, use of mechanical ventilation, severe cardiac arrhythmias, previous AMI, inability to perform pulmonary function tests, previous prostate surgery, and/or exclusive treatment with chemical reperfusion were excluded. Patients with chronic lung disease confirmed by pulmonary function testing according to American Thoracic Society standards were also excluded.
The patients underwent a supervised early mobilization exercise program, 2 times a day, beginning 12 hours after the AMI, according to American Heart Association recommendations. Initial energy expenditure during exercise training was estimated at 2 METs, with an incremental progressive increase to an estimated intensity of 4 METs. During the exercise program, patients were instructed to maintain a Borg Rating of Perceived Exertion Scale (RPE) score of 4 or 5 (the scale ranges from 0 to 10), corresponding to mild to moderate exercise intensity, according to current recommendations. The supervised exercise program performed during the inpatient phase was terminated if there were signs of exercise intolerance and low cardiac output (cyanosis, pallor, nausea).
Upon hospital discharge, patients were classified in relation to cardiovascular risk according to American Association of Cardiovascular and Pulmonary Rehabilitation guidelines. In this study, only patients at low cardiovascular risk were prospectively randomized into 2 groups by a computer system (numbered, sealed, and opaque envelopes were used to maintain confidentiality): (1) a home-based walking group (n = 41), instructed to participate in a progressive outdoor walking program, or (2) a control group (n = 45), receiving usual care.
In the 2 groups the patients underwent an educational process that included general education about their disease, treatment, importance of continuing to exercise, and nutritional recommendations. Moreover, before hospital discharge, patients received standardized information about the resumption of sexual activity. In addition, patients received a brochure with detailed instructions, in an attempt to improve adherence.
The subjects in the home-based walking group were instructed to perform a home-based, unsupervised, outdoor progressive walking program, 4 times a week, for the month after hospital discharge. The exercise program consisted of 3 phases: (1) a warmup period of 5 minutes; (2) an endurance training period, progressively increasing walking time from 20 minutes during the first week, 25 minutes during the second week, 30 to 35 minutes during the third week, to 35 to 40 minutes during the last week; and (3) a cool-down period of 5 minutes. During the exercise program, patients were instructed to maintain an RPE score of 4 or 5, corresponding to mild to moderate exercise intensity, according to current recommendations. The control group, which was not subjected to the home-based walking program, received general health information on the need for a healthy lifestyle, including guidance on the importance of continuing to perform physical activity initiated during inpatient care. Regardless of group assignment, all patients were instructed to stop exercising if they rated their RPE score ≥6 and/or, through a self-assessed talk test, when they observed that they were unable to talk during exercise. Moreover, subjects were trained to use the RPE during the inpatient phase and instructed to exercise at home on a level surface with comfortable clothes and shoes and also not to run during exercise.
Once a week, patients in the home-based walking group were contacted by telephone, encouraging the continuation of the proposed exercises and, for patients in the usual-care group, emphasizing the importance of maintaining activities of daily living. All patients were prescribed β blockers, clopidogrel (75 mg/day), acetylsalicylic acid (100 mg/day), statins, and angiotensin-converting enzyme inhibitors and also were encouraged to maintain their prescribed medications.
Erectile function was assessed by the International Index of Erectile Function (IIEF) questionnaire, validated for the Brazilian population and administered this study 2 times, on the day of discharge and 30 days afterward, by the same evaluator blinded to randomization. ED was defined as a score <25 on the 30-point scale, consistent with previous studies.
Submaximal functional capacity was determined by the 6-minute walk test, at discharge and 30 days afterward, by the same evaluator blinded to randomization, according to the guidelines of the American Thoracic Society. The equation proposed by Iwama et al was used to predict 6-minute walk distance for all patients.
On the basis of the results of previous studies, the sample size was calculated for detecting a ≥15% difference in 6-minute walk distance with power of 90% and α risk of 5% (p <0.05). For this study, the sample size needed to achieve the calculated study power was 42 patients per group. The paired Student’s t test was used for intragroup comparisons. When variables were compared between groups, we used the unpaired Student’s t test and the Mann-Whitney test when necessary. Categorical variables were analyzed by Pearson’s χ 2 test. Pearson’s correlation coefficient was used to evaluate associations of interest. A p value <0.05 was considered statistically significant. Statistical analyses were performed using GraphPad Prism version 3.0 (GraphPad Software, Inc., San Diego, California).
Results
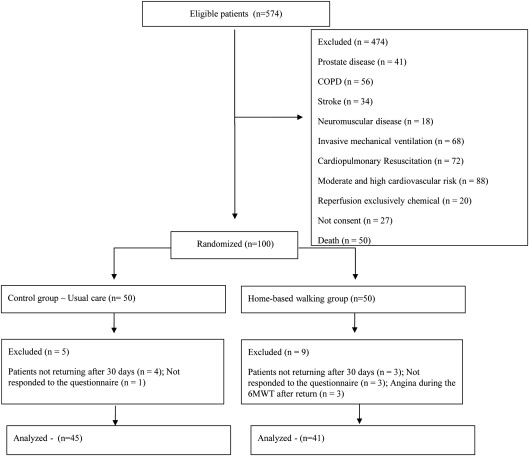
During the study period, 574 patients were assessed for eligibility, and from that sample, 100 were allocated to 2 groups, with 86 ultimately accomplishing the protocol ( Figure 1 ). The groups were homogenous, and no statistical difference was found with respect to key baseline characteristics, as listed in Table 1 .
| Variable | Control group (N = 45) | Home-based walking group (N = 41) | p |
|---|---|---|---|
| Age (years) | 57±9 | 59± 10 | 0.22 |
| Body mass index (kg/m 2 ) | 25± 5 | 26± 4 | 0.21 |
| Waist-hip ratio (cm) | 1.0 ± 0.1 | 1.0 ± 0.1 | 0.36 |
| Ejection fraction of the left ventricle | 52 ± 9% | 50 ± 10% | 0.21 |
| Hypertension | 26 (58%) | 26 (63%) | 0.29 |
| Diabetes mellitus | 16 (35%) | 12 (29%) | 0.26 |
| Smoker | 31 (68%) | 30 (73%) | 0.33 |
| Dyslipidemia | 13 (28%) | 13 (31%) | 0.38 |
| Forced vital capacity (L) | 3.2 ± 0.6 | 3.6 ± 0.4 | 0.14 |
| Percent predicted | 98 ± 12% | 97 ± 11% | |
| Forced expiratory volume in 1 second (L) | 2.8 ± 0.4 | 2.9 ±0.5 | 0.19 |
| Percent predicted | 97 ±14% | 95 ± 10% | |
| Distance covered in 6-minute walk test (meters) | 457± 73 | 460 ± 106 | 0.45 |
| Percent predicted | 79 ± 12% | 81 ± 17% | |
| Medication | |||
| Antihypertensive | 25 (55%) | 26 (63%) | 0.22 |
| Diuretic | 4(8%) | 5(12%) | 0.30 |
| Classification of erectile dysfunction, n | |||
| Severe | 18 (40%) | 15 (36%) | 0.37 |
| Moderate | 13 (29%) | 11 (27%) | 0.41 |
| Mild to moderate | 5 (11%) | 6 (15%) | 0.31 |
| Mild | 2 (4%) | 2 (5%) | 0.46 |
| No erectile dysfunction | 7 (16%) | 7 (17%) | 0.42 |
| Total with erectile dysfunction, n | 38 (84%) | 34 (83%) | 0.42 |
| Days of hospitalization | 5.0 ±1.2 | 5.6 ±1.5 | 0.15 |
In the overall cohort, 72 subjects (84%) reported previous ED on the IIEF questionnaire at hospital discharge. At 30 days after discharge, ED prevalence had increased by 9% in the control group compared with baseline, which trended toward statistical significance (from 84% to 93%, p = 0.08), whereas the home-based walking group had a significant 71% decrease (from 83% to 12%, p <0.0001). This domain’s scores and respective percentage and comparison between groups 30 days after hospital discharge are listed in Table 2 . The 2 groups demonstrated significant increases in 6-minute walk distance 30 days after discharge compared with baseline (p <0.05). However, when comparing the groups, the control group showed an increase of 6.6% (30 m), whereas the home-based walking group exhibited a significantly higher increase of 16.5% (76 m) (p = 0.01). A significant negative correlation was observed between 6-minute walk distance and ED 30 days after hospital discharge (r = −0.71, p <0.01).



